Abstract
The authors determined current health status of patients who had been included in a long-term survivorship analysis of a lumbar dynamic stabilizer. Among 133 living patients, 107 (average age at surgery, 44.2 ± 9.9 years) completed health questionnaires. All patients had initially been scheduled for decompression and fusion for canal stenosis, herniated disc, or both. In 20 patients, the implant was removed, and fusion was performed. The other 87 still had the dynamic stabilizer. Satisfaction, Oswestry disability index, visual analog scales for back and leg pain, short-form (SF-36) quality-of-life physical composite score, physical function, and social function were significantly better (p ≤ 0.05) in the patients who still had the dynamic stabilization device. SF-36 scores of the fused subgroup were no worse than those reported elsewhere in patients who had primary pedicle-screw enhanced lumbar fusion. This anatomy-sparing device provided a good 13-year clinical outcome and obviated arthrodesis in 80% of patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Interspinous spacers combined with tension bands around the spinous processes for lumbar segmental stabilization were developed in the early 1980s [23]. The initial version of this system was upgraded to the current Wallis dynamic stabilization device in 2001 [24]. Indications for these devices have been the need to stabilize symptomatic degenerative lumbar spine segments, imparting rigidity while preserving intervertebral mobility. One of the goals of restoring stiffness to unstable degenerate segments is to recreate mechanical conditions that could permit consolidation of altered intervertebral soft tissues [9, 16]. Above all, dynamic stabilization is intended to relieve low back pain related to instability and thus delay the need for irreversible, more invasive surgical management [25].
The system’s long-term safety and efficacy has recently been confirmed in a 14-year retrospective study [25]. The latter study was an actuarial survivorship analysis of the first-generation device showing that it effectively obviated the need for arthrodesis or total disc replacement (TDR) in over 80% of patients throughout the follow-up period, which ranged from 9 to 17 years.
The purpose of the present study was to evaluate the long-term clinical results of the first-generation lumbar dynamic stabilization system.
Materials and methods
Implants
The implant (Figs. 1 and 2) included a double-braided woven polyester (Dacron) cord fixed to a titanium spacer and, when more than one intervertebral segment was treated, additional interspinous spacers made of polyacetal (Hostaform) were used. The implants created a semi-constrained system designed to stabilize the intervertebral axis of extension and flexion and reduce the mobility of the instrumented segment. The spacers placed between the spinous processes were intended to produce an unloading effect, reducing pressure in the facet joints and posterior portion of the intervertebral endplates in lordosis. There was a radiodense marker inside the cord throughout its length. The polyacetal spacers were radiolucent.
Surgical technique
After the supraspinous ligament was detached, the interspinous space was trimmed with a gouge and a high-speed drill to create a trapezoid opening so as to prevent the posterior displacement of the spacer. When instrumenting the L5-S1 space, if the first sacral spinous process was atrophic, a groove for the cord was cut in the lamina with a high-speed drill, or the sacral crest was perforated transversely to thread the cord through it. The spacers were chosen to fit the trimmed interspinous space and avoid kyphosis of the instrumented segment. The lordosis of the lumbar column was verified using an image intensifier before final fixation of the implant.
The first spacer (the only spacer if a single level was instrumented) was made of titanium, delivered attached to a lone woven polyester cord. The surgeon threaded the cord around the spinous processes and through the spacers in figure-8 fashion. When tension had been applied throughout all levels, we blocked the extremity of the cord by firmly lodging a taper beside it in the metal spacer. The supraspinous ligament was reattached to each spinous process using separate transfixing sutures.
Postoperative care
Patients were encouraged to begin walking the first day after the intervention and wore a lumbar orthosis for 3 weeks. Isometric exercises were prescribed to maintain the muscle tone of the trunk. After discontinuation of the lumbar orthosis, rehabilitation was pursued with emphasis on tightening the lower back muscles. Patients were generally seen between 1 and 2 months after the operation then again after 6 months if they lived within a 50-mile radius of our spinal unit. At discharge from the unit and at follow-up visits, we urged them and their general practitioner to consult us if any low back or leg problem persisted or subsequently developed.
Patients
We recently published a paper on the actuarial survivorship of 142 first-generation Wallis devices [25]. The patients were requested to participate in a long-term retrospective clinical survey when they were contacted by telephone. Two additional patients who had not been interviewed by telephone presented spontaneously for a follow-up visit, during which they also completed the clinical questionnaire, leading to a total of 144 patients.
Eleven of the 144 patients were deceased when the clinical survey was performed, leaving 133 available patients. Among them, there were two patients who refused to respond to the questionnaire, 24 who agreed to respond but failed to follow through, and 107 (80%) who completed the questionnaire. There were no differences in those followed and those lost to follow-up evaluation in terms of gender breakdown (p = 0.4), age at operation (p = 0.3), body mass index (BMI; p = 0.5), number of levels operated (p = 0.16), and indications (p = 0.4).
Outcome measures
The follow-up questionnaire contained questions regarding patient satisfaction, an Oswestry disability index (ODI) [3], visual analog scales (VAS) [11] for self-reported back pain and leg pain, and a short-form 36 (SF-36) quality-of-life survey [14, 18].
Statistical analysis
Comparison of patient subgroups was performed using the Chi2 test for patient satisfaction, Student’s t test for ODI and VAS findings, and the non-parametric Mann–Whitney U test for the SF-36 values. A p value of 0.05 was considered to be significant.
Results
Among the 107 patients who responded to the questionnaire, review of hospital charts indicated that the index operation was performed for isolated canal stenosis (n = 39), canal stenosis and herniated disc (n = 22), isolated primary herniated disc (n = 13), isolated recurrent disc (n = 21), and other diagnoses (n = 4). The information on the indication for surgery was missing from eight of the hospital charts.
The majority of the 107 patients who completed the questionnaires were male (73%), and the average age at the time of surgery was 44.2 ± 9.9 years (range, 21–66 years). The average length of follow-up was 13.5 ± 2.7 years (range, 8.3–19.6 years).
Twenty-three of these patients had a subsequent lumbar operation. In 20 of these patients, the implant or implants were removed, and fusion was performed. The purpose of this paper was being able to investigate the long-term clinical outcome of patients with dynamic stabilization; the patients from whom the implant was subsequently removed and who had arthrodesis (n = 20/107) were analyzed separately. The other subgroup (n = 87/107) included the 84 patients who had never been reoperated and the three patients who were reoperated at the index or adjacent levels but still had a functional implant. There were no differences in these two subgroups in terms of gender breakdown (p = 0.2), age at operation (p = 0.3), BMI (p = 0.8), number of levels operated (p = 0.9), or indications (p = 0.9). Likewise, the percentages of response to the survey were similar, 81% (n = 87) of the 107 living patients who still had the implant versus 77% (n = 20) among the 26 living patients who had undergone fusion after removal of the implant. Follow-up after the index operation of the patients who still had the implant was 13.2 ± 2.6 years. The patients subsequently revised to fusion, responded to the questionnaire 15.1 ± 2.7 years after the index operation and 10.6 ± 4.8 years after the revision procedure.
Long-term clinical outcome
The satisfaction of the patients who still had the dynamic stabilization was high, with 95% reporting that they were either very satisfied or satisfied with their surgery, and 91% indicating that they would certainly or probably have the procedure if they were confronted with the same choice. The details of patient satisfaction are provided in Table 1. In both questions used to assess patient satisfaction, there was a significant difference between the subgroup of patients who still had the dynamic stabilizer at follow-up and the subgroup of patients in whom the device had been removed and the segments stabilized by fusion.
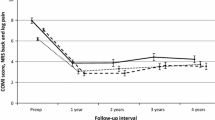
The patients’ report of disability in terms of the ODI was relatively low as can be seen in Table 2. The self-reported pain levels in the low back and legs are also shown in Table 2. The disability scores, low back pain and leg pain of the patients who still had the implant were roughly half of the corresponding values of the patients who had a fusion procedure to replace the implant. Regarding the pain scores, the difference between the two subgroups was highly significant.
Regarding the reported SF-36 quality-of-life assessment, the average value of all eight parameters as well as the average calculated physical composite score (PCS) and mental composite score were higher in the subgroup of patients who still had the first-generation Wallis implant. This difference was close to significant for bodily pain (p = 0.07) and role-physical (p = 0.06) and reached significance for physical function (p = 0.05), PCS (p < 0.05), and social function (p < 0.02). Age- and gender-adjusted SF-36 scores at follow-up assessment are shown in Fig. 3 according to whether or not the patients still had the implant at follow-up. The age- and gender-matched SF-36 values of the general French population are included for reference. Table 3 allows comparison of the long-term SF-36 values of our two subgroups with long-term values reported by Glaser et al. [8] in patients who had undergone primary pedicle-screw enhanced lumbar fusion. One should remember that, as stated above, fusion was performed to stabilize the lumbar spine if and when the first-generation Wallis implant was removed. The scores in Table 3 were computed by subtracting patient scores from the appropriate age/gender general population cohort so that negative values indicate function below that of the cohort and positive scores indicate function better than the average person in the cohort.
Discussion
This cohort study was retrospective and consequently suffers the limitations of that design. There was no control group and no randomization. Furthermore, the decision to stabilize the operated lumbar spine was up to the individual surgeons. Although almost all the patients agreed to complete the questionnaire, only 80% of the 133 patients who were possible candidates for this study responded to the survey. However, there was no significant difference between the patients lost to follow-up evaluation and the followed group in terms of age at operation, sex, BMI, number of levels operated, or indications. This does not prove that the patients who responded were representative of the total population, but it is inconsistent with the existence of a selection bias. Other long-term studies of patients operated for lumbar degenerative disc disease have attrition rates ranging from as low as 0% [4] to as high as 53% [8] of still-living patients. Our overall attrition rate of 20% was similar to those of two other reports, which lost 16% and 19% of surviving patients to long-term follow-up, respectively [10, 12]. Another shortcoming of the present study was the lack of preoperative clinical data. In a recently published retrospective study of TDRs, David chose to classify the patients’ functional status as excellent, good, fair, or poor, arguing that the ODI, VAS, and SF-36 outcome questionnaires in use today were either not validated measures or were not in widespread use when his patients were operated resulting in the absence of baseline data to compare [4]. Nevertheless, we felt these scores would be of particular interest in this 13-year follow-up because they are all validated and self-reported scores, which are theoretically difficult to influence. Furthermore, as noted by Glaser et al. [8], the SF-36 values can be compared to those of the age- and gender-matched general population. These clinical scores also permit comparisons among the different subgroups of the study.
The present long-term clinical results in the patients who still have the implant suggest that dynamic stabilization is an effective technique for the lumbar degenerative disorders we treated. The 95% level of patients “satisfied” or “very satisfied” was high, even compared to the 82% satisfaction rate reported for posterior fusion patients at long-term [8]. The average ODI score of 19% indicates little disability. The self-reported leg and low back pain levels are also moderately low. Furthermore, the quality-of-life scores were only slightly below those of the age- and gender-matched general population. Our long-term clinical results are even comparable to those of TDR patients [4].
Just as important as the promising outcome itself, were the large significant differences observed between the patients who still had the implant and those in whom the implant was removed and replaced by arthrodesis. The significantly poorer clinical outcome of the patients in whom the dynamic stabilization device was replaced by a fusion procedure would suggest either that prior use of the interspinous stabilization device somehow induces a greater failure rate of subsequent arthrodesis, or that any patient who undergoes fusion might expect this significantly poorer outcome. The report on long-term clinical outcome of pedicle-screw enhanced fusion cited above with our results is consistent with the second hypothesis [8]. Their quality of life compared to the general population was super imposable with that of our fusion subgroup. The same was true for the reported long-term pain levels (approximately 3/6 and only 26% were using less pain medication at 10 years than at the time of their primary osteosynthesis) [8]. Interestingly, the pain level reported by their fusion patients at long-term follow-up was similar to the level reported by the same patients shortly after having the arthrodesis, suggesting that more was involved than a problem of progressive postoperative deterioration.
The present study shows that the long-term clinical outcome of our subgroup that still had the first-generation Wallis implant was better than that of fused patients, justifying the development of lumbar dynamic stabilization in the 1980s. Various hypotheses may explain why patients with dynamic stabilization have less pain and disability than fusion patients and quality of life close to that of subjects of the same age who have never had lumbar surgery. Perhaps the original hypothesis was founded that mechanical normalization of the treated segment permits healing of the intervertebral disc, as recently confirmed in animal studies [16]. It is also possible that motion preservation may indeed achieve better long-term clinical results than fusion in the remaining adjacent and non-adjacent untreated lumbar segments. A 10-year follow-up of TDR patients is consistent with the latter hypothesis [4, 17].
In patients who have a lumbar arthrodesis, the clinical results related to the outcome of the index levels and of the remaining untreated levels are well documented. Concerning the index level, low back pain should be resolved if it originates in the disc, vertebral body endplates, or facet joints of a successfully fused intervertebral segment. However, pseudarthrosis can be a source of low back pain after fusion. Etminan et al. estimated that roughly 15% of attempted spinal fusions result in pseudarthrosis [6]. Complications of arthrodesis might also affect subsequent quality-of-life and disability scores [20].
In fused patients, the motion patterns of the residual intact motion segments are modified in proportion to the extent and rigidity of the fused segments, and this may accelerate the degenerative process at the initially intact levels [26]. This notion of accelerated degeneration of motion segments adjacent to fused segments is controversial. Because genetic factors play a greater role than mechanical factors in the development of degenerative disease in intervertebral motion segments [1, 27], authors of some imaging and biomechanical studies have contended that the added constraints on segments around a lumbar arthrodesis should play a negligible role in the subsequent course of degeneration in the unfused segments [21, 22]. However, the cited studies do not provide corresponding clinical results, which are more relevant to therapeutic decision making than purely genetic, in vitro mechanical, or imaging aspects [2, 5]. The long-term clinical findings achieved by the present dynamic stabilization device, despite the study limitations, are not only very acceptable but possibly even better than results obtained with primary fusion. Therefore, although the predominant role of genetics in intervertebral degeneration is undeniable in unoperated subjects, the mechanical alterations resulting from lumbar fusion may play an important role in the long-term clinical results of surgically treated patients. Consistent with our findings, other long-term studies have shown disturbingly high rates of clinically significant symptoms in lumbar segments not included in previous fusion procedures [7, 13]. Their findings along with the present clinical data and our previous survivorship analysis [25] would suggest that use of dynamic stabilization instead of fusion in certain indications might reduce the number of secondary lumbar procedures during the first 10 years after the initial operation. The impact of dynamic stabilization could be even greater at present, given a recent report demonstrating a paradoxical increase in the rate of reoperations after lumbar fusion in spite of improvements in instrumentation and techniques during the last decade [19].
Today, there exist other interspinous dynamic stabilization systems, but they are fundamentally different from the first- and second-generation Wallis devices, which have hard interspinous spacers and strong tension bands [28]. Other types of dynamic stabilization devices are also being proposed for degenerative disorders of the lumbar spine. While most of these devices are recent, the first-generation Wallis implant was initially used in patients close to 20 years ago [15]. To the best of the authors’ knowledge, this is the first long-term study of clinical outcome for any kind of interspinous dynamic stabilization system.
Conclusion
Clinical results of lumbar dynamic stabilization with the first-generation Wallis system at long-term follow-up evaluation are reviewed. This relatively superficial and easily reversible surgical procedure, which preserved spinal anatomy, was applied in patients who had been scheduled for fusion for painful degenerative lumbar conditions. A 13-year clinical outcome in terms of pain level, disability, quality of life, and patient satisfaction was excellent, especially in the patients who were not subsequently converted to arthrodesis. The quality of life of these patients approached values of the age- and gender-matched general population. The first-generation Wallis dynamic stabilization system successfully delayed stabilization by arthrodesis and provided outcomes comparable to the more technically demanding TDR procedures.
References
Ala-Kokko L (2002) Genetic risk factors for lumbar disc disease. Ann Med 34:42–47
Borenstein DG, O’Mara JW Jr, Boden SD et al (2001) The value of magnetic resonance imaging of the lumbar spine to predict low-back pain in asymptomatic subjects: a seven-year follow-up study. J Bone Joint Surg Am 83-A:1306–1311
Calmels P, Bethoux F, Condemine A et al (2005) Low back pain disability assessment tools. Ann Readapt Med Phys 48:288–297
David T (2007) Long-term results of one-level lumbar arthroplasty: minimum 10-year follow-up of the CHARITE artificial disc in 106 patients. Spine 32:661–666
Elfering A, Semmer N, Birkhofer D et al (2002) Risk factors for lumbar disc degeneration: a 5-year prospective MRI study in asymptomatic individuals. Spine 27:125–134
Etminan M, Girardi FP, Khan SN et al (2002) Revision strategies for lumbar pseudarthrosis. Orthop Clin North Am 33:381–392
Ghiselli G, Wang JC, Bhatia NN et al (2004) Adjacent segment degeneration in the lumbar spine. J Bone Joint Surg Am 86-A:1497–1503
Glaser J, Stanley M, Sayre H et al (2003) A 10-year follow-up evaluation of lumbar spine fusion with pedicle screw fixation. Spine 28:1390–1395
Guehring T, Omlor GW, Lorenz H et al (2006) Disc distraction shows evidence of regenerative potential in degenerated intervertebral discs as evaluated by protein expression, magnetic resonance imaging, and messenger ribonucleic acid expression analysis. Spine 31:1658–1665
Guigui P, Wodecki P, Bizot P et al (2000) [Long-term influence of associated arthrodesis on adjacent segments in the treatment of lumbar stenosis: a series of 127 cases with 9-year follow-up]. Rev Chir Orthop Reparatrice Appar Mot 86:546–557
Hartigan C, Rainville J, Sobel JB et al (2000) Long-term exercise adherence after intensive rehabilitation for chronic low back pain. Med Sci Sports Exerc 32:551–557
Katz JN, Lipson SJ, Chang LC et al (1996) Seven- to 10-year outcome of decompressive surgery for degenerative lumbar spinal stenosis. Spine 21:92–98
Kawaguchi Y, Ishihara H, Kanamori M et al (2007) Adjacent segment disease following expansive lumbar laminoplasty. Spine J 7:273–279
Keller SD, Ware JE Jr, Bentler PM et al (1998) Use of structural equation modeling to test the construct validity of the SF-36 health survey in ten countries: results from the IQOLA project. International quality of life assessment. J Clin Epidemiol 51:1179–1188
Khoueir P, Kim KA, Wang MY (2007) Classification of posterior dynamic stabilization devices. Neurosurg Focus 22:E3
Kroeber M, Unglaub F, Guehring T et al (2005) Effects of controlled dynamic disc distraction on degenerated intervertebral discs: an in vivo study on the rabbit lumbar spine model. Spine 30:181–187
Lemaire JP, Carrier H, Sariali el H et al (2005) Clinical and radiological outcomes with the Charite artificial disc: a 10-year minimum follow-up. J Spinal Disord Tech 18:353–359
Leplege A, Ecosse E, Verdier A et al (1998) The French SF-36 health survey: translation, cultural adaptation and preliminary psychometric evaluation. J Clin Epidemiol 51:1013–1023
Martin BI, Mirza SK, Comstock BA et al (2007) Are lumbar spine reoperation rates falling with greater use of fusion surgery and new surgical technology? Spine 32:2119–2126
Okuda S, Miyauchi A, Oda T et al (2006) Surgical complications of posterior lumbar interbody fusion with total facetectomy in 251 patients. J Neurosurg Spine 4:304–309
Pellise F, Hernandez A, Vidal X et al (2007) Radiologic assessment of all unfused lumbar segments 7.5 years after instrumented posterior spinal fusion. Spine 32:574–579
Rohlmann A, Neller S, Bergmann G et al (2001) Effect of an internal fixator and a bone graft on intersegmental spinal motion and intradiscal pressure in the adjacent regions. Eur Spine J 10:301–308
Senegas J (1991) Surgery of the intervertebral ligaments, alternative to arthrodesis in the treatment of degenerative instabilities. Acta Orthop Belg 57(Suppl 1):221–226
Senegas J (2002) Mechanical supplementation by non-rigid fixation in degenerative intervertebral lumbar segments: the Wallis system. Eur Spine J 11(Suppl 2):S164–S169
Senegas J, Vital JM, Pointillart V et al (2007) Long-term actuarial survivorship analysis of an interspinous stabilization system. Eur Spine J 16:1279–1287
Shono Y, Kaneda K, Abumi K et al (1998) Stability of posterior spinal instrumentation and its effects on adjacent motion segments in the lumbosacral spine. Spine 23:1550–1558
Videman T, Battie MC, Ripatti S et al (2006) Determinants of the progression in lumbar degeneration: a 5-year follow-up study of adult male monozygotic twins. Spine 31:671–678
Wilke H-J, Drumm J, Haeussler K, et al (2007) Biomechanical comparison of the segmental stability and intradiscal pressure achieved with different interspinous implants. In: 53rd annual meeting of the Orthopaedic Research Society. Orthopaedic Research Society, San Diego, CA, p 88
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Luciano Mastronardi, Roma, Italy
This is a very interesting article on a large series of patients with various type of lumbar instabilities treated with the interspinous device Wallis. I think any spine surgeon would find the data analysis complete, the follow-up adequate, and the results promising.
Even if I am not completely convinced that the interspinous device Wallis, which I use time by time, can avoid a lumbar fusion in a very high percentage of cases, I think that the readers will enjoy this experience. A multicenter, randomized study comparing the results of standard fixation and interspinous techniques would be very useful for the future.
Hatem Sabry, Jack Jallo, Philadelphia, USA
The authors of this article have conducted a retrospective study aimed at evaluating the health status of the patients who underwent a lumbar dynamic stabilization procedure. This is a well-written article covering a relatively large number of patients treated with the Wallis dynamic stabilizer and with a long-term follow-up of 13 years.
The authors concluded that the patients had excellent clinical results in terms of pain, disability, and quality of life. The question that comes to mind of course after reading this article is how these patients would compare to others managed conservatively. The answer to this would ideally be provided by a randomized, controlled study.
Yet, we cannot ignore that this study brings to light an important, less invasive, and somewhat underestimated alternative to traditional decompression and fusion of the spinal canal.
Li-Yang Dai, Shanghai, China
Senegas et al. provided a relatively large series of patients treated with interspinous process spacers for degenerative disorders of the lumbar spine. Their results of long-term follow-up are interesting and show success in the patients with implants survived. This clinical report suggests that satisfactory long-term results could be achieved when these devices are applied in appropriately selected patients. I congratulate the authors on adding to our knowledge in lumbar spine surgery.
As the authors pointed out, this study might be limited in its retrospective nature. It is difficult to determine whether the improvement of the clinical symptoms is the result of decompression or dynamic stabilization, or both of them. Therefore, a randomized, controlled study should be required for comparing the results between interspinous device insertion and fusion, although the authors found that better clinical outcome was noted at follow-up in the patients who still had the dynamic stabilizer than the patients who received subsequent fusion.
Another limitation of this study might be the heterogeneity of enrolled patients with regard to surgical indications. As generally believed, the interspinous process spacers are indicated for the patients with neurogenic claudication resulting from lumbar spinal stenosis. Our previous study showed that the capacity of the spinal canal is influenced by flexion-extension motion of the lumbar spine with a significant increase from extension to flexion (1). The advantage of using interspinous process spacers may lie in the enlargement of the spinal canal and decrease in painful motion by restricting the extension or increasing the flexion of lumbar spine. So far, as we know, there are no studies showing that interspinous process spacer insertion would be more advantageous than simple discectomy in the treatment of disc herniation. In fact, recurrence of disc herniation after the use of interspinous process devices in the primary discectomy has been reported (2). Concern remains regarding the role of the interspinous process spacers in the treatment of disc herniation.
References
1. Dai LY, Xu YK, Zhang WM, Zhou ZH (1989) The effect of flexion-extension motion of the lumbar spine on the capacity of the spinal canal: an experimental study. Spine 14:523–525
2. Floman Y, Millgram MA, Smorgick Y, Rand N, Ashkenazi E (2007) Failure of the Wallis interspinous implant to lower the incidence of recurrent lumbar disc herniations in patients undergoing primary disc excision. J Spinal Disord Tech 20:337–341
All index operations were performed in the Unité de Pathologie Rachidienne, Centre Hospitalier Pellegrin, Bordeaux.
Rights and permissions
About this article
Cite this article
Sénégas, J., Vital, JM., Pointillart, V. et al. Clinical evaluation of a lumbar interspinous dynamic stabilization device (the Wallis system) with a 13-year mean follow-up. Neurosurg Rev 32, 335–342 (2009). https://doi.org/10.1007/s10143-009-0199-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-009-0199-z