Abstract
Although three-dimensional computed tomographic angiography (3D-CTA) is less complicated and time-consuming than conventional cerebral angiography (CCA) and represents a reliable alternative for evaluating cerebral aneurysms, some patients experience aneurysmal rerupture during 3D-CTA. Two women, 79 and 71 years old, who presented with severe subarachnoid hemorrhage (SAH) underwent 3D-CTA within 3 h after SAH onset. Their images clearly indicated extravasation from their aneurysms. Neither patient recovered from deep coma, and both died within 2 days. We reviewed the literature with special reference to the condition of SAH patients at admission and the interval between SAH onset and 3D-CTA, and discuss serious complications of 3D-CTA study. Although aneurysmal rerupture may reflect the natural course, rerupture during 3D-CTA, especially in SAH patients who are in poor clinical condition during the acute stage, should be recognized as a potentially fatal complication. Their blood pressure must be strictly controlled and factors such as their clinical condition and the interval from the ictus must be considered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although conventional cerebral angiography (CCA) is the gold standard for diagnosing ruptured intracranial aneurysms, patients undergoing CCA in the acute stage of subarachnoid hemorrhage (SAH) are at significant risk for aneurysmal rerupture during the procedure [6, 7, 14, 17]. Three-dimensional computed tomographic angiography (3D-CTA) has been suggested as a reliable alternative to CCA for the detection and evaluation of cerebral aneurysms because it can be performed even in the acute stage of SAH, exposes the patient to less risk and discomfort, and is easier to perform and less expensive than CCA [1, 5, 16].
We report two patients who died as a result of aneurysmal rerupture during 3D-CTA and discuss our experience in the context of present knowledge about the severe complications that may attend 3D-CTA.
Case reports
Case 1
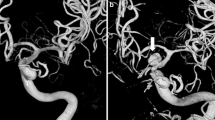
This 79-year-old woman suddenly lapsed into a deep coma and was referred to our hospital. On admission, she presented with grade 5 according to the World Federation of Neurological Surgeons (WFNS). The initial computed-tomography (CT) scan showed diffuse SAH and intraventricular hemorrhage predominantly in the right lateral ventricle. A subsequent 3D-CTA scan demonstrated a reversed cone-like structure connecting to a dumbbell-shaped aneurysm of the right posterior cerebral artery, findings suggestive of extravasation of the contrast medium and rerupture (Fig. 1). The interval between the ictus and the acquisition of 3D-CTA scans was less than 3 h. Her blood pressure (BP) markedly increased from 109/59 mmHg on admission to 229/108 mmHg immediately after 3D-CTA. She did not recover to an operable state and died on the 2nd hospital day.
Plain CT scan obtained immediately before (a) and after (b) 3D-CTA. Note the wide diffusion of a thin SAH with intraventricular hemorrhage (a). An irregular lesion (arrow) whose density is equal to that of the aneurysm and artery is seen on the 3D-CTA, but not the plain CT scan. 3D-CTA (c, stereoscopic view) shows a dumbbell-shaped aneurysm of the right posterior cerebral artery (superior view). A reversed cone-shaped structure (arrowhead) connecting to the proximal portion of the aneurysm protrudes toward the temporal horn of the right lateral ventricle
Case 2
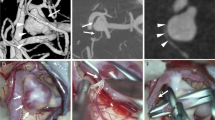
This 71-year-old woman suddenly fell into a deep coma and was referred to our hospital. Her WFNS grade was 5 on admission. The admission CT scan showed diffuse SAH and a thick hematoma in the left Sylvian fissure. The subsequent 3D-CTA scan demonstrated a twisted ribbon-like structure originating from a giant aneurysm of the left internal carotid artery, suggestive of rerupture (Fig. 2). The interval between the initial ictus and acquisition of the 3D-CTA scan was less than 3 h. Her BP was 164/82 mmHg on admission; the administration of diltiazem reduced it to below 130 mmHg before CT evaluation. However, it rose to 174/88 mmHg immediately after 3D-CTA study and further increased to greater than 200 mmHg thereafter. She did not recover and died on the same day.
Discussion
Although it is not clear whether CCA performed in the acute stage of SAH raises the incidence of aneurysmal rerupture beyond that of spontaneous rerupture, its avoidance during the first 6 h after the last insult has been recommended [6, 7, 17]. The reported rate of aneurysmal rerupture during emergency CCA within 6 h of the ictus is 3–8.7%; according to a recent study it increased up to 23.9% when the procedure was performed within 3 h [6, 7, 14, 17]. The main risk factors are the patient’s condition at admission, the aneurysmal site, and the interval between SAH and CCA. There is a significant correlation between aneurysmal rerupture and a worse clinical grade, the internal carotid and middle cerebral artery localization of the aneurysms, and the performance of angiographic procedures within the first 3–6 h after occurrence of the ictus. On the other hand, there is no significant correlation between aneurysmal rerupture during CCA and the size or shape of the aneurysm and the patient age and sex [6, 7, 14, 17]. Therefore, to decrease the risk of aneurysmal rerupture that attends CCA in the early stages after the initial ictus, 3D-CTA study has been suggested as a potentially reliable alternative to facilitate surgical planning [7, 18].
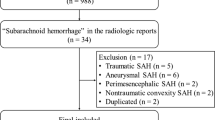
Our search of the literature found eight previously reported SAH patients (seven men and one woman ranging in age from 41 to 71 years) who suffered aneurysmal rerupture during 3D-CTA (Table 1) [3, 4, 11–13]. Of ten patients, including the two reported here, six manifested WFNS grade 5 at admission and seven died within 2 weeks of the initial insult. The female:male ratio was 3:7; in four the aneurysm was located at the anterior cerebral artery. Of the ten patients reviewed here, six underwent 3D-CTA in the acute stage within 3 h of the last insult rather than the putatively more risky CCA procedure [6, 7, 17]. Considering the female predisposition for SAH [2], the apparent predominance of males over females among cases with rerupture during 3D-CTA may be characteristic. However, the observation that the incidence of rerupture was similar in patients undergoing CCA or 3D-CTA during the acute stage leads us to posit that the important risk factors are the grade at admission and the interval between the last insult and angiographic study. With the exception of one, all reported patients who suffered rerupture had a very poor outcome.
Nakatsuka et al. [12], who did not detail their selection criteria, reported the highest rerupture rate during 3D-CTA. Among their 28 consecutive patients who underwent 3D-CTA study within a few hours of SAH onset, 5 (17.9%) suffered aneurysmal rerupture. Between January 2004 and December 2005, we performed 3D-CTA on 61 consecutive patients with non-traumatic SAH. Of these, 12 (19.7%) died. If we suspect SAH at admission, we routinely control the patient’s BP with calcium blockers, nifedipine, and/or diltiazem before CT evaluation. Of our 61 patients subjected to 3D-CTA in the acute phase, the 2 reported here (3.3%) suffered aneurysmal rerupture.
It has been suggested that rerupture is incidental to aneurysmal SAH in the acute stage and that 3D-CTA does not significantly increase the risk for rerupture because, unlike CCA, 3D-CTA does not induce a transient increase in the arterial BP [12, 13, 15]. However, under certain experimental conditions, the intravascular injection of contrast medium leads to a transient increase in the arterial BP before or after a BP decrease [8–10]. Therefore, 3D-CTA, which requires a bolus injection of contrast medium, may increase the risk for aneurysmal rerupture beyond the already existing level, especially in patients who are in poor clinical condition and are examined during the acute stage. Based on our findings, we conclude that the incidence of aneurysmal rerupture is not significantly lower in SAH patients undergoing 3D-CTA during the acute phase than in those examined by CCA.
Conclusions
Because the incidence of aneurysmal rerupture may not be significantly lower in SAH patients undergoing 3D-CTA during the acute phase than in those examined by CCA, their blood pressure must be strictly controlled and factors such as their clinical condition and the interval from the ictus must be considered.
References
Chappell ET, Moure FC, Good MC (2003) Comparison of computed tomographic angiography with digital subtraction angiography in the diagnosis of cerebral aneurysms: A meta-analysis. Neurosurgery 52:624–631
Hamada J, Morioka M, Yano S, Kai Y, Ushio Y (2004) Incidence and early prognosis of aneurysmal subarachnoid hemorrhage in Kumamoto Prefecture, Japan. Neurosurgery 54:31–38
Holodny A, Farkas J, Schlenk R, Maniker A (2003) Demonstration of an actively bleeding aneurysm by CT angiography. AJNR Am J Neuroradiol 24:962–964
Josephson SA, Dillon WP, Dowd CF, Malek R, Lawton MT, Smith WS (2004) Continuous bleeding from a basilar terminus aneurysms imaged with CT angiography and conventional angiography. Neurocrit Care 1:103–106
Karamessini MT, Kagadis GC, Petsas T, Karnabatidis D, Konstantinou D, Sakellaropoulous GC, Nikiforidis GC, Siablis D (2004) CT angiography with three-dimensional techniques for the early diagnosis of intracranial aneurysms: Comparison with intra-arterial DSA and surgical findings. Eur J Radiol 49:212–223
Komiyama M, Tamura K, Nagata Y, Fu Y, Yagura H, Yasui T (1993) Aneurysmal rupture during angiography. Neurosurgery 33:798–803
Kusumi M, Yamada M, Kitahara T, Endo M, Kan S, Iida H, Sagiuchi T, Fujii K (2005) Rerupture of cerebral aneurysms during angiography: A retrospective study of 13 patients with subarachnoid hemorrhage. Acta Neurochir (Wien) 147:831–837
Lasser EC, Lamkin GE (2002) Mechanisms of blood pressure change after bolus injections of X-ray contrast media. Acad Radiol 9(Suppl 1):s72–s75
Morcos SK, Dawson P, Pearson JD, Jeremy JY, Davenport AP, Yates MS, Tirone P, Cipolla P, de Haen C, Muschick P, Krause W, Refsum H, Emery CJ, Liss P, Nygren A, Haylor J, Pugh ND, Karlsson JO (1998) The haemodynamic effects of iodinated water-soluble radiographic contrast media: A review. Eur J Radiol 29:31–46
Morcos SK (2003) Review article: Effects of radiographic contrast media on the lung. Br J Radiol 76:290–295
Nakada M, Akaike S, Futami K (2000) Rerupture of an aneurysm during three-dimensional computerized tomography angiography. Case illustration. J Neurosurg 93:900
Nakatsuka M, Mizuno S, Uchida A (2002) Extravasation on three-dimensional CT angiography in patients with acute subarachnoid hemorrhage and ruptured aneurysm. Neuroradiology 44:25–30
Ryu CW, Kim SJ, Lee DH, Suh DC, Kwun BD (2005) Extravasation of intracranial aneurysm during computed tomography-angiography: Mimicking a blood vessel. J Comput Assist Tomogr 29:677–679
Saitoh H, Hayakawa K, Nishimura K, Okuno Y, Teraura T, Yumitori K, Okumura A (1995) Rerupture of cerebral aneurysms during angiography. AJNR Am J Neuroradiol 16:539–542
Saitoh H, Hayakawa K, Nishimura K, Okuno Y, Murayama C, Miyazawa T, Zieroth BF, Shimizu Y (1996) Intracarotid blood pressure changes during contrast medium injection. AJNR Am J Neuroradiol 17:51–54
Tipper G, U-King-Im JM, Price SJ, Trivedi RA, Cross JJ, Higgins NJ, Farmer R, Wat J, Kirollos R, Kirkpatrick PJ, Antoun NM, Gillard JH (2005) Detection and evaluation of intracranial aneurysm with 16-row multislice CT angiography. Clin Radiol 60:565–572
Yasui T, Kishi H, Komiyama M, Iwai Y, Yamanaka K, Nishikawa M (1996) Very poor prognosis in cases with extravasation of the contrast medium during angiography. Surg Neurol 45:560–565
Zaehringer M, Wedekind C, Gossmann A, Krueger K, Trenschel G, Landwehr P (2002) Aneurysmal rerupture during selective angiography. Eur Radiol 12(Suppl 3):s18–s24
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hashiguchi, A., Mimata, C., Ichimura, H. et al. Rebleeding of ruptured cerebral aneurysms during three-dimensional computed tomographic angiography: report of two cases and literature review. Neurosurg Rev 30, 151–154 (2007). https://doi.org/10.1007/s10143-007-0068-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-007-0068-6