Abstract
Determination of renal neoplasms, hematoma, infarct, urinoma, cysts, and pyelonephritis may require contrast material administration following unenhanced CT in patients with flank pain. In this pictorial review, we aimed to clarify when contrast material administration is needed following vague urinary system findings on unenhanced CT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Contrast is not routinely required for CT imaging of renal colic, although it may be required occasionally to clarify equivocal unenhanced CT findings and characterization of tumoral and cystic lesions. Indications for contrast-enhanced CT evaluation (based on unenhanced CT findings) are: (1) presence of unilateral perinephric stranding without hydroureteronephrosis, with/without renal enlargement (acute renal infarction, renal vein thrombosis, acute pyelonephritis), (2) significant hypo/hyperdense perirenal collection (urinoma, hematoma) with/without presence of hydroureteronephrosis, (3) presence of a mass or complicated cyst with/without calculus, and (4) negative unenhanced CT findings in a patient with unexplained hematuria.
In the presence of such findings, differential diagnosis spectrum should be broadened and additional contrast-enhanced CT scan should be performed. Via this approach, a variety of pathologies presenting with acute renal colic and hematuria mimicking urinary stone disease can be readily diagnosed (Fig. 1).
Infections
Acute pyelonephritis is a clinical diagnosis with findings simulating an obstructing ureteral stone. Imaging is indicated when there is inadequate response to treatment and/or a complication is suspected [1]. On unenhanced CT, pyelonephritis may manifest as asymmetric perinephric stranding and/or mild renal enlargement when infection is moderate to severe, but mild pyelonephritis usually has no unenhanced CT findings. On contrast-enhanced images, pyelonephritis may be seen as wedge-shaped areas of low attenuation and poor corticomedullary differentiation representing hypoperfusion and edema (Fig. 2). Additionally, delayed phase images may demonstrate obliterated renal sinus, linear hypo-hyperenhancing foci parallel to renal tubules and collecting ducts. More serious complications of pyelonephritis such as renal or perinephric abscess, its unusual forms like emphysematous, and fungal pyelonephritis can also be demonstrated with contrast-enhanced CT [2].
Neoplasms
Renal cell carcinoma (RCC) is one of the main concerns of radiologists because it can be easily missed on unenhanced CT. RCC should be excluded in any middle-aged to elderly patient with flank pain and hematuria [3]. Large RCCs can be detected on unenhanced CT but small RCCs can be overlooked. Most RCCs are solid lesions with ≥20 HU on unenhanced CT. Smaller tumors usually appear homogeneously, while larger lesions are more heterogeneous due to internal hemorrhage or necrosis. Calcifications can be found in 1/3 of RCCs. On unenhanced CT, RCC may appear as subtle, focal contour abnormality of kidney or as complex renal cysts. If such signs are present, intravenous contrast will be useful for further characterization. Nephrographic phase images are the most accurate for detecting renal masses and their internal texture (Fig. 3) [4].
Transitional cell carcinoma (TCC) is commonly encountered in urinary bladder, but 5% of them arise from the ureter or renal pelvis/calices. Patients with TCC present with macroscopic or microscopic hematuria, acute flank pain, and renal colic. Renal TCC is seen as pelvicaliceal irregularity and focal or diffuse mural thickening. TCCs can show early enhancement after contrast. It is typically seen as a sessile filling defect in excretory phase expanding centrifugally with compression of renal sinus fat. Asymmetric or circumferential ureteric wall thickening, luminal narrowing or infiltrating mass, hydronephrosis, and hydroureter are frequent findings of ureteric TCC (Fig. 4) [5].
Renal cyst complications
In the presence of suspicious complicated renal cysts contrast, administration can provide depiction of a possible malignancy. Management of atypical cystic renal masses on unenhanced CT is a common problem. These types of renal cysts may be complicated by hemorrhage or infection and may represent cystic types of renal cell cancer. In such cases, further evaluation of the cystic lesion via IV contrast is required (Fig. 5).
Bosniak classification system is a practical method limiting the number of complex cystic renal masses requiring surgery and may influence the choice of surgical technique. The degree of enhancement of a lesion reflects its vascularity, which is a critical factor in proper categorization (Fig. 6) [6].
Vascular lesions
Acute renal infarction (ARI) is a cause of acute flank pain that may require contrast for diagnosis. In patients with increased risk of thromboembolism referring with unexplained acute flank pain, ARI should be suspected. Under such circumstances, hematuria, leukocytosis, and an elevated serum lactate dehydrogenase are strongly supportive for diagnosis. ARI can be easily missed because CT findings can be subtle such as mild perinephric stranding. In such cases, following IV contrast, wedge-shaped low attenuation areas consistent with ARI can be seen (Fig. 7) [7].
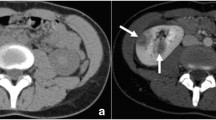
Patients with acute renal vein thrombosis present with flank pain, hematuria, and nephrotic syndrome. Acute membranous glomerulonephritis, systemic lupus erythematosis, diabetes, sepsis, and dehydration are major factors that may result in acute renal vein thrombosis. The affected kidney is enlarged with perinephric stranding on unenhanced images whereas delayed and prolonged nephrogram is observed due to the decrease in glomerular filtration and tubular compression secondary to interstitial edema. Moreover, thrombosed renal vein is distended with a low attenuation clot (Fig. 8) [8].
A 38-year-old female with a 2-week history of pyrexia, dysuria, and two episodes of rigors, treated for pyelonephritis presented with acute right flank pain and microscopic hematuria. Unenhanced CT image shows enlargement of right kidney with slight thickening of anterior pararenal fascia (arrowhead) (a); contrast-enhanced CT image demonstrates thrombus within right renal vein (arrow) (b) (courtesy of Steven Colley M.D. from Birmingham, UK)
Renal artery aneurysms (RAA) compromise 15–20% of all visceral aneurysms. Arteriosclerosis, hypertension, fibromuscular dysplasia, renal angiomyolipoma, pregnancy, and trauma are predisposing factors. Clinical findings of RAA are non-specific and include microscopic hematuria, hypertension, and flank pain. Although uncommon, in case of rupture, acute flank pain and shock may occur [9]. Unruptured RAA cannot be readily seen on unenhanced CT or can rarely be seen as subtle small hyperdense focus which cannot be prospectively determined and discriminated from other lesions; following IV contrast, lesion can be noticed as a rapidly enhancing focus (Fig. 9) [8].
A 28-year-old male with flank pain and macroscopic hematuria with a known history of kidney biopsy 1 week ago. Axial and coronal reformatted contrast-enhanced CT images show asymmetrically enlarged right kidney secondary to perirenal hematoma and perirenal stranding (arrowhead) (a) and rapidly enhancing round lesion consistent with traumatic renal artery pseudoaneurysm (arrows) (a, b, c)
Left renal vein (LRV) entrapment syndrome also known as “nutcracker syndrome” is characterized with compression of LRV between superior mesenteric artery and abdominal aorta. Such patients usually present with recurrent left flank and abdominal pain, with or without hematuria. Contrast-enhanced CT readily demonstrates venous tree of left kidney and compression non-invasively [10].
Urinoma
In case of perirenal and/or periureteral fluid on unenhanced CT, urinoma should be suspected. Urinoma is a chronic encapsulated extravasation of urine that leaks slowly into perirenal space and collects within fascia. It may be a result of forniceal rupture secondary to acute urinary obstruction (mostly due to urinary stones), but trauma and diagnostic/therapeutic instrumentation can also lead to urinoma. Contrast-enhanced CT is the study of choice for diagnosis [11]. Contrast-enhanced CT protocol in patients with a suspected urine leak involves scanning of abdomen and pelvis following IV administration of 100–150 ml contrast. Delayed phase (5–20 min) images are key for demonstrating the urine leak as iodinated urine increases attenuation of urinoma (Fig. 10).
A 35-year-old female with a history of urinary stone intervention 10 days ago. Axial unenhanced CT images show significant perinephric fluid collection (arrowheads) (a) and left ureteric stone (arrow) with left retroperitoneal fluid (asterisk) (b); delayed contrast-enhanced image (c) shows urinary leak from ureter (arrow)
Acute perirenal hematoma
An acute perirenal hematoma may be a result of trauma, renal and adrenal tumors, coagulopathy, renal infarction, renal cysts, or can be idiopathic [12]. In case of isolated subcapsular or perirenal hemorrhage, occult malignancies, which may result in spontaneous hemorrhage and concomitant flank pain, should be considered. On unenhanced CT scans, acute subcapsular hematoma is usually seen as hyperdense; as hematoma resolves, its fluid content increases and becomes more hypodense. On contrast-enhanced CT, hematoma shows lower enhancement compared to renal parenchyma but IV contrast not only enables demonstration of hematoma burden but also it may contribute to determination of the underlying etiology (Fig. 9) [13].
Imaging protocol
For patients presenting to the emergency room with acute onset flank pain, multidetector computed tomography (MDCT) scans are performed by 2-, 4-, and 16-detector row MDCT scanners (Siemens, Erlangen, Germany) with the following imaging parameters. Detector collimations: 2 × 2.5 mm, 4 × 2.5 mm, 16 × 1.5 mm; slice thickness: 3 mm; pitch: 1.5; mAs: 80; kVp: 120. Unenhanced images are instantly evaluated by emergency radiologists and if one or more than one of those suspicious findings mentioned above are detected, 100–150 ml of non-ionic contrast material is given through an 18G IV line at a rate of 3 ml s−1. In case of a suspicion of an arterial pathology, arterial phase scan of kidneys is performed using bolus tracking method; otherwise, the routine contrast-enhanced images are obtained with the same parameters in nephrographic phase at approximately 100 s after intravenous contrast injection for suspicious masses and complicated cysts; whereas in patients with perirenal collections and negative unenhanced CT findings but with positive unexplained hematuria, additionally entire urinary system is scanned at urographic phase that corresponds to 7–10-min delay after injection. In almost all patients, coronal and sagittal multiplanar reconstructions are obtained in addition to axial images for better delineation of etiology.
Conclusion
Potential benefits and disadvantages of administering contrast and its impact on patient management should be evaluated by radiologists and referring physicians. A complete clinical history and good communication between the referring physician and radiologist are important for narrowing the differential diagnosis of acute renal colic. As a result, tailored CT examination can be performed, improving diagnostic accuracy.
Take home messages
-
1-
Common clinical conditions requiring contrast-enhanced CT after unenhanced CT scan in a patient presenting with flank pain and hematuria are: infections, neoplasms, renal cyst complications, vascular lesions, urinoma, and acute perirenal hematoma.
-
2-
Suspicious unenhanced CT findings in absence of a urinary stone should be carefully evaluated and correct management should be tailored for each case accordingly.
References
Miller FH, Kraemer E, Dalal K, Keppke A, Huo E, Hoff FL (2005) Unexplained renal colic: what is the utility of IV contrast. Clin Imaging 29:331–336 doi:10.1016/j.clinimag.2005.01.002
Saunders HS, Dyer RB, Shifrin RY, Scharling ES, Bechtold RE, Zagoria RJ (1995) The CT nephrogram: implications for evaluation of urinary tract disease. Radiographics 15:1069–1085
Rucker CM, Menias CO, Bhalla S (2004) Mimics of renal colic: alternative diagnoses at unenhanced helical CT. Radiographics 24(Suppl 1):S11–S28 doi:10.1148/rg.24si045505
Coll DM, Smith RC (2007) Update on radiological imaging of renal cell carcinoma. BJU Int 99:1217–1222 doi:10.1111/j.1464-410X.2007.06824.x
Browne RF, Meehan CP, Colville J, Power R, Torreggiani WC (2005) Transitional cell carcinoma of the upper urinary tract: spectrum of imaging findings. Radiographics 25:1609–1627 doi:10.1148/rg.256045517
Israel GM, Hindman N, Bosniak MA (2004) Evaluation of cystic renal masses: comparison of CT and MR imaging by using the Bosniak classification system. Radiology 231:365–371 doi:10.1148/radiol.2312031025
Korzets Z, Plotkin E, Bernheim J, Zissin R (2002) The clinical spectrum of acute renal infarction. Isr Med Assoc J 4:781–784
Kawashima A, Sandler CM, Ernst RD, Tamm EP, Goldman SM, Fishman EK (2000) CT evaluation of renovascular disease. Radiographics 20:1321–1340
Henke PK, Cardneau JD, Welling TH 3rd et al (2001) Renal artery aneurysms: a 35-year clinical experience with 252 aneurysms in 168 patients. Ann Surg 234:454–462 doi:10.1097/00000658-200110000-00005
Ahmed K, Sampath R, Khan MS (2006) Current trends in the diagnosis and management of renal nutcracker syndrome: a review. Eur J Vasc Endovasc Surg 31:410–416 doi:10.1016/j.ejvs.2005.05.045
Titton RL, Gervais DA, Hahn PF, Harisinghani MG, Arellano RS, Mueller PR (2003) Urine leaks and urinomas: diagnosis and imaging-guided intervention. Radiographics 23:1133–1147 doi:10.1148/rg.235035029
Yamamoto K, Yasunaga Y (2005) Antiplatelet therapy and spontaneous perirenal hematoma. Int J Urol 12:398–400 doi:10.1111/j.1442-2042.2005.01059.x
Sebastià MC, Pérez-Molina MO, Alvarez-Castells A, Quiroga S, Pallisa E (1997) CT evaluation of underlying cause in spontaneous subcapsular and perirenal hemorrhage. Eur Radiol 7:686–690 doi:10.1007/BF02742926
Author information
Authors and Affiliations
Corresponding author
Additional information
Erhan Akpinar and Baris Turkbey contributed equally to this work.
Rights and permissions
About this article
Cite this article
Akpinar, E., Turkbey, B., Eldem, G. et al. When do we need contrast-enhanced CT in patients with vague urinary system findings on unenhanced CT?. Emerg Radiol 16, 97–103 (2009). https://doi.org/10.1007/s10140-008-0752-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-008-0752-z