Abstract
Purpose
In the emergency setting, flank pain commonly leads to a noncontrast CT despite a significant percentage of patients having alternative diagnoses, often difficult to characterize without contrast. We investigated the combined utility of urinalysis and history of urolithiasis in identifying patients who are unlikely to have urolithiasis and may benefit from a contrast-enhanced study.
Methods
Retrospective review of 350 patients from May 2013 to May 2016 was performed for patients in the emergency department with renal colic that underwent noncontrast CT and urinalysis testing.
Results
Urolithiasis was present in 282 of the 350 patients reviewed (81%), of which 175 (62%) had an obstructing calculus. RBC-positive urinalysis was present in 231 patients with calculi on CT (sensitivity 82%). Patient history of urolithiasis plus urinalysis had a sensitivity of 94% for detecting calculi. Thirty-five patients (10%) had alternative diagnoses, 33 of which were in patients without obstructing calculi. Sixty-seven patients underwent noncontrast CT despite no history of urolithiasis and a negative urinalysis, 10 of which (15%) had alternative diagnoses. Only three cases in this subset (4%) had nonobstructing 1–2-mm calculi, potentially missed with contrast. In this subset, the projected proportion of optimally characterized cases with intravenous contrast is 96%, compared to 85% without contrast (p = .03).
Discussion
Given the high combined sensitivity of urinalysis and patient history (94%), this simple analysis can confidently direct clinicians to a contrast-enhanced CT in “rule-out” cases of flank pain in patients with a negative history and negative urinalysis, particularly given that 15% of these patients had alternative diagnoses.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Purpose
Kidney stones are a common problem, afflicting up to 1 in 11 people in the USA with an estimated annual cost of 2.1 billion dollars [1, 2]. Urolithiasis often incites flank pain, which is a common presentation to the emergency department (ED) often reflexively triggering a “stone protocol” CT without intravenous or oral contrast. However, while nephrolithiasis figures prominently in the differential diagnosis, flank pain prompts consideration of a host of alternative urological, gastrointestinal, gynecological, pancreatic and hepatobiliary, vascular, and musculoskeletal conditions (Table 1) [3]. While many of these conditions are detectable with a stone protocol CT, many are incompletely characterized and some are potentially not detectable [4,5,6]. As such, stone protocol CT applied indiscriminately threatens missed diagnoses, repeat and/or additional testing, and operational inefficiency.
Many of the conditions potentially missed or incompletely characterized with stone protocol CT are better characterized with contrast-enhanced CT, which demonstrates high sensitivity for renal calculi (≥ 3 mm) [7]. Given the combined utility not only for stone disease but also for alternative diagnoses, contrast-enhanced CT is potentially more appropriate in equivocal cases of flank pain. Including stone-specific clinical parameters, such as urinalysis confirming hematuria and history of urolithiasis, offers an opportunity to triage patients to either stone protocol CT or routine contrast-enhanced CT.
While these clinical parameters fail to capture every patient with clinically significant stones, obstructing stones feature many more findings—hydroureteronephrosis, delayed nephrogram, and perinephric and periureteral inflammation—rendering them much more conspicuous. Only 10% of obstructing stones present without microscopic or gross hematuria [8, 9]. Subjecting the small number of patients without either hematuria or known urolithiasis to enhanced CT instead of stone protocol CT in order to characterize possible alternative diagnoses—present in up to 30% of patients presenting with acute flank pain—is a reasonable prospect, especially if enhanced CT detects renal calculi (Fig. 1) [10,11,12,13]. This study investigates the combined utility of urinalysis and clinical history (of stone disease) to identify patients with a lower likelihood of urolithiasis.
Methods
Study design
Institutional Review Board approval was obtained for this retrospective study. The study was performed at a major, urban academic center. The institutional Radiology Information System (RIS) database was searched over a 3-year period between May 2013 and May 2016 for patients presenting to the emergency department with renal colic undergoing subsequent testing with urinalysis and evaluation with noncontrast CT. The terms “flank, colic, renal, and pain” were entered into the database using multiple permutations until no new cases were found. The database search engine used was Primordial (Primordial Inc., San Mateo, CA). The results of urinalysis posted in the Hospital Information System (HIS) were reviewed for the presence or absence of blood and red blood cells (RBCs). Clinical notes in the HIS were reviewed to determine whether a preceding history of urolithiasis had been established. Patients without a clinical note, without documentation of a positive or negative history of urolithiasis, or without urinalysis were excluded. Additionally, patients with indwelling nephroureteral catheters, nephrostomy catheters, or known urologic malignancy were excluded.
Radiology report review
Finalized CT reports obtained from the database search, previously generated by a board-certified attending radiologist, were reviewed to assess for the presence or absence of (1) renal stone disease, (2) obstructive uropathy, and (3) alternative diagnoses to explain the current symptomatology. Stone size below 3 mm—the established threshold for detectability with contrast—was recorded.
Statistical analysis
Sensitivity and specificity analysis was performed to evaluate stone detection by urinalysis alone and by the combination of urinalysis and/or patient history of stones, with CT as the gold standard. The proportion of cases optimally characterized without intravenous contrast was calculated and compared to the cases projected to be optimally characterized with intravenous contrast. The resultant sensitivities and proportions were compared using a chi-square analysis.
Results
A total of 1543 patients were initially collected by keyword search of radiology reports. One thousand one hundred ninety-three of these patients were excluded from the study—786 patients had no documentation of urinalysis in the HIS and 407 patients had inadequate urological history documentation—yielding 350 patients for the study.
Urolithiasis was present on stone protocol CT in 282 of the 350 patients reviewed (81%), of which 175 (62%) had an obstructing calculus. Sixty-eight patients (19%) had no urolithiasis on CT and no alternative imaging explanation for flank pain (Table 2; Fig. 2).
Macroscopic or microscopic hematuria (positive urinalysis for blood or RBCs, respectively) was seen in 231 patients with calculi on CT (sensitivity 82%). Negative urinalysis was seen in 54 patients without calculi (specificity 80%), with noncontrast CT as the gold standard for diagnosing stone disease. Adding prior history of urolithiasis to urinalysis increased the sensitivity of detecting calculi to 94% (p < .001).
Alternative diagnoses were present in 35 cases (10%), 33 of which were in cases without obstructing calculi and 10 of which were in cases with a negative urinalysis and no history of urolithiasis (Tables 3 and 4).
In patients with a negative urinalysis and no history of urolithiasis (67 patients), 15% (10 cases) had alternative diagnoses, not fully characterized due to lack of contrast. Thus, 6–7 patients would need to be administered intravenous contrast (“number needed to inject”) to optimize 1 CT study. Of the ten cases, three had repeat CT imaging with intravenous contrast within 48 h to evaluate the alternative diagnoses, including aortic dissection, ruptured appendicitis, and right-sided colitis (Figs. 3 and 4). Based on this small dataset, approximately 22 patients would need to be injected to avoid repeat CT. Only three cases (4%) in the negative urinalysis and negative history subset had calculi difficult to detect in the setting of contrast (< 3 mm), all of which were nonobstructing (Table 4). In this subset, noncontrast CT would be able to fully characterize 85% of the cases (negative studies and all calculi) whereas contrast-enhanced CT would be able to fully characterize 96% (negative studies, calculi ≥ 3 mm, and the alternative diagnoses; p = .03).
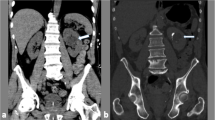
a The initial noncontrast CT of the abdomen and pelvis in this patient with flank pain, negative urinalysis, and no history of urolithiasis demonstrates displaced calcification within the abdominal aorta (arrow), concerning for aortic dissection (suboptimally characterized without IV contrast). No urolithiasis was present. b Follow-up contrast-enhanced CTA 1 h later clearly demonstrates the type B aortic dissection
a The initial noncontrast CT of the abdomen and pelvis in this patient with flank pain, negative urinalysis, and no history of urolithiasis demonstrates dilated loops of bowel in the right lower quadrant, with a reported differential diagnosis of Meckel diverticulitis, terminal ileitis/enteritis, or appendicitis. No urolithiasis was present. b Given the uncertainty of diagnosis clinically and on imaging, repeat CT with contrast was performed 2 h later which clearly demonstrates acute perforated appendicitis (arrow) with a previously unseen fluid collection (arrowhead)
Discussion
Appropriateness and utilization have become increasingly scrutinized in the current healthcare environment in an effort to maximize the value of care delivered. Incorporating patient-specific parameters to optimize imaging protocols helps to meet these demands. The emergency department (ED) presents a high-impact environment to apply this approach where relatively little clinical information is available and throughput constraints demand rapid turnaround in a high-acuity setting. Optimizing the utility of CT is especially important as ED CT utilization continues to escalate [14,15,16,17,18,19,20]. This study shows the potential to incorporate clinical parameters into the clinical decision-making process to improve utilization according to patient-specific parameters and better detect and characterize unexpected abnormalities without sacrificing the accuracy of the primary diagnostic aim.
This study found a very high sensitivity of 94% for detecting urolithiasis by utilizing quick and cost-efficient screening tools—urinalysis and patient history of urolithiasis. Given the high sensitivity of this screening tool, referring physicians can be confidently directed to the correct study, tailored to the patient’s history and results. In “rule-out” cases of flank pain with a negative urinalysis and no prior history of urolithiasis, the patient would benefit from a contrast-enhanced CT based on the results of our study. Fifteen percent of patients in this subgroup had alternative diagnoses to explain their flank pain, a majority of which would be significantly better characterized with intravenous contrast, including pyelonephritis, diverticulitis, colitis, adnexal masses, complex renal masses, ruptured appendicitis, and especially aortic dissection (Figs. 3 and 4). Not only is this important from a patient safety perspective—making a timely diagnosis—it also has the potential to decrease extra unnecessary studies.
This study has a number of limitations. The cases for the study were collected by searching our institutional RIS for noncontrast abdominal CT with indications similar to “flank pain.” Since the indication on the radiology report may be erroneous—due to an unclear clinician-provided history, typographical errors, or lack of review of the HIS by the radiologist—a potentially large number of cases were not collected. The nonstandardized documentation in the HIS forced many cases to be excluded due to lack of a proper patient history or undocumented urinalysis. Additionally, since noncontrast CT in the emergency setting is so rapidly performed, the clinician may forego the urinalysis if the CT provided a suitable diagnosis.
While our study suggests the use of intravenous contrast in patients meeting the criteria described, the decision must be made on a case-to-case basis and administering contrast agents does have certain disadvantages—increased initial time and cost, increased radiation, increased staffing requirement, and a small risk of adverse reactions—allergic reactions, extravasation, nephropathy [21,22,23]. Additionally, we assumed that intravenous contrast would optimize most studies. A majority of the alternative diagnoses can be established without contrast, and determining how optimal the study is remains subjective and varies for each case. A cost-benefit and risk-benefit analysis in addition to a follow-up large-scale study evaluating outcomes of the proposed algorithm would be useful.
Despite the limitations, the results of this study demonstrate that with all diagnostic outcomes considered, there is an overall improvement in diagnostic ability with contrast-enhanced CT in this population (95%, including negative cases, calculi greater than or equal to 3 mm, and alternative diagnoses) compared to noncontrast CT (85%, including negative cases and all calculi; p = .03). Only a small fraction (4%) of patients in the negative urinalysis and negative history subgroup had calculi that may be undetectable on a contrast-enhanced CT (less than 3 mm in size), all of which were nonobstructing and unlikely to be clinical significant [24, 25]. We propose the use of this screening method in cases of flank pain to improve appropriateness and utilization, improve diagnoses, and most importantly facilitate patient care.
Conclusion
The combination of urinalysis and patient history of urolithiasis can be utilized as a screening tool to direct referring physicians and protocoling radiologists to the appropriate study. In “rule-out” cases of flank pain with a negative urinalysis for hematuria and a negative history of urolithiasis, a contrast-enhanced CT may be more appropriate particularly given that 15% of these patients had alternative diagnoses suboptimally characterized without contrast and only 4% had calculi potentially difficult to detect in the setting of contrast.
References
Scales CD Jr, Smith AC, Hanley JM et al (2012) Prevalence of kidney stones in the United States. Eur Urol 62:160
Pearle MS, Calhoun EA, Curhan GC (2005) Urologic diseases in America project: urolithiasis. J Urol 173:848–857
Rucker CM, Menias CO, Bhalla S (2004) Mimics of renal colic: alternative diagnoses at unenhanced helical CT. Radiographics 24(suppl 1):S11–S28
Kitagawa M, Kotani T, Miyamoto Y, Kuriu Y, Tsurudome H, Nishi H, Yabe M, Otsuji E (2009) Noncontrast and contrast enhanced computed tomography for diagnosing acute appendicitis: a retrospective study for the usefulness. J Radiol Case Rep 3(6):26–33. https://doi.org/10.3941/jrcr.v3i6.101
Jang HJ, Lim HK, Lee SH, Kim EY, Kim SH (2000) Acute diverticulitis of the cecum and ascending colon: the value of thin-section helical CT findings in excluding colonic carcinoma. AJR Am J Roentgenol 174(5):1397–1402
DeStigter KK, Keating DP (2009) Imaging update: acute colonic diverticulitis. Clin Colon Rectal Surg 22(3):147–155. https://doi.org/10.1055/s-0029-1236158
Dym RJ, Duncan DR, Spektor M, Cohen HW, Scheinfeld MH (2014) Renal stones on portal venous phase contrast-enhanced CT: does intravenous contrast interfere with detection? Abdom Imaging 39(3):526–532
Bove P, Kaplan D, Dalrymple N et al (1999) Reexamining the value of hematuria testing in patients with acute flank pain. J Urol 162:685–687
Teichman JMH (2004) Acute renal calculus from ureteral calculus. N Engl J Med 350:684–693
Dalrymple N, Verga M, Anderson K et al (1998) The value of unenhanced helical computerized tomography in the management of acute flank pain. J Urol 159:735–740
Vieweg J, Chu T, Freed K et al (1998) Unenhanced helical CT for the evaluation of patients with acute flank pain. J Urol 160:679–684
Katz D, Scheer M, Lumerman J, Mellinger B, Stillman C, Lane M (2000) Alternative or additional diagnoses on unenhanced helical computed tomography for suspected renal colic: experience with 1000 consecutive examinations. Urology 56:53–57
Nachmann M, Harkaway R, Summerton S et al (2000) Helical CT scanning: the primary imaging modality for acute flank pain. Am J Emerg Med 18:649–652
Kanzaria HK, Hoffman JR, Probst MA, Caloyeras JP, Berry SH, Brook RH (2015) Emergency physician perceptions of medically unnecessary advanced diagnostic imaging. Acad Emerg Med 22(4):390–398
Drescher FS, Sirovich BE (2016) Use of computed tomography in emergency departments in the United States. JAMA Intern Med 176(2):273–275
Meltzer AC, Pines JM, Richards LM, Mullins P, Mazer-Amirshahi M (2017) US emergency department visits for adults with abdominal and pelvic pain 2007–13: trends in demographics, resource utilization and medication usage. Am J Emerg Med 35(12):1966–1969
Shoenfeld EM, Pekow PS, Shieh M, Scales CD, Lagu T, Lindenauer PK (2017) The diagnosis and management of patients with renal colic across a sample of US hospitals: high CT utilization despite low rates of admission and inpatient urologic intervention. PLoS One 12(1):e0169160
Raja AS, Mortele KJ, Hanson R, Sodickson AD, Zane R, Khorasani R (2011) Abdominal imaging utilization in the emergency department: trends over two decades. Int J Emerg Med 4:19
Rao VM, Levin DC, Parker L, Frangos AJ, Sunshine JH (2011) Trends in utilization rates of the various imaging modalities in emergency departments: nationwide Medicare data from 2000 to 2008. JACR 8(10):706–709
Bellolio MF, Heien HC, Sangaralingham LR, Jeffery MM, Campbell RL, Cabrera D, Shah ND, Hess EP (2017) Increased computed tomography utilization in the emergency department and its association with hospital admission. West J Emerg Med 18(5):835–845
Beckett KR, Moriarity AK, Langer JM (2015) Safe use of contrast media: what the radiologist needs to know. Radiographics 35(6):1738–1750
Anzai Y, Heilbrun ME, Haas D, Boi L, Moshre K, Minoshima S, Kaplan R, Lee VS (2017) Dissecting costs of CT study: application of TDABC (time-driven activity-based costing) in a tertiary academic center. Acad Radiol 24(2):200–208
Perisinakis K, Tzedakis A, Spanakis K, Papadakis AE, Hatzidakis A, Damilakis J (2018) The effect of iodine uptake on radiation dose absorbed by patient tissues in contrast enhanced CT imaging: implications for CT dosimetry. Eur Radiol 28(1):151–158
Dropkin BM, Moses RA, Sharma D, Pais VM Jr (2015) The natural history of nonobstructing asymptomatic renal stones managed with active surveillance. J Urol 193(4):1265–1269
Ordon M, Andonian S, Blew B, Shuler T, Chew B, Pace KT (2015) CUA guideline: management of ureteral calculi. Can Urol Assoc J 9(11–12):E837–E851
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Institutional Review Board approval was obtained for this retrospective study.
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
ESM 1
(XLSX 21 kb)
Rights and permissions
About this article
Cite this article
Desai, V., Cox, M., Deshmukh, S. et al. Contrast-enhanced or noncontrast CT for renal colic: utilizing urinalysis and patient history of urolithiasis to decide. Emerg Radiol 25, 455–460 (2018). https://doi.org/10.1007/s10140-018-1604-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-018-1604-0