Abstract
Background
Although the extent of resection frequently dictates the method of reconstruction following distal subtotal gastrectomy, it is unclear whether Roux-en-Y gastrojejunostomy compared with Billroth II gastrojejunostomy is associated with superior perioperative outcomes.
Methods
Patients who underwent resection for gastric cancer with Roux-en-Y or Billroth II reconstruction between 2000 and 2012 in seven academic institutions (US Gastric Cancer Collaborative) were identified. Patients who underwent total gastrectomy, gastric wedge, or palliative resections (metastatic disease or R2 resections) were excluded.
Results
Of a total of 965 patients, 447 met the inclusion criteria. A comparison between the Roux-en-Y (n = 257) and Billroth II (n = 190) groups demonstrated no differences in patient and tumor characteristics, except for Billroth II patients having a higher proportion of antral tumors (71 % vs. 50 %, p < 0.001). Roux-en-Y operations were slightly longer (244 min vs. 212 min, p < 0.001) and associated with somewhat higher blood loss (243 ml vs. 205 ml, p = 0.033). However, there were no significant differences in the length of hospital stay (8 days vs. 7 days), readmission rate (17 % vs. 18 %), 90-day mortality (5.1 % vs. 4.7 %), incidence (39 % vs. 41 %) and severity of complications, dependency on jejunostomy tube feeding at discharge (13 % vs. 12 %), same-patient decrease in serum albumin level from the preoperative to the postoperative value at 30, 60, and 90 days, receipt of adjuvant therapy (50 % vs. 53 %), or 5-year survival (44 % vs. 41 %).
Conclusions
Although long-term quality-of-life parameters were not compared, this study did not show an advantage of Roux-en-Y gastrojejunostomy over Billroth II gastrojejunostomy in short-term perioperative outcomes. Both techniques should be regarded as equally acceptable reconstructive options following partial gastrectomy for gastric cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastric cancer is the second leading cause of cancer-related death globally, accounting for nearly 10 % of all cancer-related deaths [1]. Surgery remains the cornerstone of treatment and provides the only chance for long-term survival. There are three ways to establish gastrointestinal continuity after gastrectomy: Billroth I (B1), Billroth II (B2), and Roux-en-Y (RY) reconstruction. The impact of the type of reconstruction after partial gastrectomy on perioperative outcomes has been a subject of intense study. Two prospective randomized trials from Japan have assessed outcomes between B1 and RY reconstructions after gastrectomy for gastric cancer, reporting variable results on perioperative morbidity and functional outcomes. In one study [2], both B1 and RY patients had similar weight loss (9.1 % vs. 9.7 %) and median albumin level (both 4.2 mg/dl; p = 0.18) 1 year after gastrectomy. However, the other study [3] showed the B1 group to have inferior postoperative outcomes, with higher rates of anastomotic leakage (5 % vs. 0 %), anastomotic stricture (6 vs. 1 %), intra-abdominal abscess (3 % vs. 0 %), and wound infection (5 % vs. 1 %). In addition, both studies showed the incidence of bile reflux gastritis to be higher in the B1 group (31 % vs. 21 % and 48 % vs. 26 %) on the basis of endoscopy performed 1 year postoperatively [2, 3]. Furthermore, a subsequent randomized trial of 159 patients from Korea comparing all three reconstruction types showed that although bile reflux gastritis was significantly less common 1 year after RY reconstruction (compared with B1 or B2 reconstruction), a comparison of quality-of-life and nutritional parameters 1 year postoperatively revealed no differences between the three groups [4]. Lastly, the latest results (12–21 years) of a prospective randomized study from Chile comparing B2 and RY reconstruction after gastrectomy for benign disease showed a higher incidence of gastroesophageal reflux symptoms after B2 reconstruction versus RY reconstruction (33 % vs. 3 %), endoscopic appearance of short-segment Barrett’s esophagus (25 % vs. 3 %), and histologically proven intestinal metaplasia (21 % vs. 3 %) [5].
Although B1 and RY reconstruction are preferable reconstruction techniques in Eastern countries [6, 7], B2 and RY reconstruction appear more prevalent choices in Western countries [8]. There has been no study from the West comparing surgical outcomes on the basis of the type of reconstruction after resection of gastric cancer. The objective of this study was to determine if the type of reconstruction after partial gastrectomy for gastric cancer has an impact on perioperative and long-term oncologic outcomes.
Methods
The study cohort included patients who underwent either RY reconstruction or B2 reconstruction after partial gastrectomy for gastric adenocarcinoma between 2000 and 2012 at one of seven academic centers participating in the US Gastric Cancer Collaborative: Emory University, Johns Hopkins University, Stanford University, Ohio State University, University of Wisconsin, Wake Forest University, and Washington University in St Louis. Data on patient demographics, clinicopathologic characteristics, perioperative outcomes, and overall survival were collected. Postoperative morbidity was graded with use of the modified Clavien-Dindo classification of surgical complications [9]. The seventh edition of the American Joint Committee on Cancer’s staging manual was used to determine the stage [10]. Patients were dichotomized into two groups on the basis of the type of reconstruction performed to restore gastrointestinal continuity after partial gastrectomy: RY versus B2 gastrojejunostomy. Partial gastrectomies include distal gastrectomy (less than 50 % of the stomach resected) and subtotal gastrectomy (more than 50 % of the stomach but not the entire stomach resected). The following patients were excluded from analysis: patients who underwent palliative resections (R2 or in the presence of stage 4 disease), patients who underwent total gastrectomy (as RY reconstruction is typically used in this case), patients who underwent wedge resection of the stomach (no reconstruction required), and patients who underwent B1 reconstruction.
Continuous variables are presented as mean and standard deviation and were compared by Student’s t test. Categorical variables are presented as observed counts and percentages within each subgroup and were compared by Pearson’s chi-square test or Fisher’s exact test. Comparisons of preoperative and postoperative albumin level changes (within the same patient) were calculated and compared by a paired t test. Survival time was calculated from the date of gastric resection to the date of death or last documented follow-up. Overall survival and the time to recurrence were calculated by the Kaplan–Meier method and compared by the log-rank test. Statistical analyses were performed with SPSS version 23.0 (IBM, Chicago, IL, USA) and STATA version 13.1 (StataCorp, College Station, TX, USA). Each participating site obtained institutional review board approval for this multi-institutional study.
Results
Demographic and preoperative characteristics
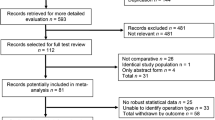
Of the 965 patients captured by the US Gastric Cancer Collaborative, the following patient groups were excluded: 398 patients who underwent total gastrectomy, 101 patients with stage 4 disease at presentation, 14 patients who underwent R2 resections, 12 patients who underwent wedge resections, and 17 patients who underwent B1 reconstruction. After exclusion of the aforementioned patients (some of them had overlapping exclusion criteria), 447 patients (47 %) met the inclusion criteria, with B2 reconstructions being performed in 190 patients (43 %) and RY reconstructions being performed in 257 patients (57 %); see Table 1. The demographic characteristics of patients who underwent RY and B2 reconstructions are detailed in Table 2. There were no differences in age, sex, American Society of Anesthesiologists class, comorbidities, and race between the B2 and RY groups. Preoperative nutritional status (i.e., albumin level) was similar between patients who underwent B2 reconstruction versus RY reconstruction. Slightly more patients in the RY group underwent preoperative neoadjuvant chemotherapy (17 % vs. 10 %, p = 0.032).
Operative and pathologic results
Subtotal gastrectomies were more commonly associated with RY reconstruction (78.6 % vs. 59.5 %, p < 0.001). Tumors of the antrum constituted 71 % of B2 reconstructions and 50 % of RY reconstructions (p < 0.001). Moreover, RY reconstruction was associated with a slightly longer operation time (mean 244 min vs. 212 min, p < 0.001) and intraoperative blood loss (243 ml vs. 205 ml, p = 0.033) than B2 reconstruction. Regardless of the type of reconstruction selected for restoration of gastrointestinal continuity, the number of lymph nodes harvested was marginally higher in the RY group than in the B2 group (range 0–63 lymph nodes vs. 0–42 lymph nodes; median 17 lymph nodes vs. 15 lymph nodes; mean 18 lymph nodes vs. 16 lymph nodes, p = 0.050); however, the rates of D2 lymphadenectomy (63.4 % vs. 61.9 %) and multivisceral resections (12.1 % vs. 13.2 %) were comparable. The rate of placement of feeding jejunostomy tubes was similar between the two groups.
There were no differences in the distribution of the American Joint Committee on Cancer stage, T category, and N category between the two groups. The rates of R0 resections (94.5 % vs. 91 %) were similar between the two groups. There were no differences in tumor differentiation, lymphovascular invasion, perineural invasion, and presence of signet ring cells; however, more patients in the RY group had diffuse histologic type (35.5 % vs. 22.4 %, p = 0.015).
Postoperative outcomes
Postoperative outcomes between RY and B2 reconstructions are shown in Table 3. The rates of any complication, a major complication (Clavien grade 3 or more), 30 and 90-day mortality, and reoperation were similar between the two groups. Of the 22 % of patients who had a jejunostomy tube placed intraoperatively, there were no differences in the proportion of patients who were discharged with long-term tube feeding (13 % vs. 12 %, p = 0.109). The rates of postoperative adjuvant therapy were similar between the two groups (50.2 % vs. 53.3 %, p = 0.530).
To control for the fact that sometimes the method of reconstruction is dictated by the extent of gastric resection (surgeons would more commonly perform RY reconstruction after subtotal gastrectomy and B2 reconstruction after distal gastrectomy), we performed subgroup analyses separately on distal gastrectomy and subtotal gastrectomy patients (Table 4). This demonstrated no differences in postoperative morbidity, mortality, or decline in nutritional status (i.e., postoperative decrease in serum albumin level) between patients undergoing either RY reconstruction or B2 reconstruction.
Survival analysis
Overall survival between RY and B2 groups was comparable (5-year overall survival rate 44 % vs. 40.7 %, p = 0.177; Fig. 1a). Similarly, the time to recurrence was similar between the two groups (p = 0.121; Fig. 1b. When we stratified survival by stage, there were no differences in survival between patients who underwent B2 reconstruction and patients who underwent RY reconstruction: Stage 1 (5-year overall survival rate 69.6 % vs. 51.1 %, p = 0.454), Stage 2 (5-year overall survival rate 36.7 % vs. 48.1 %, p = 0.096), and Stage 3 (5-year overall survival rate 25.1 % vs. 32.3 %, p = 0.440).
Discussion
This is the first multi-institutional study from the West evaluating outcomes of gastric cancer resection on the basis of the type of reconstruction performed to restore gastrointestinal continuity. The results of the study suggest that RY reconstruction after partial gastrectomy for gastric cancer has perioperative outcomes similar to those of B2 reconstruction in terms of morbidity, mortality, and nutritional impairment. As expected, important oncologic surrogates of the quality of resection such as the extent of lymphadenectomy, and margin status remain similar regardless of the type of gastrointestinal reconstruction, a fact that most likely accounts for the similar long-term outcomes (survival and recurrence) noted between the two groups.
Postoperative complications leading to malnutrition, such as delayed gastric emptying, anastomotic leak, or dumping syndrome, may require enteral nutritional support, prolong hospital stay, and increase health care costs [11]. In the present study, nutritional status, as measured by the postoperative decline in serum albumin level at 30, 60, and 90 days within the same patient, was equally affected by RY reconstruction or B2 reconstruction. This observation held true on separate subset analyses for distal and subtotal gastrectomy patients. Similarly, in a prospective randomized study of 159 gastrectomy patients who underwent B1, B2, or RY reconstruction, Lee et al. [4] found a comparable impact of the three reconstruction methods on nutritional parameters (albumin level, protein level, total lymphocyte count, transferrin level, body weight, and body mass index) measured at 3, 6, 12, and 24 months postoperatively. In another randomized trial, Csendes et al. [5] found that there were no differences in the rates of postgastrectomy diarrhea (9.1 % vs. 9.7 %), dumping syndrome (6 % vs. 3.2 %), and weight gain (78.8 % vs. 90.3 %) between patients who underwent either B2 reconstruction or RY reconstruction. Although our retrospective registry did not include information specifically on delayed gastric emptying, dumping syndrome, diarrhea, body weight, or relevant quality-of-life parameters, we used the length of hospital stay, discharge destination, readmission, and dependency on jejunostomy tube feeding on discharge to indirectly evaluate patients for potential postoperative gastrointestinal dysfunction. We found all of the aforementioned parameters to be similar in our study irrespective of the reconstruction method used.
The comparison of RY reconstruction versus B2 reconstruction has previously been addressed in two studies evaluating restoration of gastrointestinal continuity after pancreaticoduodenectomy. A retrospective study from Memorial Sloan Kettering Cancer Center comparing 122 patients who underwent RY reconstruction with 588 patients who underwent classic B2 reconstruction after pancreaticoduodenectomy found no difference in the rates of delayed gastric emptying (10.1 % vs. 10.3 %), reoperation (9.1 % vs. 6.9 %), and interventional radiology procedures (9.8 % vs. 6.8 %), length of hospital stay (11 days vs. 10 days), or mortality (0.9 % vs. 2.6 %) between the two groups [12]. In fact, in a prospective randomized trial of 101 patients who underwent pancreaticoduodenectomy, Shimoda et al. [13] actually found higher rates of delayed gastric emptying after RY reconstruction than after B2 reconstruction (20.4 % vs. 5.7 %), and concluded that B2 reconstruction may be a better reconstructive option. These studies do not support the routine use of RY reconstruction after pancreaticoduodenectomy and reinforce our findings that RY reconstruction may not be superior to B2 reconstruction after gastrectomy, at least in the short term.
Bile reflux gastritis associated with B2 reconstruction after distal gastrectomy has been strongly correlated with carcinogenesis in the gastric remnant, as well as in the setting of Barrett’s esophagus. [5] Our retrospective study did not specifically examine this issue, but given the long latency period (sometimes decades) before the development of gastric remnant cancer, it is reasonable to advocate RY reconstruction in younger patients with early gastric cancer who have a long life expectancy, thereby being at risk of metachronous gastric remnant cancer.
There are several limitations to this retrospective study. It is difficult to identify intraoperative factors that may have influenced the decision to proceed with RY versus B2 reconstruction, introducing significant selection bias. Second, given the multi-institutional nature of our study, important technical aspects employed during reconstruction, including stapled versus hand-sewn anastomosis, isoperistaltic versus antiperistaltic anastomosis, the choice of antecolic versus retrocolic routes, the addition of a Braun anastomosis to a B2 reconstruction (which would make it a functional RY reconstruction), the exact percentage of stomach remaining after gastrectomy, and length of the Roux limb, may have differed by institution and surgeon, but were not available for analysis. Similarly, it was not feasible to collect long-term quality-of-life measures, although we acknowledge that such information would have been extremely helpful for the purposes of this study. Furthermore, it is difficult to discern retrospectively whether specific complications were directly related to the type of reconstruction performed; however, one of our main findings was that the rate of any morbidity or a serious morbidity was comparable between the two groups. Lastly, the exact findings of postoperative endoscopic surveillance (specifically in regard to alkaline gastritis) and perhaps the incidence of aspiration pneumonia secondary to bile reflux were also not recorded, but could have shed light on the differing incidence of this phenomenon after various types of postgastrectomy reconstruction as reported by others.
Conclusion
Despite the presumed theoretical advantage of RY gastrojejunostomy over B2 gastrojejunostomy with regard to bile reflux gastritis, and its potential disadvantage because of the need for an additional anastomosis, this multi-institutional study did not reveal any differences based on the type of reconstruction after partial gastrectomy in the rate and distribution of postoperative complications, postoperative mortality, length of stay, dependency on enteral feeding, discharge destination, readmission, and decline in albumin level. In regard to short-term perioperative outcomes, RY and B2 reconstruction can be considered as equally acceptable restorative options following partial gastrectomy for gastric cancer.
References
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–917.
Hirao M, Takiguchi S, Imamura H, Yamamoto K, Kurokawa Y, Fujita J, et al. Comparison of Billroth I and Roux-en-Y reconstruction after distal gastrectomy for gastric cancer: one-year postoperative effects assessed by a multi-institutional RCT. Ann Surg Oncol. 2013;20:1591–7.
Kojima K, Yamada H, Inokuchi M, Kawano T, Sugihara K. A comparison of Roux-en-Y and Billroth-I reconstruction after laparoscopy-assisted distal gastrectomy. Ann Surg. 2008;247:962–7.
Lee MS, Lee HJ, Kim HH, Ahn SH, Lee JH, Park DJ, et al. What is the best reconstruction method after distal gastrectomy for gastric cancer? Surg Endosc. 2012;26:1539–47.
Csendes A, Burgos AM, Smok G, Burdiles P, Braghetto I, Diaz JC. Latest results (12–21 years) of a prospective randomized study comparing Billroth II and Roux-en-Y anastomosis after a partial gastrectomy plus vagotomy in patients with duodenal ulcers. Ann Surg. 2009;249:189–94.
Xiong JJ, Altaf K, Javed MA, Nunes QM, Huang W, Mai G, et al. Roux-en-Y versus Billroth I reconstruction after distal gastrectomy for gastric cancer: a meta-analysis. World J Gastroenterol. 2013;19:1124–34.
Hoya Y, Mitsumori N, Yanaga K. The advantages and disadvantages of a Roux-en-Y reconstruction after a distal gastrectomy for gastric cancer. Surg Today. 2009;39:647–51.
Chin AC, Espat NJ. Total gastrectomy: options for the restoration of gastrointestinal continuity. Lancet Oncol. 2003;4:271–6.
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250:187–96.
Edge SB, American Joint Committee on Cancer, American Cancer Society. AJCC cancer staging manual. New York: Springer; 2010.
Chima CS, Barco K, Dewitt ML, Maeda M, Teran JC, Mullen KD. Relationship of nutritional status to length of stay, hospital costs, and discharge status of patients hospitalized in the medicine service. J Am Diet Assoc. 1997;97:975–8; quiz 979–80.
Grobmyer SR, Hollenbeck ST, Jaques DP, Jarnagin WR, DeMatteo R, Coit DG, et al. Roux-en-Y reconstruction after pancreaticoduodenectomy. Arch Surg. 2008;143:1184–8.
Shimoda M, Kubota K, Katoh M, Kita J. Effect of Billroth II or Roux-en-Y reconstruction for the gastrojejunostomy on delayed gastric emptying after pancreaticoduodenectomy: a randomized controlled study. Ann Surg. 2013;257:938–42.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All participating institutions obtained institutional review board approval for this retrospective study. The research was performed in accordance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
T. B. Tran and D. J. Worhunsky contributed equally to this article.
Rights and permissions
About this article
Cite this article
Tran, T.B., Worhunsky, D.J., Squires, M.H. et al. To Roux or not to Roux: a comparison between Roux-en-Y and Billroth II reconstruction following partial gastrectomy for gastric cancer. Gastric Cancer 19, 994–1001 (2016). https://doi.org/10.1007/s10120-015-0547-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-015-0547-3