Summary
Aim
The aim of this study was to assess and validate the clinical efficacy of Roux-en-Y reconstruction (R-Y) when compared to Billroth I reconstruction (B-I) after distal gastrectomy (DG).
Methods
The authors identified the prospective, randomized, controlled trials comparing R‑Y with B‑I after DG for gastric cancer from January 1990 to July 2016 using PubMed, Web of Knowledge, Ovid’s database. The method of meta-analysis is performed to compare the complications and recurrences of R‑Y versus B‑I.
Result
Seven randomized controlled trials (RCTs) involving 1197 patients were included. Meta-analysis revealed that R‑Y reconstruction was associated with a significant reduction in the incidence of remnant gastritis (Odds ratios [OR] 2.58, 95%Confidence interval [CI]: 1.78, 3.74; P < 0.00001). No significant differences were observed between the groups in terms of intraoperative blood loss (Weighted mean difference [WMD] −20.97, 95%CI: −47.85, 5.92; P = 0.13), time to resumed oral intake (WMD −1.32, 95%CI: −6.39, 3.75; P = 0.61), reflux esophagitis (OR 1.71, 95%CI: 0.82, 3.57; P = 0.15), and recurrence (OR 1.10, 95%CI: 0.44, 2.71; P = 0.84). Moreover, the B‑I reconstruction method took significantly less time to perform as compared to R‑Y reconstruction (WMD −38.12, 95%CI: −50.50, −25.74; P < 0.00001) and postoperative hospital stay was shorter (WMD −2.96, 95%CI: −5.93, 0.00; P = 0.05),
Conclusion
The R‑Y reconstruction was effective in preventing gastritis, although R‑Y reconstruction after gastric resection was inferior to B‑I reconstruction in terms of taking more time to perform and a longer stay in hospital.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Both Billroth I (B-I) reconstruction and Roux-en-Y reconstruction (R-Y) have commonly been performed after distal gastrectomy (DG) [1, 2]. Patients after gastrectomy typically display good clinical course. However, dyspepsia and gastrointestinal reflux usually occur after these procedures, and may cause remnant gastritis, remnant gastric ulcer, and reflux esophagitis [3,4,5].
In recent years, attention for gastrointestinal and esophageal reflux has also been strongly considered when choosing a surgical technique [6]. Control of acid reflux is generally regarded as the essential physiological principle that directly influences the quality of life of patients after surgery. R‑Y has been attempted in order to prevent bile and pancreatic secretion from reaching the gastric mucosa, and to prevent postoperative alkaline reflux gastritis or esophagitis after DG [7]. However, the procedure is technically more difficult and complex than the B‑I procedure. Indeed, because an additional anastomosis is required in the R‑Y procedure, the number of postoperative complications might be expected to be increased.
To our knowledge, there are two existing meta-analysis [8, 9] comparing the outcome of B‑I with R‑Y. However, both of them included a small number of studies and the latest one was published 3 years ago. With an increasing number of new publications on this controversial subject in recent years, we conducted a systematic review and meta-analysis to compare the benefits and drawbacks following DG between B‑I and R‑Y by reviewing the current literature.
Materials and methods
Search strategy
PubMed, Web of Knowledge, and Ovid’s database were searched from January 1990 to June 2016 without language restrictions. The search terms used were “Roux-en-Y,” “Billroth I,” “distal gastrectomy,” and “randomized clinical trial.” The reference lists of relevant studies were checked manually to locate any missing studies.
Study selection
Identified studies were assessed for eligibility for inclusion in the review by scrutinizing the titles, abstracts, and keywords of every record retrieved. Studies were restricted to those published in English and Chinese. Clinical studies concerning comparisons of any aspects between the B‑I and R‑Y for DG were also included.
Data extraction
Two coauthors (LY and LH) independently selected studies for inclusion and exclusion and reached consensus when they did not agree in the initial assignment. The following variables were recorded: authors, journal and year of publication, number of patients, age, operation time, blood loss, postoperative hospital stay, time to resumed oral intake, reflux esophagitis, remnant gastritis, and recurrence. If necessary, the corresponding authors of studies were contacted to obtain supplementary information.
Quality assessment
The quality of the trials was assessed in the light of Cochrane Handbook for Systematic Reviews of Interventions version 5.1.0 [10]. The scale consists of three items, such as randomization, blinding, and description of the withdrawals and dropouts. Studies with a score of 3–5 were considered to be of high quality.
Statistical analysis
A formal meta-analysis was carried out for all included studies comparing the results of B‑I and R‑Y for distal gastrectomy. The outcomes in our study were operation time, blood loss, postoperative hospital stay, time to resumed oral intake, reflux esophagitis, remnant gastritis, and recurrence. Pooled estimates of outcomes were calculated using a fixed-effects model, but a randomized-effects model was used according to heterogeneity. Heterogeneity was explored using I2 statistics, a measure of how much the variance between studies can be attributed to inter-study differences rather than chance. I2 > 50% was regarded to indicate strong heterogeneity. The Cochrane Collaboration’s Review Manager Software version 5.0 (The Cochrane Collaboration, Oxford, UK) was utilized for the data analysis.
Results
Study selection
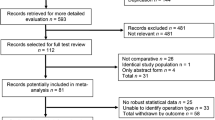
314 potentially relevant articles comparing B‑I and R‑Y after DG for gastric malignancies were found (Fig. 1). After exclusion of duplicate references, non-relevant literature, and those that did not satisfy inclusion criteria, 25 candidate articles were considered for the meta-analysis. After careful review of the full text of these articles, 7 studies [11,12,13,14,15,16,17,18] were included. The study characteristics are summarized in Tables 1, 2 and 3.
Patient demographics for the 7 studies are presented in Table 1. All papers were randomized clinical trials. The publication dates ranged from January 1990 to July 2016. Study sizes ranged from 45 to 332 patients.
Outcome measures
A total of 1197 patients who underwent B‑I and R‑Y were analyzed. To date, 7 randomized controlled trials (RCTs) have been undertaken to compare R‑Y with B‑I reconstruction. All studies had a clear description of the sample size calculation and were found to be of high quality according to the Jadad scoring system. The detailed results of meta-analysis are given in Figs. 2, 3, 4, 5, 6, 7 and 8. Meta-analysis revealed that R‑Y reconstruction was associated with a significant reduction in the incidence of remnant gastritis (Odds ratio [OR] 2.58, 95%Confidence interval [CI]: 1.78, 3.74; P < 0.00001). No significant differences were observed between the groups in terms of intraoperative blood loss (Weighted mean difference [WMD] −20.97, 95%CI: −47.85, 5.92; P = 0.13), time to resumed oral intake (WMD −1.32, 95%CI: −6.39, 3.75; P = 0.61), reflux esophagitis (OR 1.71, 95%CI: 0.82, 3.57; P = 0.15), and recurrence (OR 1.10, 95%CI: 0.44, 2.71; P = 0.84). Moreover, the B‑I reconstruction method took significantly less time to perform as compared to R‑Y reconstruction (WMD −38.12, 95%CI: −50.50, −25.74; P < 0.00001) and postoperative hospital stay was significantly shorter in the B‑I group than in the R‑Y group (WMD −2.96, 95%CI: −5.93, 0.00; P = 0.05).
Forest plot of the comparison of time to resumed oral intake for B‑I vs. R‑Y. B‑I Billroth‑I, R‑Y Roux-en‑Y, SD standard deviation, CI confidence interval, green elements weighted mean difference (WMD) showing that B‑I results in a shorter time to resumed oral intake than R‑Y, but no significant differences are observed
Our review of 3 RCTs [13, 14, 16], involving nearly 500 patients, showed that body weight loss was not different between the two groups. Rates of change in total protein, serum albumin, and total cholesterol levels were similar between the two groups [13, 14, 16]. On the other hand, according to Tanaka’s [18] opinion, the visceral fat loss in the BMI ≥ 22.5 kg/m2 group for R‑Y was greater than for B‑I reconstruction.
Discussion
The choice of reconstruction method after DG remains controversial. The ideal gastrointestinal reconstruction procedure should minimize postoperative morbidity and improve quality of life [19]. To our knowledge, B‑I reconstruction has usually been applied after DG for gastric cancer due to its simplicity and shorter operating time.
We evaluated data regarding intraoperative blood loss and time to resumed oral intake, and no significant difference in either of these parameters between the two groups was found. It may be largely due to the use of gastrointestinal stapling devices and the refinement of technique.
The Roux-en-Y stasis syndrome is characterized by symptoms of upper gut stasis after Roux-en-Y gastrojejunostomy [3, 15], and it is generally thought to be caused by the fact that the Roux limb is separated from the natural small bowel pacemaker, which was located in the proximal duodenum. In terms of the postoperative course, the R‑Y group showed a significantly higher frequency of nausea and vomiting as well as a longer postoperative hospital stay compared to the B‑I group [11].
B-I is more commonly performed in Eastern countries because of its simplicity. The R‑Y operation is reported to be superior to the conventional B‑I reconstructions in preventing bile reflux into the gastric remnant and in preventing impeding gastritis [20]. Previous studies indicated that the R‑Y procedure was more effective at preventing postoperative reflux esophagitis [3, 21]. In contrast, several studies [7, 13, 14, 16] illustrated that there was no significant difference in reflux esophagitis between the two groups. Our meta-analysis demonstrated that B-I was more likely to occur remnant gastritis. This may attribute to the absence of the pyloric sphincter, which allows reflux of duodenal contents into the remnant stomach [22]. It is important to state that reflux of duodenal contents into the esophagus is strongly associated with Barrett’s esophagus or esophageal cancer and remnant stomach cancer after gastrectomy [23,24,25].
The omega loop gastric bypass (OLGB) has become a very commonly performed bariatric procedure, because it might be a promising procedure, simpler, quicker, and safer with similar efficacy in comparison to R‑Y. Whether OLGB increased the reflux of bile into the gastric pouch and into the esophagus is controversial [26]. However, OLGB consists of a long narrow vertical gastric pouch, thus, reflux into the esophagus is not believed to be an OLGB-specific problem. By contrast, the B‑I lacks a long narrow gastric pouch and reflux esophagitis is more likely. In OLGB and Billroth II (B-II), the most important parallel is the single anastomosis bypass of the duodenum without a Roux limb. The OLGB distance of the gastrojejunostomy to the esophagus is longer than in Billroth II.
Recurrence was important for evaluating the oncological benefit of surgical intervention when lacking of compromising post-operative survival. When the primary lesion has directly invaded the duodenum or head of the pancreas, B‑I is more likely to result in local recurrence than R‑Y near the anastomosis. This result was confirmed by Langhans et al. [27]. On the contrary, there were no differences between the two groups in terms of recurrence. As only two included studies [16, 18] covered the recurrence, and none of them mentioned the invasion of duodenum or head of the pancreas, the bias was inevitable.
There is no difference in the postoperative nutritional status between reconstructive procedures, despite the fact that R‑Y reconstruction might be a better choice for obese patients who require distal gastrectomy to treat gastric cancer.
This review has some limitations and hence the results should be interpreted with a degree of caution. Firstly, several important outcomes including remnant gastritis and reflux esophagitis have not been reported adequately in the RCTs. Secondly, there is no standard definition for recurrence in the literature. It is important to mention that we were unable to analyze important outcomes including quality of life and incidence of gastric carcinoma in the gastric remnant due to lack of available data. We would therefore propose well-designed RCTs with adequate follow-up and emphasis on assessing important outcomes to clarify ambiguities surrounding the use of these reconstruction methods.
Conclusions
The R‑Y reconstruction was effective in preventing gastritis and esophagitis, although R‑Y reconstruction after gastric resection was inferior to BI reconstruction in terms of taking more time to perform and length of stay in hospital. However, the results of the present study should be verified by long-term follow-up of these patients and additional randomized control studies are warranted to determine the clinical efficacy of R‑Y reconstruction in DG.
References
Yoshino K. History of gastric cancer surgery. Nihon Geka Gakkai Zasshi. 2000;101:855–60.
Weil PH, Buchberger R. From Billroth to PCV: a century of gastric surgery. World J Surg. 1999;23:736–42.
Fukuhara K, Osugi H, Takada N, Takemura M, Higashino M, Kinoshita H. Reconstructive procedure after distal gastrectomy for gastric cancer that best prevents duodenogastroesophageal reflux. World J Surg. 2002;26:1452–7.
Osugi H, Fukuhara K, Takada N, Takemura M, Kinoshita H. Reconstructive procedure after distal gastrectomy to prevent remnant gastritis. Hepatogastroenterology. 2004;51:1215–8.
Kauer WK, Peters JH, DeMeester TR, Feussner H, Ireland AP, Stein HJ, et al. Composition and concentration of bile acid reflux into the esophagus of patients with gastroesophageal reflux disease. Surgery. 1997;122:874–81.
Kiesslich R, Kanzler S, Vieth M, Moehler M, Neidig J, Thanka Nadar BJ, et al. Minimal change esophagitis: prospective comparison of endoscopic and histological markers between patients with non-erosive reflux disease and normal controls using magnifying endoscopy. Dig Dis. 2004;22:221–7.
Kojima K, Yamada H, Inokuchi M, Kawano T, Sugihara K. A comparison of Roux-en-Y and Billroth-I reconstruction after laparoscopy-assisted distal gastrectomy. Ann Surg. 2008;247:962–7.
Xiong JJ, Altaf K, Javed MA, et al. Roux-en-Y versus Billroth I reconstruction after distal gastrectomy for gastric cancer: a meta-analysis. World J Gastroenterol. 2013;19:1124–34.
Zong L, Chen P. Billroth I vs. Billroth II vs. Roux-en-Y following distal gastrectomy: a meta-analysis based on 15 studies. Hepatogastroenterology. 2011;58(109):1413–24.
Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011.
Imamura H, Takiguchi S, Yamamoto K, Hirao M, Fujita J, Miyashiro I, et al. Morbidity and mortality results from a prospective randomized controlled trial comparing Billroth I and Roux-en-Y reconstructive procedures after distal gastrectomy for gastric cancer. World J Surg. 2012;36(3):632–7.
Hirao M, Takiguchi S, Imamura H, Yamamoto K, Kurokawa Y, Fujita J, et al. Comparison of Billroth I and Roux-en-Y reconstruction after distal gastrectomy for gastric cancer: one-year postoperative effects assessed by a multi-institutional RCT. Ann Surg Oncol. 2013;20(5):1591–7.
Ishikawa M, Kitayama J, Kaizaki S, Nakayama H, Ishigami H, Fujii S, et al. Prospective randomized trial comparing Billroth I and Roux-en-Y procedures after distal gastrectomy for gastric carcinoma. World J Surg. 2005;29(11):1415–20. discussion 1421.
Lee MS, Ahn SH, Lee JH, Park DJ, Lee HJ, Kim HH, et al. What is the best reconstruction method after distal gastrectomy for gastric cancer? Surg Endosc. 2012;26(6):1539–47.
Montesani C, D’Amato A, Santella S, Pronio A, Giovannini C, Cristaldi M, et al. Billroth I versus Billroth II versus Roux-en-Y after subtotal gastrectomy. Prospective [correction of prespective] randomized study. Hepatogastroenterology. 2002;49(47):1469–73.
Nakamura M, Nakamori M, Ojima T, Iwahashi M, Horiuchi T, Kobayashi Y, et al. Randomized clinical trial comparing long-term quality of life for Billroth I versus Roux-en-Y reconstruction after distal gastrectomy for gastric cancer. Br J Surg. 2016;103(4):337–47.
Takiguchi S, Yamamoto K, Hirao M, Imamura H, Fujita J, Yano M, et al. A comparison of postoperative quality of life and dysfunction after Billroth I and Roux-en-Y reconstruction following distal gastrectomy for gastric cancer: results from a multi-institutional RCT. Gastric Cancer. 2012;15(2):198–205.
Tanaka K, Takiguchi S, Miyashiro I, Hirao M, Yamamoto K, Imamura H, et al. Impact of reconstruction method on visceral fat change after distal gastrectomy: results from a randomized controlled trial comparing Billroth I reconstruction and roux-en-Y reconstruction. Surgery. 2014;155(3):424–31.
Piessen G, Triboulet JP, Mariette C. Reconstruction after gastrectomy: which technique is best? J Visc Surg. 2010;147:e273–e83.
Fukuhara K, Osugi H, Takada N, Takemura M, Ohmoto Y, Kinoshita H. Quantitative determinations of duodenogastric reflux, prevalence of Helicobacter pyroli infection, and concentrations of interleukin-8. World J Surg. 2003;27:567–70.
Shinoto K, Ochiai T, Suzuki T, Okazumi S, Ozaki M. Effectiveness of Roux-en-Y reconstruction after distal gastrectomy based on an assessment of biliary kinetics. Surg Today. 2003;33:169–77.
Kubo M, Sasako M, Gotoda T, Ono H, Fujishiro M, Saito D, et al. Endoscopic evaluation of the remnant stomach after gastrectomy: proposal for a new classification. Gastric Cancer. 2002;5:83–9.
Sato T, Miwa K, Sahara H, Segawa M, Hattori T. The sequential model of Barrett’s esophagus and adenocarcinoma induced by duodeno-esophageal reflux without exogenous carcinogens. Anticancer Res. 2002;22:39–44.
Wetscher GJ, Hinder RA, Smyrk T, Perdikis G, Adrian TE, Profanter C. Gastric acid blockade with omeprazole promotes gastric carcinogenesis induced by duodenogastric reflux. Dig Dis Sci. 1999;44:1132–5.
Namikawa T, Kitagawa H, Okabayashi T, Sugimoto T, Kobayashi M, Hanazaki K. Double tract reconstruction after distal gastrectomy for gastric cancer is effective in reducing reflux esophagitis and remnant gastritis with duodenal passage preservation. Langenbecks Arch Surg. 2011;396:769–76.
Fisher BL, Buchwald H, Clark W, Champion JK, Fox SR, MacDonald KG, et al. Mini-gastric bypass controversy. Obes Surg. 2001;11:773–7.
Langhans P, Heger RA, Stegemann B. The cancer risk in the stomach subjected to nonresecting procedures. An experimental long-term study. Scand J Gastroenterol Suppl. 1984;92:138–41.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
H. Liu and Y. Li declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Liu, H., Li, Y. Roux-en-Y versus Billroth I following distal gastrectomy. Eur Surg 50, 202–208 (2018). https://doi.org/10.1007/s10353-018-0532-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10353-018-0532-2