Abstract
The literature on the efficacy of erbium lasers for nonsurgical periodontal therapy is inconsistent. The objective of the umbrella review was to collate the information available in the systematic reviews to provide a comprehensive synthesis of clinical and patient reported outcomes following the use of erbium lasers for non-surgical periodontal therapy. An electronic database search was carried out, and systematic reviews/meta-analyses which assessed the efficacy of erbium lasers as monotherapy or as an adjunct to scaling and root planing were included. The methodological quality and reporting quality of the included studies were assessed. 15 Systematic reviews/meta-analyses were obtained after title, abstract, and full text search. The meta-analyses data revealed a clinical attachment level gain, reduction in probing pocket depth at 1 and 3-month follow-up, and no additional benefit at ≥ 6-month follow-up in the erbium laser group. The evidence gap map revealed lack of clinical outcome data at > 6-month follow-up and dearth in studies assessing patient reported outcome measures and adverse events. Erbium lasers may provide short-term clinical benefits, and further studies with standardized laser parameters evaluating long-term follow-up, patient-reported outcome measures, and adverse events are needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Periodontal disease is a chronic condition of bacterial origin that is characterized by inflammation of the supporting structures of the tooth [1]. The prevalence of periodontitis ranges between 20 and 50% [2], and it is reported to be the 11th most prevalent condition in the world [3]. The recent evidence-based 2017 classification of periodontal diseases had proposed a multi-dimensional staging and grading system of periodontitis that includes both chronic and aggressive forms of the disease [4]. Non-surgical periodontal therapy (NSPT) is recommended for the debridement of plaque and calculus as the initial step in the management of periodontitis [5]. Advances in technology such as the erbium lasers have revolutionized the approach to non-surgical periodontal therapy. According to the consensus statement of the 6th European Workshop in Periodontology, erbium lasers, among all other available lasers, may be considered as the most suitable for NSPT [5]. The erbium family of lasers includes the erbium:YAG (2,940 nm) and erbium, chromium:YSGG lasers (2,780 nm), both of which have shown high absorption in water and hydroxyapatite, which facilitates the effective removal of calculus from the root surface without deleterious effects [6].
The American Dental Association published clinical practice guidelines on the non-surgical treatment of chronic periodontitis by SRP with or without adjunctive therapy [7]. Sub-antimicrobial-dose doxycycline (SDD), systemic antimicrobials, chlorhexidine chips, and photodynamic therapy with diode lasers all had beneficial effects with moderate levels of certainty when used as adjuncts [8]. Erbium lasers have been used as monotherapy/adjunct to SRP, with various outcomes being reported in the literature [9, 10]. Patient-reported outcomes have also been found to favor the use of erbium lasers in NSPT [11].
The amalgamation of scientific evidence with personal clinical expertise and patient needs/preferences forms the core of evidence-based dentistry. Systematic reviews (SR) and meta-analysis (MA) represent the highest level of evidence in research and pave the way for the formulation of clinical practice guidelines. Numerous systematic reviews have been published on the effectiveness of erbium lasers for NSPT [12,13,14,15]. Variations in the laser parameters used, time points of assessment, methods of usage, and use as monotherapy/adjunct to SRP have contributed to heterogeneity in the outcomes reported in the systematic reviews [16, 17]. The need of the hour is to obtain a critical insight into whether the use of erbium lasers in NSPT is clinically effective and predictable. Hence, this umbrella review aimed to collate the information available in systematic reviews to provide a comprehensive synthesis of clinical and patient-reported outcomes following the use of erbium lasers in NSPT.
Methods
Systematic collection and evaluation of multiple SR/MA were performed to create a standardized, accessible, and applicable document. The study protocol for the umbrella review was registered at the International Prospective Register of Systematic Reviews — PROSPERO (Ref No: CRD42020156118) [Registered on 28 April 2020]. A revision to this protocol was uploaded on 13 February 2021. This umbrella review addresses the specific research question on the use of erbium lasers in non-surgical periodontal therapy.
Search strategy
The search was performed by two independent reviewers in databases such as Medline via PubMed, EMBASE, Cochrane Database of Systematic Reviews, Science Direct, Google Scholar, LILACS, and Open Grey to include high-impact journals as well as grey literature.
The following keywords and the Boolean operators “AND” and “OR” were used to filter the information: (Laser solid state OR erbium laser) AND (non-surgical periodontal therapy OR scaling and root planing OR dental scaling) AND (periodontitis) AND (systematic review OR meta-analysis) NOT (letter OR newspaper article) (Supplementary Fig. 1).
In addition to the above search strategy, the following search combinations were used in PubMed to narrow the list of included studies:
-
#1 “Lasers, Solid-State” [MeSH] OR “Erbium” [MeSH] OR “Lasers” [MeSH].
-
#2 “scaling root planing” OR “Dental Scaling” [MeSH] OR “Root Planing” [MeSH] OR non-surgical periodontal therapy”.
-
#3 “Periodontitis” [MeSH] OR “Chronic Periodontitis” [MeSH].
-
#4 systematic reviews [MeSH] OR meta analysis [MeSH].
-
#5 #1AND#2AND#3AND#4.
Initially, two investigators (VL, DK) independently evaluated titles and abstracts to select probable articles. After all duplicate references were excluded, the remaining articles were reviewed in full text. References from the full-text articles were screened to identify eligible papers. Any disagreements were resolved by a consensus involving a third investigator [MM].
Inclusion and exclusion criteria
The time frame of the included studies was between January 2000 and January 2021, and only articles in English were selected. Systematic reviews with or without meta-analysis involving human subjects and comparing erbium lasers alone or as an adjunct to SRP vs conventional approaches to non-surgical periodontal therapy were included. Gain in clinical attachment level (CAL) was considered as the primary outcome, while secondary outcomes included probing pocket depth (PPD) reduction, reduction in overall or specific microbial counts in the sub-gingival pocket area, and patient-related outcome measures (PROM). Systematic reviews that documented changes in the primary outcomes recorded at baseline and at least 3 months after interventions were included in this umbrella review. Systematic reviews involving animal studies, in vitro studies, other types of lasers (Nd:YAG/diode/photodynamic therapy/photobiomodulation), narrative reviews, consensus reports, and position papers were excluded.
Data extraction
All authors had access to the data throughout the study, and the following parameters were extracted prior to review: author name(s), year of publication, period during which the included original studies were published, sources searched, objectives, number of studies, number of participants, types of study design included, instrument of quality assessment used, interventions, control(s), laser settings, method of statistical analysis, heterogeneity, outcomes assessed, and study observations. Data extraction was performed by VL and DD.
Quality assessment and assessment of risk of bias
An assessment of the validity of the results presented in systematic reviews was critical for the recommendations and was performed by the Risk Of Bias In Systematic Reviews (ROBIS) tool. Each systematic review was assessed independently by two investigators (VL, AM) using the three phases of the ROBIS tool: (A) assessment of relevance, (B) identification of concerns with the review process, and (C) judgment of the risk of bias in the review. The second phase involves four domains: assessment of study eligibility (Domain 1), identification and selection of studies (Domain 2), data selection and study appraisal (Domain 3 — risk of bias), and synthesis and findings (Domain 4) critical to the minimization of bias. Risk of bias was determined as low/high/unclear based on the interpretation of the four domains.
Statistical analysis
Pooled data from the outcomes were analyzed to generate a forest plot. Corrected covered areas (CCA) analysis was done to assess primary study overlap in the included systematic reviews. An evidence gap map (EGM) was developed by means of EPPI Reviewer Version 4.12.1.1.0.
Results
Search results and description of the included systematic reviews and meta-analyses
A comprehensive literature search was performed, and 583 publications were identified based on the selection criteria. Eight duplicate articles were removed, and the search was narrowed to 575 articles. The title and abstract search resulted in the exclusion of 515 articles (which were either systematic reviews on peri-implantitis or lasers other than those in the erbium family or study designs other than systematic reviews). Of the remaining 60 articles screened for full text, 43 were excluded as narrative reviews, and two systematic reviews were excluded since they did not assess outcomes chosen for this umbrella review. Of the 15 systematic reviews included in the qualitative synthesis, 10 had meta-analysis data (Figure 1). The excluded studies and the reasons for exclusion are listed in Supplementary Table 1.
Characteristics of included systematic reviews
The selected 15 systematic reviews included 50 randomized controlled trials (RCTs) with 1,681 participants. A qualitative synthesis was performed for all 15 included systematic reviews (Table 1), and a quantitative synthesis was performed using meta-analysis data from eight of the 15 systematic reviews. Only four of the 15 systematic reviews compared the efficacy of erbium lasers vs conventional therapy in NSPT [13, 15, 16, 18]. The remaining 11 systematic reviews compared the efficacy of lasers (including erbium lasers/diode laser/Nd:YAG laser/photodynamic therapy) vs conventional therapy in NSPT [8, 12, 14, 17, 19,20,21,22,23,24,25] The outcomes assessed in the included systematic reviews were probing pocket depth, clinical attachment level, reduction in microbial count, plaque index (PI), gingival index (GI), gingival recession (REC), bleeding on probing (BOP), visual analog scale (VAS) score, and patient comfort and adverse events following the use of erbium lasers/conventional therapy.
Most of the systematic reviews (12/15) evaluated PPD/CAL as the primary outcome, except the SR by Mikami et al. (2020) [24], wherein the authors evaluated VAS as the primary outcome variable and the studies by Akram et al. (2016) [20] and Kellesarian et al. (2017) [21], who evaluated the GCF levels of pro-inflammatory cytokines as the primary outcome variable. The secondary outcome measures evaluated in the included systematic reviews were bleeding on probing, plaque index, gingival index, gingival recession, and reduction of microbial levels.
Nine of the systematic reviews chose a minimum follow-up period of 3 months for inclusion of the RCTs [12,13,14,15, 18, 19, 22, 23, 25], whereas three of the systematic reviews included RCTs with a follow-up of at least 6 months [8, 16, 17]. The systematic review by Akram et al. (2016) [20] reported 8 weeks as the minimum follow-up time point for inclusion, and Kellesarian et al. (2017) [21] reported no specific time points for inclusion criteria; however, those authors included two RCTs evaluating erbium lasers with follow-up time points of 4 and 8 weeks. The systematic review by Mikami et al. (2020) [24] evaluated VAS as the primary outcome variable, and hence the follow-up time points ranged from immediately post-operative to 30 days.
VAS was assessed in the systematic review by Mikami et al. (2020) [24], who concluded that the use of erbium lasers (HLLT) could suppress post-operative pain. In a recent systematic review [18], the authors observed significantly lower VAS scores following the use of Er:Cr:YSGG laser as an adjunct or monotherapy for non-surgical treatment of periodontitis.
Systematic reviews by Akram et al. (2016) [20] and Kellesarian et al. (2017) [21] assessed the evidence on the influence of the use of lasers as an adjunct to SRP on the expression of inflammatory cytokines in GCF and concluded that the existing evidence was insufficient.
Subgroup analysis was done in three of the 15 selected systematic reviews [13, 14, 22]. The criteria used for subgroup analysis included (a) laser energy, (b) fluorescence feedback laser use, (c) quality of trial [13], (d) different modes of lasers [14], and (e) types of treatment and phases of therapy (non-surgical, maintenance, and surgical phase of treatment) [22] (Table 1).
Assessment of methodological quality of included systematic reviews
The methodological quality of the systematic reviews was assessed according to the ROBIS checklist. In this umbrella review, six systematic reviews were found to have low risk of bias, four had high risk of bias, and the remaining five had an unclear risk of bias (Table 2). The reporting quality was assessed by means of the PRISMA checklist. A score of 0 or 1 was allotted for each criterion of the PRISMA checklist based on whether the systematic review had fulfilled the criteria or not, respectively. The PRISMA scores are summarized [Supplementary Tables 2,3]. Most SRs with meta-analysis had scores between 22 and 27. The systematic review by Zhao et al. (2020) [25] fulfilled all the PRISMA requirements and received the maximum score of 27. Among the systematic reviews without meta-analysis data, the scores ranged between 15 and 22. The SR by Karlsson et al. (2008) [19] had missing data according to the PRISMA reporting checklist and received the lowest score (15/27) among all the included SRs.
Quantitative synthesis of meta-analysis data
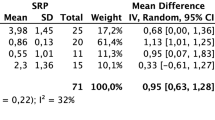
Of the 15 included systematic reviews, five had narrative syntheses [12, 17, 19,20,21], two had performed network meta-analyses [23, 25], and eight had performed meta-analyses [8, 13,14,15,16, 18, 22, 24]. The meta-analysis (MA) data from the included systematic reviews comparing the outcomes of CAL, PPD, REC, PI, and VAS in the experimental group (erbium laser) vs control (mechanical instrumentation for SRP) at various follow-up time points are summarized as forest plots in Figures 2 and 3. Considerable heterogeneity was observed for all the clinical and patient-related outcomes at the time points assessed (1, 3, 6, 12 months). Meta-analysis data for a few outcomes was available only for a few follow-ups time points, due to which a statistical analysis was not performed, and data were represented as available in the forest plot.
A forest plot representation of the meta- analysis data of the included systematic reviews comparing the outcome of clinical attachment level (CAL) [2.1 to 2.4] and probing pocket depth (PPD) [2.5 to 2.8] in experimental (erbium laser) versus control (mechanical instrumentation for SRP) at various time points.
A forest plot representation of the meta- analysis data of the included systematic reviews comparing the outcome of gingival recession change (REC) [3.1 to 3.3], plaque index (PI) [3.4], and visual analog scale score (VAS) [3.5] in experimental (erbium laser) versus control (mechanical instrumentation for SRP) at various time points.
Corrected covered areas
A calculation of corrected covered areas (CCA) was performed to assess the influence of the overlapping primary studies in multiple systematic reviews according to a protocol described by Seifo et al. (2019) [26]. CCA = N-r/rc-r, wherein N = number of included publications including those counted twice, r = number of rows (number of indexed publications — RCTs), and c = number of columns (number of included systematic reviews). A CCA value of 0.08 was obtained, indicating moderate overlap of the RCTs in the included systematic reviews (Figure 4).
Evidence gap map development and description
To understand the heterogeneity in the outcome data in quantitative synthesis, we generated an evidence gap map (using EPPI Reviewer Version 4.12.1.1.0) based on interventions and outcomes in the included RCTs and systematic reviews (https://eppi.ioe.ac.uk/cms/Portals/35/Maps/SriRamachandra/EGM_RCT_SR-ErbiumLasers-NSP-RoB.html) (https://eppi.ioe.ac.uk/cms/Portals/35/Maps/SriRamachandra/EGM_RCT_SR-ErbiumLasers-NSP.html).
In total, 65 studies (50 randomized controlled trials and 15 systematic reviews) were included in this EGM. The impact evaluation studies were represented by the 50 randomized controlled trials, whose numbers steadily increased from 2001 to 2019 [9,10,11, 27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73]. The quality assessment for the included RCTs was as reported by the authors of SRs (using the Cochrane risk-of-bias tool). The quality assessment of the included systematic reviews was performed by the authors of this umbrella review using the Risk of Bias in Systematic Reviews (ROBIS) scale. Outcome measures for both the EGMs included clinical outcomes (CAL, PPD, REC. PI, GI, BOP), microbial level reduction, patient-reported outcome measures (VAS), and adverse outcomes reporting.
Among the 50 RCTs included in the EGM, most of the trials had evaluated the efficacy of erbium lasers as a monotherapy (20/50 RCTs — 40%) or as an adjunct to SRP (23/50 RCTs — 46%) in NSPT. Seven studies accounted for the remaining 14%, distributed among the three remaining interventions. The trial quality of the primary studies was also included in the EGM based on the risk of bias as reported by the authors of the systematic reviews. Of the 50 RCTs, the methodological quality of 42 RCTs as reported in the SRs was included in the EGM. The remaining eight RCTs were from the systematic review by Li et al. (2021), wherein the authors discussed the domain-based assessment of the included RCTs and not the individual study quality. The authors of this systematic review were contacted; however, data for the individual study methodological quality could not be obtained. Among the 42 studies with quality assessment data available, 11 had a low risk of bias, 17 studies had high risk of bias, and 14 studies had an unclear risk of bias. Among the primary studies, only 7/50 studies reported the VAS scores, and 2/50 studies reported adverse outcomes following the use of erbium lasers or mechanical instrumentation for SRP. The clinical outcomes commonly reported were CAL, PPD, PI, GI, and REC, and the most frequently reported time points were 3 and 6 months.
Among the included systematic reviews, CAL and PPD were the most frequently included and reported clinical parameters in the meta-analysis; however, in a systematic review by Mikami et al. (2020) [24], VAS was reported as the primary outcome measure. Risk-of-bias data can be found in Table 2 and were included in the EGM developed. Some SRs had performed meta-analysis at 3 months [22], some at the 6-month time point [8], and some SRs provided meta-analysis data for 3, 6, and 12 months [13,14,15,16, 18].
Discussion
This overview of systematic reviews was performed to provide an insight into the efficacy of erbium lasers in NSPT. The published literature includes several systematic reviews that addressed this question, with various results being reported [12, 15, 16]. This overview observed heterogeneity in the outcomes assessed in the included systematic reviews. Hence, an evidence gap map was developed for the identification of any gaps in the study data pertaining to the research question. The following gaps were identified: lack of clinical outcome data at longer follow-up time points (> 6 months), variations in quality assessment for the RCTs included in and assessed by authors of different systematic reviews, need for RCTs with higher methodological quality (since several of the included studies were reported to have a high risk of bias), and very few studies (RCTs/SRs) that assessed patient-reported outcome measures and adverse outcomes.
It can be inferred from the qualitative synthesis of the included systematic reviews that erbium lasers, when used as an adjunct to SRP, were better than SRP alone. This can be substantiated by the observations of a significant short-term reduction in CAL and PPD and BOP (1–3 months), [14, 15, 18, 23, 25] but results comparable with those of SRP were obtained at ≥ 6-month follow-up time points [8, 12,13,14,15,16,17,18,19, 22].
A quantitative synthesis of the outcome data pooled from the systematic reviews with meta-analysis data available demonstrated considerable variation in outcomes at the time points assessed. The outcomes of CAL and PPD were assessed at 3 and 6 months in most SRs. An improved CAL gain and reduction of PPD were reported at 1 and 3 months, but no additional benefit was observed at longer-term follow-up ≥ 6 months in the erbium laser group as compared with SRP [8, 16]. For outcomes such as VAS score [15, 18, 24], gingival recession, and plaque index [13, 16], only a few systematic reviews had performed a meta-analysis of the data, and hence a clear inference could not be made.
The inclusion of the same primary studies in two or more systematic reviews caused overlap and may have contributed to bias. The degree of overlap can be graphically represented efficiently and pragmatically by the corrected covered areas (CCA) formula. The distribution of the 50 RCTs in the 15 SRs was plotted, and moderate overlap (CCA value — 0.08) was identified.
The EGM provides an abundant source of information on included SRs related to the efficacy of erbium lasers in NSPT. The number of studies, outcomes assessed, interventions performed, and quality of primary studies and systematic reviews are represented visually, allowing for a quick interpretation of the data. The map also has a provision for updating the data as new studies are performed and published, which is convenient for researchers working in the particular field.
This umbrella review has attempted to collate the information from existing SRs on the efficacy of erbium lasers in NSPT. The pooled meta-analyses reveal marginal short-term benefits (3 and 6 months) and no differences in outcomes when compared with SRP at longer-term follow-ups (12 and 24 months). This could be due to a lack of data at long-term follow-up time points (12 and 24 months) in the primary study data, as revealed in the EGM. The umbrella review has also brought to light several inconsistencies in the assessment of trial quality (Supplementary Fig. 2). A confounding variable identified during the qualitative synthesis was the lack of standardization of laser operating parameters by the RCTs, as reported in several of the included systematic reviews [16, 17, 24]. In addition, the EGM has demonstrated that only around 30% of the studies were of high quality (low risk of bias), and the remaining had either high or unclear risk of bias, emphasizing the need for more RCTs with higher quality. It can be inferred from the EGM that there is a lack of information on patient-reported outcome measures and adverse event reporting.
The limitations of this overview were that the trial quality data could not be obtained from the authors of one systematic review [18] and a deviation from the published protocol to include an EGM analysis. However, this overview has reported on the gap in evidence which needs to be corrected for clinical practice guidelines to be developed for erbium laser use in NSPT.
Conclusion
1. The use of erbium lasers as monotherapy or adjunct to scaling and root planing improves clinical and patient reported outcome measures at earlier time points of follow-up.
2. There is a need for multi-center trials with standardized laser parameters, uniformity in outcome assessment and long-term follow-up for demonstration of the efficacy of erbium lasers in nonsurgical periodontal therapy.
References
Tatakis DN, Kumar PS (2005) Etiology and pathogenesis of periodontal diseases. Dent Clin N Am 49(3):491–516. https://doi.org/10.1016/j.cden.2005.03.001
Sanz M (2010) European workshop in periodontal health and cardiovascular disease. Oxford University Press, Oxford
GBD (2017) Disease and Injury Incidence and Prevalence Collaborators (2017) Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 390(10100):1211–1259. https://doi.org/10.1016/S0140-6736(17)32154-2
Caton JG, Armitage G, Berglundh T, Chapple ILC, Jepsen S, Kornman KS et al (2018) A new classification scheme for periodontal and peri-implant diseases and conditions - introduction and key changes from the 1999 classification. J Periodontol 89(Suppl 1):S1–S8. https://doi.org/10.1002/JPER.18-0157
Sanz M, Teughels W (2008) Innovations in non-surgical periodontal therapy: consensus report of the sixth European workshop on periodontology. J Clin Periodontol 35(8 Suppl):3–7. https://doi.org/10.1111/j.1600-051X.2008.01256.x
Schwarz F, Pütz N, Georg T, Reich E (2001) Effect of an Er:YAG laser on periodontally involved root surfaces: an in vivo and in vitro SEM comparison. Lasers Surg Med 29(4):328–335. https://doi.org/10.1002/lsm.1125
Smiley CJ, Tracy SL, Abt E et al (2015) Evidence-based clinical practice guideline on the nonsurgical treatment of chronic periodontitis by means of scaling and root planing with or without adjuncts. J Am Dent Assoc 146(7):525–535. https://doi.org/10.1016/j.adaj.2015.01.026
Smiley CJ, Tracy SL, Abt E et al (2015) Systematic review and meta-analysis on the nonsurgical treatment of chronic periodontitis by means of scaling and root planing with or without adjuncts. J Am Dent Assoc 146(7):508–524. https://doi.org/10.1016/j.adaj.2015.01.028
Sculean A, Schwarz F, Berakdar M, Romanos GE, Arweiler NB, Becker J (2004) Periodontal treatment with an Er: YAG laser compared to ultrasonicInstrumentation: a pilot study. J Periodontol 75(7):966–973. https://doi.org/10.1902/jop.2004.75.7.966
Ciurescu CE, Cosgarea R, Ciurescu D et al (2019) Adjunctive use of InGaAsP and Er, Cr: YSGG lasers in nonsurgical periodontal therapy: a randomized controlled clinical study. Quintessence Int (Berl) 50(6):436–447. https://doi.org/10.3290/j.qi.a42508
Soo L, Leichter JW, Windle J et al (2012) A comparison of Er: YAG laser and mechanical debridement for the non-surgical treatment of chronic periodontitis: a randomized, prospective clinical study. J Clin Periodontol 39(6):537–545. https://doi.org/10.1111/j.1600-051X.2012.01873.x
Schwarz F, Aoki A, Becker J, Sculean A (2008) Laser application in non-surgical periodontal therapy: a systematic review. J Clin Periodontol 35:29–44. https://doi.org/10.1111/j.1600-051X.2008.01259.x
Zhao Y, Yin Y, Tao L, Nie P, Tang Y, Zhu M (2014) Er: YAG laser versus scaling and root planing as alternative or adjuvant for chronic periodontitis treatment: a systematic review. J Clin Periodontol 41(11):1069–1079. https://doi.org/10.1111/jcpe.12304
Cheng Y, Chen JW, Ge MK, Zhou ZY, Yin X, Zou SJ (2016) Efficacy of adjunctive laser in non-surgical periodontal treatment: a systematic review and meta-analysis. Lasers Med Sci 31(1):151–163. https://doi.org/10.1007/s10103-015-1795-5
Ma L, Zhang X, Ma Z et al (2018) Clinical effectiveness of Er: YAG lasers adjunct to scaling and root planing in non-surgical treatment of chronic periodontitis: a meta-analysis of randomized controlled trials. Med Sci Monit Int Med J Exp Clin Res 24:7090–7099. https://doi.org/10.12659/MSM.911863
Sgolastra F, Petrucci A, Gatto R, Monaco A (2012) Efficacy of Er: YAG laser in the treatment of chronic periodontitis: systematic review and meta-analysis. Lasers Med Sci 27(3):661–673. https://doi.org/10.1007/s10103-011-0928-8
Coluzzi D, Anagnostaki E, Mylona V, Parker S, Lynch E (2020) Do lasers have an adjunctive role in initial non-surgical periodontal therapy? A systematic review. Dent J 8(3):93. https://doi.org/10.3390/dj8030093
Li M-M, Jia J-H, Wu M-X et al (2021) Clinical effectiveness of Er,Cr:YSGG lasers in non-surgical treatment of chronic periodontitis: a meta-analysis of randomized controlled trials. Lasers Med Sci 36(4):889–901. https://doi.org/10.1007/s10103-020-03156-2
Karlsson MR, Diogo Löfgren CI, Jansson HM (2008) The effect of laser therapy as an adjunct to non-surgical periodontal treatment in subjects with chronic periodontitis: a systematic review. J Periodontol 79(11):2021–2028. https://doi.org/10.1902/jop.2008.080197
Akram Z, Abduljabbar T, Sauro S, Daood U (2016) Effect of photodynamic therapy and laser alone as adjunct to scaling and root planing on gingival crevicular fluid inflammatory proteins in periodontal disease: a systematic review. Photodiagn Photodyn Ther 16:142–153. https://doi.org/10.1016/j.pdpdt.2016.09.004
Kellesarian SV, Malignaggi VR, Majoka HA et al (2017) Effect of laser-assisted scaling and root planing on the expression of pro-inflammatory cytokines in the gingival crevicular fluid of patients with chronic periodontitis: a systematic review. Photodiagn Photodyn Ther 18:63–77. https://doi.org/10.1016/j.pdpdt.2017.02.010
Chambrone L, Ramos UD, Reynolds MA (2018) Infrared lasers for the treatment of moderate to severe periodontitis: an American Academy of Periodontology best evidence review. J Periodontol 89(7):743–765. https://doi.org/10.1902/jop.2017.160504
Jia L, Jia J, Xie M et al (2020) Clinical attachment level gain of lasers in scaling and root planing of chronic periodontitis: a network meta-analysis of randomized controlled clinical trials. Lasers Med Sci 35(2):473–485. https://doi.org/10.1007/s10103-019-02875-5
Mikami R, Mizutani K, Sasaki Y, Iwata T, Aoki A (2020) Patient-reported outcomes of laser-assisted pain control following non-surgical and surgical periodontal therapy: a systematic review and meta-analysis. PLoS One 15(9):e0238659. https://doi.org/10.1371/journal.pone.0238659
Zhao P, Song X, Nie L et al (2020) Efficacy of adjunctive photodynamic therapy and lasers in the non-surgical periodontal treatment: a Bayesian network meta-analysis. Photodiagn Photodyn Ther 32:101969. https://doi.org/10.1016/j.pdpdt.2020.101969
Seifo N, Cassie H, Radford JR, Innes NPT (2019) Silver diamine fluoride for managing carious lesions: an umbrella review. BMC Oral Health 19(1):145. https://doi.org/10.1186/s12903-019-0830-5
Schwarz F, Sculean A, Georg T, Reich E (2001) Periodontal treatment with an Er: YAG laser compared to scaling and root planing. A controlled clinical study. J Periodontol 72(3):361–367. https://doi.org/10.1902/jop.2001.72.3.361
Schwarz F, Sculean A, Berakdar M, Georg T, Reich E, Becker J (2003) Clinical evaluation of an Er: YAG laser combined with scaling and root planing for non-surgical periodontal treatment: a controlled, prospective clinical study. J Clin Periodontol 30(1):26–34. https://doi.org/10.1034/j.1600-051x.2003.300105.x
Schwarz F, Sculean A, Berakdar M, Georg T, Reich E, Becker J (2003) Periodontal treatment with an Er: YAG laser or scaling and root planing. A 2-year follow-up split-mouth study. J Periodontol 74(5):590–596. https://doi.org/10.1902/jop.2003.74.5.590
Tomasi C, Schander K, Dahlén G, Wennström JL (2006) Short-term clinical and microbiologic effects of pocket debridement with an Er: YAG laser during periodontal maintenance. J Periodontol 77(1):111–118. https://doi.org/10.1902/jop.2006.77.1.111
Crespi R, Cappare P, Toscanelli I, Gherlone E, Romanos GE (2007) Effects of Er: YAG laser compared to ultrasonic scaler in periodontal treatment: a 2-year follow-up split-mouth clinical study. J Periodontol 78(7):1195–1200. https://doi.org/10.1902/jop.2007.060460
Derdilopoulou FV, Nonhoff J, Neumann K, Kielbassa AM (2007) Microbiological findings after periodontal therapy using curettes, Er: YAG laser, sonic, and ultrasonic scalers. J Clin Periodontol 34(7):588–598. https://doi.org/10.1111/j.1600-051X.2007.01093.x
Kelbauskiene S, Maciulskiene V (2007) A pilot study of Er, Cr: YSGG laser therapy used as an adjunct to scaling and root planing in patients with early and moderate periodontitis. Stomatologija 9(1):21–26
Lopes BMV, Marcantonio RAC, Thompson GMA, Neves LHM, Theodoro LH (2008) Short-term clinical and immunologic effects of scaling and root planing with Er: YAG laser in chronic periodontitis. J Periodontol 79(7):1158–1167. https://doi.org/10.1902/jop.2008.070600
Rotundo R, Nieri M, Cairo F et al (2010) Lack of adjunctive benefit of Er: YAG laser in non-surgical periodontal treatment: a randomized split-mouth clinical trial. J Clin Periodontol 37(6):526–533. https://doi.org/10.1111/j.1600-051X.2010.01560.x
Lopes BMV, Theodoro LH, Melo RF, de Thompson GMA, Marcantonio RAC (2010) Clinical and microbiologic follow-up evaluations after non-surgical periodontal treatment with erbium: YAG laser and scaling and root planing. J Periodontol 81(5):682–691. https://doi.org/10.1902/jop.2010.090300
Braun A, Jepsen S, Deimling D, Ratka-Krüger P (2010) Subjective intensity of pain during supportive periodontal treatment using a sonic scaler or an Er: YAG laser. J Clin Periodontol 37(4):340–345. https://doi.org/10.1111/j.1600-051X.2010.01536.x
Domínguez A, Gómez C, García-Kass AI, García-Nuñez JA (2010) IL-1β, TNF-α, total antioxidative status and microbiological findings in chronic periodontitis treated with fluorescence-controlled Er: YAG laser radiation. Lasers Surg Med Off J Am Soc Laser Med Surg 42(1):24–31. https://doi.org/10.1002/lsm.20873
Feng XH, Lu RF, He L (2011) A short-term clinical evaluation of periodontal treatment with an Er: YAG laser for patients with chronic periodontitis: a split-mouth controlled study. J Peking Univ Heal Sci 43(6):886–890
Kelbauskiene S, Baseviciene N, Goharkhay K, Moritz A, Machiulskiene V (2011) One-year clinical results of Er, Cr: YSGG laser application in addition to scaling and root planing in patients with early to moderate periodontitis. Lasers Med Sci 26(4):445–452. https://doi.org/10.1007/s10103-010-0799-4
Yilmaz S, Kut B, Gursoy H, Eren Kuru B, Noyan U, Kadir T (2012) Er: YAG laser versus systemic metronidazole as an adjunct to nonsurgical periodontal therapy: a clinical and microbiological study. Photomed Laser Surg 30(6):325–330. https://doi.org/10.1089/pho.2010.2762
Malali E, Kadir T, Noyan U (2012) Er: YAG lasers versus ultrasonic and hand instruments in periodontal therapy: clinical parameters, intracrevicular micro-organism and leukocyte counts. Photomed Laser Surg 30(9):543–550. https://doi.org/10.1089/pho.2011.3202
Krohn-Dale I, Bøe OE, Enersen M, Leknes KN (2012) Er: YAG laser in the treatment of periodontal sites with recurring chronic inflammation: a 12-month randomized, controlled clinical trial. J Clin Periodontol 39(8):745–752. https://doi.org/10.1111/j.1600-051X.2012.01912.x
Ratka-Krüger P, Mahl D, Deimling D et al (2012) Er: YAG laser treatment in supportive periodontal therapy. J Clin Periodontol 39(5):483–489. https://doi.org/10.1111/j.1600-051X.2012.01857.x
Yılmaz S, Algan S, Gursoy H, Noyan U, Kuru BE, Kadir T (2013) Evaluation of the clinical and antimicrobial effects of the Er: YAG laser or topical gaseous ozone as adjuncts to initial periodontal therapy. Photomed Laser Surg 31(6):293–298. https://doi.org/10.1089/pho.2012.3379
Ge LH, Shu R (2014) Clinical application of initial treatment with Er:Cr:YSGG laser for patients with chronic periodontitis. J Oral Sci Res 03:235–237
Ming C (2015) The clinical effect of erbium laser ssisted treatment of chronic periodontitis. Mod Med J China 11:59–61
Gutknecht N, Van Betteray C, Ozturan S, Vanweersch L, Franzen R (2015) Laser supported reduction of specific microorganisms in the periodontal pocket with the aid of an Er, Cr: YSGG laser: a pilot study. Sci World J 2015:450258. https://doi.org/10.1155/2015/450258
Ji ZZ, Xu XM, Zhang RZ, Wang C, Xia R, Sang Y (2015) Clinical evaluation of Er:Cr:YSGG laser for the treatment of chronic periodontitis. Acta Univ Med Anhui 5:669–672
Sanz-Sánchez I, Ortiz-Vigón A, Matos R, Herrera D, Sanz M (2015) Clinical efficacy of subgingival debridement with adjunctive erbium: yttrium-aluminum-garnet laser treatment in patients with chronic periodontitis: a randomized clinical trial. J Periodontol 86(4):527–535. https://doi.org/10.1902/jop.2014.140258
Sanz-Sánchez I, Ortiz-Vigón A, Herrera D, Sanz M (2016) Microbiological effects and recolonization patterns after adjunctive subgingival debridement with Er: YAG laser. Clin Oral Investig 20(6):1253–1261. https://doi.org/10.1007/s00784-015-1617-y
Chen MH, Wang LM (2016) Effect of Er:Cr:YSGG laser on the treatment of chronic periodontitis:a short term evaluation. Stomatology 36(1):64–67
Qn CN, Kang J, Zhang YL, Luan QX (2016) Application of Er:Cr:YSGG laser in non-surgical treatment of chronic periodontitis. Beijing J Stomatol 24(1):21–24
Zhou LF, Fan X (2016) A short term clinical effect observation of Er:YAG laser assisted treatment of chronic periodontitis. J Prev Treat Stomatol Dis 3:170–173
Cao WJ, Gao ZB, Wang YM, Zhang WJ, Tian Y (2016) Comparison of efficacy of waterlaser and ultrasonic scaling in treatment of moderate chronic periodontitis. Prog Mod Biomed 16(23):4539–4541
Ruiz Magaz V (2016) Efficacy of adjunctive Er, Cr: YSGG laser application following scaling and root planing in periodontally diseased patients. Int J Perio Rest Dent 36(5):715–721. https://doi.org/10.11607/prd.2660
Dereci Ö, Hatipoğlu M, Sindel A, Tozoğlu S, Üstün K (2016) The efficacy of Er, Cr: YSGG laser supported periodontal therapy on the reduction of peridodontal disease related oral malodor: a randomized clinical study. Head Face Med 12(1):1–7. https://doi.org/10.1186/s13005-016-0116-y
Cui JY, Dong FS, Li SJ, Li CN, Wu MX (2017) The curative effects of twinlight laser treatment on chronic periodontitis. J Pr Stomatol 33(6):807–811
Chen M (2017) Clinical efficacy of Er:YAG laser as adjunctive therapy of chronic periodontitis. MMJC. 17(11):59–61
Ge LH, Zhang YX, Shu R (2017) Er,Cr:YSGG laser application for the treatment of periodontal furcation involvement. Photomed Laser Surg 35(2):92–97. https://doi.org/10.1089/pho.2016.4145
Wu K-Y, Xu C-J, Chi Y-T, Sun X-J, Wang H-F (2017) Detection of Dickkopf-1 and alkaline phosphatase activity in gingival crevicular fluid from chronic periodontitis with Er: YAG laser as an adjunctive treatment. Shanghai J Stomatol 26(3):285–289
Wang Y, Li W, Shi L, Zhang F, Zheng S (2017) Comparison of clinical parameters, microbiological effects and calprotectin counts in gingival crevicular fluid between Er: YAG laser and conventional periodontal therapies: a split-mouth, single-blinded, randomized controlled trial. Medicine (Baltimore) 96(51):pe9367. https://doi.org/10.1097/MD.0000000000009367
Wang YS, Li JT (2017) Effect analysis of different treatment methods in the treatment of periodontitis. Clin Res Tract 2(4):22–23
Weiyan L, Yuyue H, Zhijuan Z (2017) Study on the clinical effect of Er:YAG laser assisted ultrasound therapy instrument in periodontitis patients. Nurs Pract Res 11:10–12
Shuxia S, Shaojun Z, Na L, Peizhen S (2017) Short term clinical effect of Er:YAG laser for chronic periodontitis. Shandong Med J 10:98–99
Ye ZF, Du Y, Zhu XQ (2018) Study on the clinical effect of Er,Cr:YSGG laser combined with oral basic therapy in the treatment of patients with periodontitis. China High Med Educ 2:142–145
Grzech-Leśniak K, Sculean A, Gašpirc B (2018) Laser reduction of specific microorganisms in the periodontal pocket using Er: YAG and Nd: YAG lasers: a randomized controlled clinical study. Lasers Med Sci 33(7):1461–1470. https://doi.org/10.1007/s10103-018-2491-z
Üstün K, Hatipoğlu M, Daltaban Ö, Felek R, Firat MZ (2018) Clinical and biochemical effects of erbium, chromium: yttrium, scandium, gallium, garnet laser treatment as a complement to periodontal treatment. Niger J Clin Pract 21(9):1150–1157. https://doi.org/10.4103/njcp.njcp_51_18
Cao Y, Wu WL, Xue YQ, Sun WB (2018) Efficacy observation of Nd:YAG and Er:YAG laser for the treatment of severe periodontitis. Stomatology 38(6):514–517
Zhao M, Yang CY, Guo XQ, Wang L, Wang JJ, Zhang Y (2018) Clinical evaluation of laser treatment for moderate and severe chronic periodontitis. Med Inf 31(5):93–95
Zhou X, Lin M, Zhang D, Song Y, Wang Z (2019) Efficacy of Er: YAG laser on periodontitis as an adjunctive non-surgical treatment: a split-mouth randomized controlled study. J Clin Periodontol 46(5):539–547. https://doi.org/10.1111/jcpe.13107
Zengin Celik T, Saglam E, Ercan C, Akbas F, Nazaroglu K, Tunali M (2019) Clinical and microbiological effects of the use of erbium: yttrium–aluminum–garnet laser on chronic periodontitis in addition to nonsurgical periodontal treatment: a randomized clinical trial—6 months follow-up. Photobiomodul Photomed Laser Surg 37(3):182–190. https://doi.org/10.1089/photob.2018.4510
Wang YP, Lin ZK, Shu R (2019) Short term clinical efficacy observation of adjunctive Er,Cr:YSGG laser application following subgingival scaling in patients with severe periodontitis. Shangai Jiaotong Univ Med Sci 39(4):378–382
Funding
The study was self-funded.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
Not applicable as it is an umbrella review
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
About this article
Cite this article
Lavu, V., Kumar, D., Krishnakumar, D. et al. Erbium lasers in non-surgical periodontal therapy: an umbrella review and evidence gap map analysis. Lasers Med Sci 37, 103–120 (2022). https://doi.org/10.1007/s10103-022-03504-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-022-03504-4