Abstract
The aim of this work was to perform an integrative literature review on the influence of laser irradiation on zirconia implants to enhance surface topographic aspects and the biological response for osseointegration. An electronic search was carried out on the PubMed database using the following search terms: “zirconia” AND “laser” AND “surface modification” OR “surface treatment” AND “dental implants” OR “bone” OR “osteoblast” OR “osseointegration.” Of the identified articles, 12 studies were selected in this review. Results reported that the laser irradiation was capable of promoting changes on the zirconia surfaces regarding topographic aspects, roughness, and wettability. An increase in roughness was recorded at micro- and nano-scale and it resulted in an enhanced wettability and biological response. Also, adhesion, spreading, proliferation, and differentiation of osteogenic cells were also enhanced after laser irradiation mainly by using a femtosecond laser at 10nJ and 80 MHz. After 3 months of osseointegration, in vivo studies in dogs revealed a similar average percentage of bone-to-implant contact (BIC) on zirconia surfaces (around 47.9 ± 16%) when compared to standard titanium surfaces (61.73 ±16.27%), denoting that there is no significant difference between such different materials. The laser approach revealed several parameters that can be used for zirconia surface modification such as irradiation intensity, time, and frequency. Laser irradiation parameters can be optimized and well-controlled to reach desirable surface morphologic aspects and biological response concerning the osseointegration process.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In implant dentistry, osseointegration has been studied considering the direct, structural, and functional connection between bone tissue and implant surfaces over occlusal loading [1,2,3,4]. The long-term stability of dental implants depends on the chemical composition and surface of implants materials; although, the health state of patients also affect osseointegration [5, 6]. On standard titanium dental implants, several physicochemical techniques have been successfully used for enhanced osseointegration such as double acidic etching and grit-blasting [3, 6]. However, the surface modification of zirconia surfaces revealed different outcomes taking into consideration ordinary physicochemical techniques [7,8,9,10,11]. At first, the surface topographic aspects are quite different when compared to those noticed on titanium surfaces [8, 11, 12]. Second, the ordinary acidic etching has no effect on zirconia surfaces regarding roughness changes [11]. In this way, advanced surface modification methods have been developed to modify zirconia surfaces and maintaining the physical performance of the material [12,14,15,16,17,17].
Zirconia is a chemically stable and biocompatible ceramic material that has been used for implants and prosthetics in orthopedics and dentistry [5, 18,19,20]. The chemical stability of zirconia becomes a challenge concerning the surface modification [11, 19]. The physical properties of zirconia are achieved by stabilizing the tetragonal zirconia phase at room temperature by incorporating small contents of different oxides, namely Y2O3, MgO, CeO2, or CaO [21, 18]. For instance, yttria-stabilized tetragonal zirconia polycrystals (Y-TZP) has a flexural strength at 900–1200 MPa, elastic modulus of approximately 210 GPa, and fracture toughness at around 7–10 MPa.m1/2 [20, 18]. In vitro and in vivo studies have reported the osseointegration capability of Y-TZP zirconia implants quite similar to those on titanium implants since the surface modification techniques are well applied [7,8,9,10,11]. Grit-blasting has been commonly used to increase the titanium or zirconia roughness for adsorption of proteins, attachment of osteogenic cells, and bone formation [5, 8, 9, 22, 23]. Micro- and nano-scale surface modification influences the adsorption of extracellular matrix proteins, which regulate the adhesion of osteoblasts to the implant surface leading to cell proliferation and differentiation [5, 8, 24, 23]. However, the morphological aspects of zirconia surfaces cannot be controlled by using only ordinary surface modification such as grit-blasting since that provides a random texture on the surface.
Various methods of surface treatment have been proposed to improve the surface properties of zirconia implants [11, 22, 25,24,27]. Currently, surface modification on the implant surface via laser irradiation has gathering attention regarding the increase in roughness, wettability, and biological response without affecting the physical properties of zirconia [12, 14,16,16, 28, 23]. Morphological features (e.g., micro-grooves, pits, valleys, and peaks) on material surfaces can be controlled by using different intensity, type, time, and frequency of laser irradiation [12, 14, 28, 29].
Lasers can operate in either continuous mode (continuous wave—CW) or pulsed mode (PM), although the latter deliver the energy to the material in short (mili- to nano-seconds) or ultra-short (pico- to femto-seconds) periods of time (pulses). Various laser sources, working at different wavelengths and pulse duration have been studied aiming to modifying the surface of zirconia-based ceramics: Nd:YAG [30], Er:YAG [31], CO2 [32], Er, Cr:YSGG [33], and Nd:YVO4 [34]. Considering zirconia is a brittle material it is highly sensitive to surface processing defects like pores and cracks, as the one produced for CW CO2 lasers or Nd:YAG lasers working short pulses (nanosecond regime) [35]. The presence of cracking is attributed to the (extensive) heat-affected zone generated by the thermal induced mechanisms developed by lasers working at the nanosecond regime and proved to be detrimental to the mechanical performance of zirconia [30, 35]. Alternatively, ultra-short pulsed lasers (pico- and femtosecond lasers) have been referred to produce ceramic-structured ceramic surfaces with minimal or no damages on the adjacent surfaces to the laser-machined ones [12, 13, 28]. The localized energy in very thin surface layers (< 100 nm) during very short times (10−15–10−12 s) can lead to surface ablation of material with negligible heat effects on the surrounding material, and thus avoiding surface defects that are detrimental to the mechanical behavior of brittle materials.
The main aim of this study was to perform a literature review on the effects of laser irradiation of zirconia implants on their surface morphological aspects and biological response. It was hypothesized that laser irradiation is able to improve the surface morphologic features of zirconia implants leading to a enhanced biological response and osseointegration.
Method
Information sources and search strategy
An electronic search was performed on the PubMed database using the following search items: “zirconia” AND “laser” AND “surface modification” OR “surface treatment” AND “dental implants” OR “bone” OR “osteoblast” OR “osseointegration.” The inclusion criteria involved articles published in English language up to January 10, 2021 reporting studies on the modification of zirconia surfaces by laser irradiation. The eligibility inclusion criteria used for article searches also involved articles written in English, meta-analyses, randomized controlled trials, and prospective cohort studies. The exclusion criteria were the following: papers without abstract; case report with short follow-up period; studies focusing only on other surface modification methods. Also, a hand-search was performed on the reference lists of all primary sources and eligible studies of this systematic review for additional relevant publications. Studies based on publication date were not restricted during the search process. The present method was performed following the search strategy applied in previous integrative reviews 36,51,52,53,54,41.
Study selection and data collection process
The articles retrieved from the search process were evaluated in three steps. The total of articles was compiled for each combination of key terms and therefore the duplicates were removed using Mendeley citation manager (Elsevier BV). Studies were primarily scanned for relevance by title, and the abstracts of those that were not excluded at this stage were assessed. The second step comprised the evaluation of the abstracts and non-excluded articles, according to the eligibility criteria on the abstract evaluation. Three of the authors (JCMS, BH, WFC) independently evaluated the titles and abstracts of potentially relevant articles.
A preliminary evaluation of the abstracts was carried out to establish whether the articles met the main aim of the study. Selected articles were individually read and evaluated concerning the purpose of this study. At last, the eligible articles received a study nomenclature label, combining first author names and year of publication. Two reviewers independently organised the data, such as author names, journal, publication year, purpose, zirconia types, roughness, biological response, bone-to-implant contact (BIC) percentage, and laser parameters such as intensity, exposure time, laser type, wavelength, and application mode. Data of the reports were harvested directly into a specific data collection form to avoid multiple data recording regarding multiple reports within the same study (e.g., reports with different set-ups). Such evaluation was individually carried out by two researchers, followed by a joint discussion to ultimately select the relevant studies.
Results
The bibliographic search on PubMed identified a total of 101 articles, as shown in Fig. 1. After excluding duplicates, 46 articles were evaluated by title and abstract although 31 were excluded because they did not meet the inclusion criteria. The remnant 15 articles were full read; although, 12 studies were considered relevant to the purpose of the present study taking into account a complete information on laser parameters, methods, and main outcomes.
Of the 12 selected articles, 7 studies were carried out in vitro while 5 studies were performed in vivo. The BIC percentage was evaluated by 4 studies while 3 studies evaluated the resorption of the bone crest. Laser surface treatment was morphologically characterized by in vitro articles although 4 studies evaluated the cellular response to the laser surface treatment. The main outcomes can be drawn as follow:
-
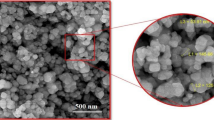
The laser treatment of the surface promoted changes in the topography of the implant surface at the following levels of scale: mesoscale (e.g., grooves), micro-scale (e.g., peak/valley), nanoscale (e.g., nodules) [42]. The crystalline structure of the zirconia can be maintained after laser treatment leading to the maintenance of the tetragonal phase [12, 14]. A nano-scale rough surface was noted in the micro-grooves of zirconia surfaces [14, 43,35,45].
-
Different surface topographic aspects were associated with the different types of lasers used for surface modification: CW lasers (e.g., CO2) produced different levels of stochastic roughness while short or ultra-short pulsed lasers (e.g., nano, pico, or femtosecond lasers) were able to imprint different patterns to the surface.
-
The laser surface treatment enhanced the adhesion, proliferation, and differentiation of osteoblasts on the zirconia surfaces, within 1 to 8 times of cell proliferation within the laser-treated groups compared to control groups [15, 16].
-
In animal models, BIC percentage on laser-treated zirconia implants showed high mean values as found for zirconia surfaces with enhanced osseointegration [13, 46, 47]. When compared to the laser treatment produced on the surface of zirconia implants over grit-blasted and etched surfaces, the further laser treatment provided a higher degree of BIC [43]. However, laser-treated zirconia showed similar BIC values to the titanium surfaces treated by ordinary grit-blasting and etching procedures [13].
-
Also, the laser-treated implants showed adequate levels of peri-implant bone crest maintenance (~ 0.5 ±0.23 mm) in the animal models over a period of 90 days.
Discussion
Zirconia implants
Zirconia has revealed remarkable clinical outcomes in the biomedical field, mainly in orthopedics and dentistry, due to the biological and mechanical response [6, 9, 21, 18, 19]. In the last years, zirconia has been used to develop teeth root canal posts, orthodontic brackets, implant abutments, and prosthetic infrastructures [48, 49, 19]. In the last 15 years, zirconia implants has increasingly become commercially available providing adequate esthetic, mechanical, and biological peri-implant outcomes [8, 20, 19, 23].
Zirconium dioxide (ZrO2) known as zirconia is a polymorphic ceramic, which has three distinct crystallographic phases: monoclinic (m), tetragonal (t), and cubic (c) [50] At room temperature, pure ZrO2 has a monoclinic structure that remains stable up to 1170 °C [21]. It turns to the tetragonal zirconia when sintered at temperature between 1170 and 2370 °C while the cubic phase is reached between 2370 and 2680 °C [21, 18]. On cooling, the ZrO2 tetragonal phase becomes monoclinic at a temperature around 970 °C [21]. The transformation pathway of tetragonal to the monoclinic phase is associated with approximately 3 to 4% volumetric expansion that can lead to cracks [21, 50]. The mechanical properties of the zirconia are enhanced when the tetragonal phase is stabilized by adding small contents of oxides such as yttrium oxide (or yttria, Y2O3), magnesium oxide (or magnesia, MgO), cerium oxide (or ceria, CeO2), and calcium oxide (or calcia, CaO) [21, 18]. For instance, yttria-stabilized zirconia polycrystals (YTZP) is produced by adding 2–5 mol% yttria to zirconia [21, 18]. That results in a significant increase in the flexural strength values at around 1200 MPa, elastic modulus at 230–270 GPa, and fracture toughness of approximately 9–10 MPa. m1/2 [20, 50]. On high stresses, oxide-stabilized zirconia has an inherent mechanism to inhibit the propagation of cracks. That consists in a transformation of the tetragonal to the monoclinic phase with an increase in the surrounding volume leading to the compression of the crack as seen in Fig. 2. However, YTZP is susceptible to degradation at low temperature when used in a humid environment as the one found in the oral cavity [20, 18, 51]. Tetragonal-to-monoclinic phase transformation can occur under fatigue conditions caused by cyclic stresses with origin in mastication loading and thermal oscillations. In this way, additive oxides such as alumina, ceria, or silica has been used to improve the resistance to low temperature degradation of zirconia [20, 21, 18, 51].
Topography, roughness, and chemical composition control the wettability and adsorption of proteins and ions (e.g., Ca+2, PO−, OH−) onto the zirconia surface prior to the osseointegration [15, 16, 24, 25, 45]. Then, the activation of blood platelets and osteogenic cell migration follow the formation of the primary bioactive layer composed of ions and proteins [45, 23]. The differentiation of osteogenic cells and further formation of collagen matrix and bone tissue depend on the surface features and chemical interaction [45, 52, 23]. Several surface modifications have been proposed to enhance the surface behavior such as grit-blasting, calcium-based coatings, and laser-structuring protocols [10, 13, 17, 22,22,23,24,27]. Nevertheless, zirconia surface modification is a current challenge considering a balance among physical properties, chemical stability, and degradation behavior. Nowadays, most zirconia implants commercially available undergo surface treatment by grit-blasting, which produce non-homogeneous and random surface features under high risks of degradation [23]. Surface modification of zirconia by laser-structuring has been studied and therefore different procedures can be applied regarding the laser type, intensity, time, and mode [12,14,15,16,17,17, 28, 52]. In fact, the wettability and roughness of zirconia surfaces can be enhanced by laser-structuring while maintaining the degradation resistance, biocompatibility, and chemical interaction with the surrounding medium [14,16,16, 51, 45, 52].
Zirconia surface modification
Zirconia implants are often machined by using CAD-CAM systems that results in surfaces with micro-scale grooves or scratches leading to an average roughness (Ra parameter) at around 0.2–0.4 µm [15, 42, 52, 23]. In a previous study, similar roughness values (~ 0.3 µm) were reported on machined MgO-PSZ [16, 45]. Wettability of the MgO-PSZ was measured by the contact angle of glycerol droplet of around 79° [16] while machined Y-PSZ revealed a mean value of 82.4° [15]. In another previous study, the average roughness of sintered Y-TZP was measured at around 1.2 ±0.6 µm [17]. Sintered Y-TZP implants are produced with rough randomly surfaces once the micro-scale peak and valleys at the roughness profile depend on the zirconia powder particle size [12]. On the standard surfaces of Y-TZP implants modified by the grit-blasting method, the average roughness of machined Y-TZP can be increased due to the abrasive effect of airborne particles [14, 29]. As a consequence, morphological features such as micro-scale peaks and valleys are also randomly distributed over the grit-blasted and sintered zirconia surfaces. The average roughness of Y-TZP grit-blasted surfaces has been measured ranging from 1.2 up to 1.6 µm [14, 29].
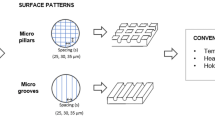
Nevertheless, morphological aspects of zirconia surfaces can be controlled by using the laser irradiation approach. Surfaces of different roughness have been produced by CO2 CW laser and patterned surfaces have been generated with short and ultra-short-pulsed lasers. Well-designed grooves, scratches, valleys, and peaks are produced at macro- and micro-scale width (1–100 µm) and micro-/submicron-scale depth (0.1–10 µm), as shown in Fig. 3 [42]. The roughness and wettability of laser-treated surfaces can also be adjusted considering the implant region and clinical considerations, as seen in Table 1 [14, 16, 45, 29]. In a previous study, a femtosecond la ser irradiation (120 fs, 795 nm, 1 kHz) was used to produce micro-scale pore patterns with 30 µm diameter and 70 µm pitch and micro-grooves with 30 µm width and 70 µm pitch on Y-TZP. The average roughness values of the micro-scale pores’ patterns reached 2.4 ±0.6 µm while micro-grooved surfaces showed roughness values of 9.5 ±0.6 µm. That resulted in an effective surface contact area of 15% on micro-porous surfaces and 25% on micro-grooved surfaces [14, 29]. Another study reported the use of a femtosecond laser irradiation (800 nm, 1 kHz, 30mW) on A-Y-TZP surfaces leading to regular micro-scale grooves’ patterns with 30 µm width and 25 µm depth [12]. Granular polycrystalline structures with dimensions of 1–6 µm and nanostructures with sizes ranging from 30 to 100 nm were detected [14]. In fact, the modification at micro- and nano-scale increased the surface contact area for interaction with proteins and osteogenic cells.
Previous studies reported the modification of MgO-PSZ surfaces by using CO2 laser regarding different laser intensity [16, 45]. Morphologic aspects of the surfaces varied in function of the intensity such as crystal refurbishment on 0.6 kW/cm2; hexagonal structure on 0.9 kW/cm2; pores formation on 1.6 kW/cm2; and dendrite on 2.5 kW/cm2) [16, 45]. Consequently, Ra roughness increased as the power density of the laser irradiation increased (Table 1): Ra roughness was recorded at 0.3 µm on 0.6 kW/cm2; 0.33 µm on 0.9 kW/cm2; 0.71 µm on 1.6 kW / cm2); 1.8 µm on 1.9 kW/cm2; and 3.8 µm on 2.5 kW/cm2 [16, 45]. On the MgO-PSZ surfaces, the angle of contact of the glycerol droplet decreased as the roughness increased that indicates an increase in wettability: 76° on 0.6 kW / cm2; 62° on 0.9 kW/cm2; 40° on 1.6 kW/cm2; 50° on 1.9 kW/cm2; and 54° on 2.5 kW/cm2 [16]. However, a significant decrease in the Ra roughness was detected on Y-PSZ when the CO2 laser intensity was increased; although, the morphological aspects also varied as a hexagonal microstructure appeared on 1.8 kW/cm2, while a porous microstructure was noted on 2.25 kW/cm2. The mean values of the contact angle of the glycerol droplet also decreased with the increase in laser power: 74.2° was recorded on 1.80 kW/cm2, while an angle of 70.5° was recorded on 2.25 kW/cm2 [15].
On Er, Cr: YSGG laser at low level irradiation, no significant changes were detected on Y-TZP using the following parameters: 1.5 W (Ra of 1.52 ±2.0 µm and Sa of 1.78 ±2.0 µm); 3.0 W (Ra of 1.14 ±0.7 µm and Sa of 1.24 ±1.3 µm); and 5.0 W (Ra of 0.70 ±0.3 µm and Sa of 1.36 ±1.0 µm) [17]. However, micro-scale scratches and grooves were detected in another study assessing a laser irradiation of 3 W on Y-TZP surface that resulted in a Ra roughness at 1.41 ±0.166 µm and Rz roughness at 5.1 ± 0.327 µm [44]. A fiber laser was also used to produce changes on the Y-TZP surfaces, and therefore the results revealed regular edges’ pattern leading to an increase in roughness at around 10 times (Sa of 1.75 ±0.32 µm) when compared to machined surf aces (Sa of 0.18 ±0.04 µm) [52].
Biological response to surface characteristics produced by laser
In vitro studies on cell culture have shown stimuli of the osteogenic cell response on laser-treated zirconia, as illustrated in Table 1 [15,17,17]. For instance, zirconia surface treated with CO2 laser revealed a significant increase in the osteogenic cell proliferation by 70–90% when compared to untreated zirconia [15, 16]. The laser energy used in the surface treatment of zirconia has an active effect on the surface morphologic aspects , which in turn influenced the osteogenic cell behavior [15,17,17]. The osteogenic cell proliferation is significantly increased when the laser intensity was increased [15,17,17]. A progressive increase in cell proliferation was noted on Y-TZP irradiated with Er, Cr: YSGG laser with wavelength of 2780 nm, for 30 s and 20 Hz on 1.5 W, 3 W, or 5 W when compared to untreated zirconia [17]. Another study with Er,Cr:YSGG laser at 20 Hz and 3 W reported a significant difference in cell proliferation for 3 and 7 days cell incubation. Viable cell count was measured at [23 ± 1.9] × 103 and [37.5 ± 1.2] × 103 for laser-treated Y-TZP and [51 ±1.4] × 103 and [72 ±2.1] × 103 for untreated zirconia [44].
The morphological aspects of the osteoblast have been reported in previous studies by evaluating projections of cytoplasm, namely phyllopodia, and the spreading of the cell over the surfaces [15,17,17, 42, 52]. The cells exhibited a final stage of cell adhesion, showing more flattened and with a higher cytoplasmic projection with phyllopod that extended about 50–60 µm beyond the cells when compared to smaller phyllopods (5 to 10 µm projections) on untreated surfaces [15, 16]. The degree of maturation achieved by osteoblasts after contact with leaser-treated Y-TZP surfaces is another important aspect to be considered, since it is a key factor for the production of the bone matrix [42, 52]. A higher degree of cell differentiation on laser-treated surfaces was validated by measuring osteogenic genes, such as collagen type I, osteopontin, osteocalcin, and BMP-2 [42]. Results showed values ranging from 7 up to 25 times higher for laser-treated Y-TZP compared to untreated surfaces over a period of 7-days incubation [42]. Remarkable changes in cell morphologic aspects were evaluated by a previous study [52] at approximately 3 times for irradiated Y-TZP when compared to the non-irradiated Y-TZP [52]. The morphologic changes were linked to an increase in the gene expression of Runx2 mRNA, alkaline phosphatase, and oxytocin mRNA for 3, 7, and 14 days incubation, respectively [52]. Those are essential transcriptional factors for the differentiation of osteoblasts. Thus, laser-assisted surface modifications increased the gene expression related to time-dependent osteogenic differentiation.
Studies have shown similar BIC values for titanium or zirconia implant surfaces treated with laser irradiation [13, 46, 53]. In American Foxhound dogs, mean BIC percentage was recorded at 44.6 ± 17.6% on zirconia for 1 month and 47.9 ±16% for 3 months. No statistically differences were found when compared to titanium implant surfaces regarding the BIC mean values at 51.3 ±12% for 1 month and at 61.7 ±16.2% for 3 months [13]. In another study in American Foxhound dogs, laser-treated zirconia implant surfaces showed the BIC mean values at 22.8 ±1.5% for 1 week and 37.5 ±2.1% for 4 weeks [46]. Those values were also not statistically different when compared to BIC values for titanium surfaces: 25.4 ±1.2% for 1 week and 38.4 ±1.8% for 4 weeks [46]. Similar results were found in another study in New Zealand white rabbits regarding the BIC mean values recorded on laser-treated zirconia implants at 39.97 ± 13.19% for 6 weeks and 43.87 ±14.54% for 12 weeks in comparison to BIC mean values on titanium implant surfaces at 34.15 ±10.34% for 6 weeks and 34.82 ±12.21% for 12 weeks [53]. Thus, the laser treatment is capable of modif ying the surface topographic aspects of zirconia for an enhanced osseointegration as compared to titanium implant surfaces [14, 46]. BIC studies in Wistar rats showed no statistically differences between Y-TZP (56.2 ±3.56%) and Ce-TZP (37.1 ±14.01%) with grit-blasted surface treatment and acidic etching for 4 weeks [43]. However, the laser-treated Y-TZP surfaces by using Nd:YAG wavelength 1064 nm, pulse of 3 ns, 50 Hz, and 150 mJ/pulse revealed higher BIC mean values (78.9 ±6.57%) when compared to laser-treated Ce-TZP (14.0 ±2.43%) [43].
In the comparison between machined and laser-treated Y-TZP implants, within a period of 4 weeks, BIC mean values were 2 times higher (81.9 ± 20.4%) in the cortical bone portion in the Sprague–Dawley rats when compared to those for machined Y-TZP surfaces (39.8 ± 19.2%). In the cancellous bone portion, BIC mean values did not show significant differences [52]. In the evaluation of the BIC percentage between zirconia implants with different surface treatments, no statistically significant differences were found between the Y-TZP surfaces with different surface treatments for 6 or 12 weeks respectively: 33 ±14% and 33.7 ±14.5% on sintered zirconia; 39.6 ±15% and 41.3 ±15.8% on grit-blasted; and 39.97 ±13.19% and 43.87 ±14.54% on laser-treated surface [53]. Regarding occlusal loading, Y-TZP implants treated with femtosecond lasers, subjected to immediate loading, showed higher BIC values for 1 month (38.9 ± 6.68%) and 3 months (65 ±4.36%) when compared to the same implant condition free of occlusal loading (32 ±3.65%) for 1 month and (57.6 ±3.62%) for 3 months. Findings revealed a statistically significant improvement of the BIC percentage when implants were immediately loaded [47].
In a Foxhound dogs model, Y-TZP zirconia implants treated with femtosecond laser (100 fs, 795 nm, 10nJ, 80 MHz), near-infrared wavelengths 795 nm and 10 nJ energy with a 80 MHz, showed marginal bone crest resorption values at 0.01 ±0.57 mm for 1 month and at 1.25 ± 1.73 mm for 3 months [13]. These values were statistically significant only in the 3-month period when compared to the marginal bone crest resorption values in titanium implants: 0.77 ±0.69 mm for 1 month and 0.37 ±0.34 mm for 3 months [13]. Another study reported findings on Y-TZP zirconia implants treated by using femtosecond on the entire implant body or only on the implant neck [29]. After 3 months, zirconia implants treated with laser at the neck region revealed a higher crestal bone loss (0.36 ±0.01 mm) when compared to the implants treated in the entire contact surfaces (0.26 ±0.01 mm) [46]. Immediately, loaded Y-TZP zirconia implants showed crestal bone loss values of 0.5 ±0.3 mm for 1 month and 0.5 ±0.23 mm for 3 months [47].
Conclusions
Within the limitations of the previous studies, the following outcomes can be drawn:
-
The surface treatment performed by laser-assisted techniques generated changes in the surface roughness parameters, producing textures at meso-, micro-, and nano-scale leading to a enhanced surface wettability.
-
The laser treatment produced a favorable response in the initial levels of adhesion and proliferation of osteoblasts on the zirconia surface when compared to untreated zirconia surfaces.
-
A high BIC percentage was recorded on the laser-treated zirconia surfaces that corresponded to enhanced osseointegration. Similar values of bone-implant contact were found on standard titanium implants and laser-treated zirconia implants.
-
Further studies are required to establish optimum processing parameters for each type of laser used in the surface treatment of different zirconia-based materials.
References
Adell R, Hansson BO, Brånemark PI, Breine U (1970) Intra-osseous anchorage of dental prostheses. Scand J Plast Reconstr Surg Hand Surg 4:19–34. https://doi.org/10.3109/02844317009038440
Brånemark PI, Adell R, Albrektsson T, Lekholm U, Lundkvist S, Rockler B (1983) Osseointegrated titanium fixtures in the treatment of edentulousness. Biomaterials 4:25–28. https://doi.org/10.1016/0142-9612(83)90065-0
Souza JCM, Sordi MB, Kanazawa M, Ravindran S, Henriques B, Silva FS, Aparicio C, Cooper LF (2019) Nano-scale modification of titanium implant surfaces to enhance osseointegration. Acta Biomater. 94:112–131. https://doi.org/10.1016/j.actbio.2019.05.045.E
Brånemark R, Öhrnell LO, Nilsson P, Thomsen P, Tool T, Suwandi JS, Toes REM, Nikolic T, Roep BO, Ferguson SJ et al (2008) Biomechanical characterization of osseointegration during healing: an experimental in vivo study in the rat. Clin Exp Rheumatol 18:97–103. https://doi.org/10.1002/jbm.a
Bergemann C, Duske K, Nebe JB, Schöne A, Bulnheim U, Seitz H, Fischer J (2015) Microstructured zirconia surfaces modulate osteogenic marker genes in human primary osteoblasts. J Mater Sci Mater Med 26:1–11. https://doi.org/10.1007/s10856-014-5350-x
Albrektsson T, Sennerby L, Wennerberg A (2000) State of the art of oral implants. Periodontol 2008(47):15–26. https://doi.org/10.1111/j.1600-0757.2007.00247.x
Gahlert M, Roehling S, Sprecher CM, Kniha H, Milz S, Bormann K (2011) In vivo performance of zirconia and titanium implants : a histomorphometric study in mini pig maxillae. Clin Oral Implants Res 23:281–286. https://doi.org/10.1111/j.1600-0501.2011.02157.x
Depprich R, Zipprich H, Ommerborn M, Naujoks C, Wiesmann H-P, Kiattavorncharoen S, Lauer H-C, Meyer U, Kübler NR, Handschel J (2008) Osseointegration of zirconia implants compared with titanium: an in vivo study. Head Face Med 4:30. https://doi.org/10.1186/1746-160X-4-30
Depprich R, Ommerborn M, Zipprich H, Naujoks C, Handschel J, Wiesmann HP, Kübler NR, Meyer U (2008) Behavior of osteoblastic cells cultured on titanium and structured zirconia surfaces. Head Face Med 29:1–9. https://doi.org/10.1186/1746-160X-4-29
Rocchietta I, Fontana F, Addis A, Schupbach P, Simion M (2009) Surface-modified zirconia implants: tissue response in rabbits. Clin Oral Implants Res 20:844–850. https://doi.org/10.1111/j.1600-0501.2009.01727.x
Schliephake H, Hefti T, Schlottig F, Gédet P, Staedt H (2010) Mechanical anchorage and peri-implant bone formation of surface-modified zirconia in minipigs. J Clin Periodontol 37:818–828. https://doi.org/10.1111/j.1600-051X.2010.01549.x
Aivazi M, hossein Fathi M, Nejatidanesh F, Mortazavi V, HashemiBeni B, Matinlinna JP, Savabi O (2016) The evaluation of prepared microgroove pattern by femtosecond laser on alumina-zirconia nano-composite for endosseous dental implant application. Lasers Med Sci 31:1837–1843. https://doi.org/10.1007/s10103-016-2059-8
Calvo-Guirado JL, Aguilar-Salvatierra A, Delgado-Ruiz RA, Negri B, Fernández MPR, Maté Sánchez de Val JE, Gómez-Moreno G, Romanos GE (2013) Histological and histomorphometric evaluation of zirconia dental implants modified by femtosecond laser versus titanium implants: an experimental study in fox hound dogs. Clin Implant Dent Relat Res 17:525–532. https://doi.org/10.1111/cid.12162
Delgado-Ruíz RA, Calvo-Guirado JL, Moreno P, Guardia J, Gomez-Moreno G, Mate-Sánchez JE, Ramirez-Fernández P, Chiva F (2011) Femtosecond laser microstructuring of zirconia dental implants. J Biomed Mater Res Part B Appl Biomater. 96 B:91–100. https://doi.org/10.1002/jbm.b.31743
Hao L, Lawrence J, Chian KS (2005) Osteoblast cell adhesion on a laser modified zirconia based bioceramic. J Mater Sci Mater Med 16:719–726. https://doi.org/10.1007/s10856-005-2608-3
Hao L, Lawrence J, Chian KS (2004) Effects of CO2 laser irradiation on the surface properties of magnesia-partially stabilised zirconia (MgO-PSZ) bioceramic and the subsequent improvements in human osteoblast cell adhesion. J Biomater Appl 19:81–105. https://doi.org/10.1177/0885328204043546
Soares RD, Rodrigues JA, Cassoni A, Cruz A, Simoes CO, Pasqua-Neto JD, Gehrke SA, Blay A, Cesar PF, Shibli JA (2016) In vitro behavior of osteoblasts on zirconia after different intensities of erbium, chromium-doped: yttrium, scandium, gallium, and garnet-laser irradiation. J Craniofac Surg 27:784–788. https://doi.org/10.1097/SCS.0000000000002429
Zhang Y, Lawn BR (2018) Novel Zirconia Materials in Dentistry. J Dent Res 97(2):140–147. https://doi.org/10.1177/0022034517737483
Pessanha-Andrade M, Sordi MB, Henriques B, Silva FS, Teughels W, Souza JCM (2018) Custom-made root-analogue zirconia implants: A scoping review on mechanical and biological benefits. J Biomed Mater Res B Appl Biomater. 106(8):2888–2900. https://doi.org/10.1002/jbm.b.34147
Zhang Y (2012) Overview: Damage resistance of graded ceramic restorative materials. J Eur Ceram Soc 32(11):2623–2632. https://doi.org/10.1016/j.jeurceramsoc.2012.02.020
Garvie RC, Hannink RH, Pascoe RT (1975) Ceramic steel? Nature 258:703–704. https://doi.org/10.1038/258703a0
Gahlert M, Gudehus T, Eichhorn S, Steinhauser E, Kniha H, Erhardt W (2007) Biomechanical and histomorphometric comparison between zirconia implants with varying surface textures and a titanium implant in the maxilla of miniature pigs. Clin Oral Implants Res 18:662–668
Schünemann FH, Galárraga-Vinueza ME, Magini R, Fredel M, Silva F, Souza JCM, Zhang Y, Henriques B (2019) Zirconia surface modifications for implant dentistry. Mater Sci Eng C Mater Biol Appl. 98:1294–1305. https://doi.org/10.1016/j.msec.2019.01.062
Gouveia PF, Mesquita-Guimarães J, Galárraga-Vinueza ME, Souza J, Silva FS, Fredel MC, Boccaccini AR, Detsch R, Henriques B (2021) In-vitro mechanical and biological evaluation of novel zirconia reinforced bioglass scaffolds for bone repair. J Mech Behav Biomed Mater 114:104164. https://doi.org/10.1016/j.jmbbm.2020.104164
Peñarrieta-Juanito G, Cruz M, Costa M, Miranda G, Marques J, Magini R, Mata A, Souza JCM, Caramês J, Silva FS (2018) A novel gradated zirconia implant material embedding bioactive ceramics: Osteoblast behavior and physicochemical assessment. Materialia 1:3–14. https://doi.org/10.1016/j.mtla.2018.07.002
Hirota M, Hayakawa T, Ohkubo C, Sato M, Hara H, Toyama T, Tanaka Y (2014) Bone responses to zirconia implants with a thin carbonate-containing hydroxyapatite coating using a molecular precursor method. J Biomed Mater Res Part B Appl Biomater. 102:1277–1288. https://doi.org/10.1002/jbm.b.33112
Lee J, Sieweke JH, Rodriguez NA, Schüpbach P, Lindström H, Susin C, Wikesjö UME (2009) Evaluation of nano-technology-modified zirconia oral implants: a study in rabbits. J Clin Periodontol 36:610–617. https://doi.org/10.1111/j.1600-051X.2009.01423.x
Han J, Zhang F, Van Meerbeek B, Vleugels J, Braem A, Castagne S (2021) Laser surface texturing of zirconia-based ceramics for dental applications: A review. Mater Sci Eng C Mater Biol Appl 123:112034. https://doi.org/10.1016/j.msec.2021.112034
Delgado-Ruíz RA, Marković A, Calvo-Guirado JL, Lazić Z, Piattelli A, Boticelli D, Maté-Sánchez JE, Negri B, Ramírez-Fernández MP, Mišić T (2014) Implant stability and marginal bone level of microgrooved zirconia dental implants: a 3-month experimental study on dogs. Vojnosanit Pregl 71:451–461. https://doi.org/10.2298/VSP121003034D
Henriques B, Hammes N, Souza JCM, Özcan M, Mesquita-Guimarães J, Silva FS, Fredel MC, Volpato CM, Carvalho O (2020) Influence of ns-Nd:YAG laser surface treatment on the tensile bond strength of zirconia to resin-matrix cements. Ceramics International 46(17):27822–27831. https://doi.org/10.1016/j.ceramint.2020.07.281
Gomes AL, Ramos JC, Santos-del Riego S, Montero J, Albaladejo A (2015) Thermocycling effect on microshear bond strength to zirconia ceramic using Er:YAG and tribochemical silica coating as surface conditioning. Lasers Med Sci. https://doi.org/10.1007/s10103-013-1433-z
Paranhos MPG, Burnett LH, Magne P (2011) Effect Of Nd:YAG laser and CO2 laser treatment on the resin bond strength to zirconia ceramic. Quintessence Int
Aras WMF, Barroso JSM, Blay A, Rodrigues JA, Cassoni A (2016) Er, Cr:YSGG laser irradiation influence on Y-TZP bond strength to resin cement. Ceram Int. https://doi.org/10.1016/j.ceramint.2016.05.180
Abu Ruja M, De Souza GM, Finer Y (2019) Ultrashort-pulse laser as a surface treatment for bonding between zirconia and resin cement. Dent Mater. https://doi.org/10.1016/j.dental.2019.07.009
Rocca J-P, Fornaini C, Brulat-Bouchard N, Bassel Seif S, Darque-Ceretti E (2014) CO2 and Nd:YAP laser interaction with lithium disilicate and Zirconia dental ceramics: a preliminary study. Opt Laser Technol 57:216–223. https://doi.org/10.1016/j.optlastec.2013.10.008
Souza JCM, Fernandes V, Correia A, Miller P, Carvalho O, Silva FS, Özcan M, Henriques B, Surface modification of glass fiber-reinforced composite posts to enhance their bond strength to resin-matrix cements: an integrative review. Clinical Oral Investigations https://doi.org/10.1007/s00784-021-04221-y
Lopes-Rocha L, Ribeiro-Gonçalves L, Henriques B, Özcan M, Tiritan ME, Souza JCM (2021) An integrative review on the toxicity of Bisphenol A (BPA) released from resin composites used in dentistry. Journal of Biomedical Materials Research Part B: Applied Biomaterials 109(11):1942–1952. https://doi.org/10.1002/jbm.b.34843
Fernandes V, Silva AS, Carvalho O, Henriques B, Silva FS, Özcan M, Souza JCM (2021) The resin-matrix cement layer thickness resultant from the intracanal fitting of teeth root canal posts: an integrative review. Clinical Oral Investigations 25(10):5595–5612. https://doi.org/10.1007/s00784-021-04070-9
Tafur-Zelada C, Carvalho O, Silva FS, Henriques B, Özcan M, Souza JCM (2021) The influence of zirconia veneer thickness on the degree of conversion of resin-matrix cements: an integrative review. Clinical Oral Investigations 25(6):3395–3408. https://doi.org/10.1007/s00784-021-03904-w
Messous R, Henriques B, Bousbaa H, Silva FS, Teughels W, Souza JCM (2021) Cytotoxic effects of submicron- and nano-scale titanium debris released from dental implants: an integrative review. Clinical Oral Investigations 25(4):1627–1640. https://doi.org/10.1007/s00784-021-03785-z
Souza JCM, Pinho SS, Pranto Braz M, Silva FS, Henriques B (2021) Carbon fiber-reinforced PEEK in implant dentistry: A scoping review on the finite element method. Computer Methods in Biomechanics and Biomedical Engineering 24(12):1355–1367. https://doi.org/10.1080/10255842.2021.1888939
Rezaei NM, Hasegawa M, Ishijima M, Nakhaei K, Okubo T, Taniyama T, Ghassemi A, Tahsili T, Park W, Hirota M et al (2018) Biological and osseointegration capabilities of hierarchically (meso-/micro-/nano-scale) roughened zirconia. Int J Nanomedicine 13:3381–3395. https://doi.org/10.2147/IJN.S159955
Hirota M, Harai T, Ishibashi S, Mizutani M, Hayakawa T (2019) Cortical bone response toward nanosecond-pulsed laser-treated zirconia implant surfaces. Dent Mater J 38:444–451. https://doi.org/10.4012/dmj.2018-153
Nassif W, Rifai M (2018) Surface characterization and cell adhesion of different zirconia treatments: an in vitro Study. J Contemp Dent Pract 19:181–188. https://doi.org/10.5005/JP-JOURNALS-10024-2234
Hao L, Lawrence J, Chian KS, Low DKY, Lim GC, Zheng HY (2004) The formation of a hydroxyl bond and the effects thereof on bone-like apatite formation on a magnesia partially stabilized zirconia (MgO-PSZ) bioceramic following CO 2 laser irradiation. J Mater Sci Mater Med 15:967–975. https://doi.org/10.1023/B:JMSM.0000042682.20595.74
Calvo-Guirado JL, Aguilar Salvatierra A, Gargallo-Albiol J, Delgado-Ruiz RA, Maté Sanchez JE, Satorres-Nieto M (2014) Zirconia with laser-modified microgrooved surface vs. titanium implants covered with melatonin stimulates bone formation. Experimental study in tibia rabbits. Clin Oral Implants Res 26:1421–1429. https://doi.org/10.1111/clr.12472
Calvo-Guirado JL, Aguilar-Salvatierra A, Gomez-Moreno G, Guardia J, Delgado-Ruiz RA, Mate-Sanchez de Val JE (2014) Histological, radiological and histomorphometric evaluation of immediate vs. non-immediate loading of a zirconia implant with surface treatment in a dog model. Clin. Oral Implants Res 25:826–830. https://doi.org/10.1111/clr.12145
Glauser R, Sailer I, Wohlwend A, Studer S, Schibli M, Schärer P (2004) Experimental zirconia abutments for implant-supported single-tooth restorations in esthetically demanding regions: 4-year results of a prospective clinical study. Int J Prosthodont 17:285–290
Kohal RJ, Klaus G (2004) A zirconia implant-crown system: a case report. Int J Periodontics Restorative Dent 24:147–153
Piconi C, Maccauro G, Muratori F, Brach Del Prever E (2003) Alumina and zirconia ceramics in joint replacements. J Appl Biomater Biomech 1:19–32. https://doi.org/10.1177/228080000300100103
Kohorst P, Borchers L, Strempel J, Stiesch M, Hassel T, Bach FW, Hübsch C (2012) Low-temperature degradation of different zirconia ceramics for dental applications. Acta biomaterialia 8(3):1213–1220. https://doi.org/10.1016/j.actbio.2011.11.016
Taniguchi Y, Kakura K, Yamamoto K, Kido H, Yamazaki J (2015) Accelerated osteogenic differentiation and bone formation on zirconia with surface grooves created with fiber laser irradiation. Clin Implant Dent Relat Res 18:883–894. https://doi.org/10.1111/cid.12366
Hoffmann O, Angelov N, Zafiropoulos G-G, Andreana S (2012) Osseointegration of zirconia implants with different surface characteristics: an evaluation in rabbits. Int J Oral MaxIllOfac Implant 27:352–358
Scarano A, Piattelli M, Caputi S, Favero GA, Piattelli A (2004) Bacterial adhesion on titanium nitride-coated and uncoated implants: an in vivo human study. J Periodontol 75:292–296. https://doi.org/10.1563/1548-1336(2003)029%3c0080:BAOTNA%3e2.3.CO;2
Deville S, Chevalier J, Gremillard L (2006) Influence of surface finish and residual stresses on the ageing sensitivity of biomedical grade zirconia. Biomaterials 27:2186–2192. https://doi.org/10.1016/j.biomaterials.2005.11.021
Funding
The authors acknowledge the support provided by the following FCT-Portugal projects: UID/EEA/04436/2013, SFRH/BPD/123769/ 2016, and LaserMULTICER [POCI-01–0145-FEDER-031035].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors declare no conflict of interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cunha, W., Carvalho, O., Henriques, B. et al. Surface modification of zirconia dental implants by laser texturing. Lasers Med Sci 37, 77–93 (2022). https://doi.org/10.1007/s10103-021-03475-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-021-03475-y