Abstract
The use of zirconia for implants and abutments has become more prevalent in implant dentistry as an alternative to the commonly used titanium implants, and peri-implant disease can still affect them. The erbium, chromium-doped:yttrium-scandium-gallium-garnet (Er, Cr:YSGG) laser has emerged as a promising treatment modality. The purposes of this in vitro study were to (1) determine the effects of the laser on the surface roughness of zirconia discs; (2) determine the extent of removal of a single species biofilm, E. coli, on the zirconia discs after applying the laser; (3) determine the amount of cell adhesion and proliferation utilizing fibroblasts on zirconia discs after treatment with the laser. All treatments will be compared with the commonly used ultrasonic instrumentation and hand scalers. For the first aim, gross examination revealed noticeable surface damage on the discs when using ultrasonic and scalers but not for the laser group. For surface roughness, the mean roughness was Pa= 0.623±0.185 μm, 0.762±0.421 μm, 0.740±0.214 μm, and 0.724±0.168 μm for control discs, and discs treated with either the Er,Cr:YSGG laser, ultrasonic instrumentation, and hand scalers respectively. There was no statistical significance among the groups (p=0.628). For bacteria decontamination, there was a statistical significance among the groups (p< 0.0001). Statistical significance was seen between the control group and each of the three treatment groups, favoring the treatment groups (p< 0.0001). Statistical significance was seen when comparing ultrasonic instrumentation and hand scalers (p= 0.000) as well as when comparing the Er,Cr:YSGG laser to hand scalers (p= 0.007), favoring both the ultrasonic instrumentation and Er,Cr:YSGG laser. No significance between the Er,Cr:YSGG laser group and the ultrasonic instrumentation group was noted (p =0.374). When comparing the cell attachment following treatment in each of the three groups and also without treatment (control), there was a statistical significance among the groups (p<0.0001) in terms of total cell count, favoring the control and the laser groups. Further evaluations with SEM showed differences in cell morphology indicating more adherent cells on Er,Cr:YSGG laser–treated surfaces. In conclusion, gross examination of the discs show clear surface changes when using ultrasonic instrumentation and hand scalers compared to the Er,Cr:YSGG laser group. The Er,Cr:YSGG laser was able to effectively ablate bacteria from zirconia disc. Fibroblast attachment on the surfaces of the zirconia discs shows more adherence when treated with Er,Cr:YSGG laser.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The use of endosseous dental implants has been a widely accepted treatment modality for patients since their introduction in 1977 [1]. Complications have become more frequent since their implementation due to the prevalence of peri-implant disease such as peri-implant mucositis and peri-implantitis. Recently, the World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions defined peri-implant disease and conditions to give us a definitive definition and description of peri-implant health, peri-implant mucositis, and peri-implantitis based on a review of the literature [2]. Peri-implant mucositis has been reported to occur in approximately 80% of patients, and peri-implantitis occurs in between 28 to 56% of patients [3]. This represents an important aspect of implant dentistry that requires multiple treatment modalities in order to ensure long-term success of dental implants.
Treatment of dental implants must be considered in a different manner than natural teeth due to the use of threads on the implant that engage into the alveolar bone for osseointegration that makes it difficult to fully decontaminate due to access. Furthermore, the abutment of the implant represents another site of potential biofilm accumulation that must be addressed when treating peri-implant diseases. This makes the treatment of dental implants more complicated. Multiple treatment protocols have been described for maintenance of implants or treatment of peri-implant inflammatory diseases [4].
Recently, the use of zirconia (zirconia-dioxide, ZrO2) has been used more widely as a substitute for the more traditionally used titanium implants as well as a material for the abutment in the final restoration. Transmucosal zirconia implant abutments have been shown to have safe long-term functional and esthetic results as well as favorable soft and hard tissue reaction [5]. It has also been shown to be favorable for use as an abutment due to having a low bacterial adherence after evaluation of zirconia discs that have been left in the oral cavity for 24 h [6]. Zirconia implants have been shown to be successful when used to support dental prostheses. A recent systematic review found that the overall survival rate of zirconia implants after 1 year of function was 92% [7]. It has been shown to have a high level of acceptance in terms of treatment modality for patients and has similar clinical results in terms of bleeding on probing, probing depths, and attachment levels compared to natural teeth [8]. With the more widespread use of zirconia in implant dentistry, it becomes more necessary to evaluate treatment modalities for when they are affected with peri-implant diseases either at the abutment or fixture level.
The use of dental lasers has been reported for nonsurgical treatment of periodontal diseases [9, 10]. Furthermore, the use of lasers has shown promising results around dental implants as well [11]. The erbium, chromium-doped:yttrium, scandium, gallium, and garnet (Er,Cr:YSGG) laser has a wavelength of 2780 nm. The laser energy allows for microablation of tooth structure, bone, or soft tissue. It has been used for surgical treatment of peri-implant disease as well as nonsurgical use [12,13,14]. This has led to promising results on the management of this complicated ailment for dental implants.
The efficacy of the Er, Cr: YSGG laser on decontamination and surface changes is correlated with parameters such as power (watts), frequency (Hz), pulse duration, diameter of the tips, and distance between the tips to the irradiated surfaces [15]. A recent in vitro study showed that use of both conical and side firing tips at 1.5 W/30 Hz did not seem to damage the titanium implant surface [16]. Another study showed that when 2.5 W/25 Hz was used, oral biofilm was effectively removed from contaminated titanium; however, this study did not report whether there were surface changes [17].
There is a paucity of reports on the management of peri-implant disease around zirconia; therefore, this in vitro study hopes to (1) determine the effects of using the Er,Cr:YSGG laser on the surface modification of zirconia discs; (2) determine the extent of removal of a single species biofilm, E. coli, on the zirconia discs; and (3) determine the amount of cell adhesion and proliferation as well as examine the morphology of fibroblasts on zirconia discs after treatment. All treatments will be compared with the commonly used ultrasonic instrumentation and hand scalers.
Materials and methods
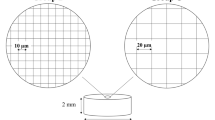
Zirconia disc preparation
Yttria-stabilized zirconia (YTZP) discs, sintered and polished, were obtained from a dental laboratory (Cusp Dental Research Inc, MA, USA). Each disc measured 10 mm in diameter and 2 mm in thickness. Prior to any treatment, discs were ultrasonically cleaned and degreased in 0.5% sodiumdodecyl sulfate (SDS; Sigma, MO, USA), deionized water, acetone (Sigma, MO, USA) and ethanol (Sigma, MO, USA), sequentially, for 20 min in each solvent, and then autoclaved at 121 °C for 20 min.
Surface treatment
For each aim, the discs were divided and treated the same way:
-
1)
Control group (no treatment)
-
2)
Laser-treated group: discs were treated with the Er,Cr:YSGG laser (Waterlase iPlus, Biolase, Irvine, CA, USA) with a wavelength of 2780 nm in short pulse “H” mode (60μs, pulse rate 30 Hz) via an end firing tip with a spot size of 1 mm. The power setting was 1.5 W with air/water of 40%/50% to simulate the recommended clinical setting for treatment of peri-implant disease using this laser. The laser tip, attached to a handle, was slowly moved along the zirconia surface while keeping a distance of about 0.5 mm between the tip and the surface.
-
3)
Ultrasonic instrumentation–treated group: discs were treated with cavitron (Cavitron Plus Ultrasonic Scaler, Dentsply Sirona, York, PA, USA) instrumentation with 20 strokes of the instrument on each disc.
-
4)
Hand instrumentation–treated group: discs were treated with stainless steel periodontal curettes (Younger Good 7-8 Curette Hu-Friedy, Chicago, Il, USA) with 20 strokes of the instrument on each disc.
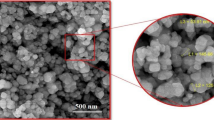
Surface characterization
After treatment of each disc on both sides following the assigned group protocol (n=5 surfaces per group), the disc surfaces were analyzed by three different methods. (1) Gross visual examination of the discs was completed to determine the effects of each instrument on the discs. (2) Scanning electron microscopy (SEM) (Zeiss Ultra55 field emission scanning electron microscope; ZEISS, Oberkochen, Germany) analysis was completed to examine any noticeable change in surface texture. (3) A surface contact profilometer (DetakXT Profilometer, Bruker, Billerica, MA, USA) was utilized to calculate the average surface roughness (Pa in μm) for each disc. Measurements were made 5 times at random on each disc surface, moving for a distance of 1 mm, and at 3 mg of stylus force. Measurements of surface roughness were averaged together for each disc for quantitative analysis.
Bacteria culture
To investigate the efficacy of different surface decontamination treatments, discs (n=12 per group) were inoculated with green fluorescent protein (GFP)–expressing Escherichia coli (ATCC 25922GFP) for 24 h. In specific, E. coli culture was grown overnight in a shaker at 28 °C for 24 h in the Lysogeny broth (LB) until OD600 reached 0.4~0.5. Subsequently, bacterial concentration was adjusted to 2×106/mL with LB. In a 24-well plate, discs were placed into each well and immersed in 1 mL E. coli containing LB for 24 h into each well. Four discs per group were used. At the end of the incubation, non-adherent bacteria were rinsed off with phosphate buffered saline (PBS) and each disc was treated according to the assigned group protocol (control, Er, Cr:YSGG, ultrasonic instrumentation and hand scalers) as described previously. Following treatments, the discs were rinsed with PBS, fixed in 4% paraformaldehyde (PFA) for 10 min and then washed twice with PBS before being mounted for fluorescent microscopy. A fluorescence microscope (Revolve, ECHO, CA, USA) with ×10 objective was used to examine the discs. Fluorescent photographs were taken with a 3.2 MP monochrome SCMOS camera at 3 random sites on each disc. A cell count was completed using ImageJ (National Institutes of Health, Bethesda, MD, USA) to examine the effectiveness of removal of the bacteria from each of the discs. These values were averaged for each group for comparison.
Fibroblast cell adhesion
For the third aim, 5 discs were used for each group for quantitative analysis with a cell count using luminescent cell viability kit (CellTiter-Glo Luminescent Cell Viability Assay, Promega, Madison, WI, USA) and 3 discs for each group were used for SEM qualitative analysis (total of n=8 per group). Discs were initially treated according to the assigned group protocols and autoclaved prior to cell incubation. Mouse fibroblast NIH3T3 cells were maintained in DMEM medium (Thermo Fisher Scientific) supplemented with 10% FBS at 37 °C in 5% CO2 and 95% atmospheric air. Cells were seeded on the 4 types of treatment surfaces at 50k cells/cm2 in 1 mL of culture medium in each well of a 24-well plate for 72 h. At the end of the incubation period, unbound cells were washed off with the culture medium and specimens were transferred to a new well where a 400-μL mixture of culture medium and CellTiterGlo solution at 1:1 ratio was added. Cell lysis was induced by 2-min vigorous shaking with an orbital shaker, and the plate was left to stabilize for 10 min before luminescent reading. Three discs from each group were fixated with 4% PFA, and then SEM analysis was completed to examine the morphology of the attached fibroblasts on the discs.
Statistical analyses
One-way analysis of variance (ANOVA) was conducted to compare measurements between the control and test groups, and the Tukey HSD post hoc test was applied to assess differences that were statistically significant. Data that did not show normal distribution after testing for normality was analyzed using the Kruskal-Wallis non-parametric test and post hoc Dunn’s multiple comparison test. The significance level adopted was 5% for all tests.
Results
Surface modification
After treatment with each group, gross examination revealed noticeable surface damage on the discs when using ultrasonic and scalers but no noticeable damage with the laser group (Fig. 1a, upper row). When compared to the control, the Er,Cr:YSGG laser–treated discs showed similar appearance after treatment. SEM analyses show minimal changes between groups (Fig. 1a, lower row). For surface roughness, the mean roughness were Pa= 0.623±0.185 μm, 0.762±0.421 μm, 0.740±0.214 μm, and 0.724±0.168 μm for control discs, and discs treated with either the Er,Cr:YSGG laser, ultrasonic instrumentation, and hand scalers respectively (Table 1 and Fig. 1b). There was no statistical significance among the groups (p=0.628).
Surface characterization following different treatments. a Upper row: gross examination of each disc after treatment. Lower row: SEM analysis of each disc after treatment at ×1000 magnification. b Surface roughness after measurements with profilometer. There was no statistical significance among the groups
Bacteria decontamination
For bacteria decontamination, there was a statistical significance among the groups (p< 0.0001), and we can see the noticeable difference when examining the discs under fluorescence microscopy (Fig. 2a). Statistical significance in the number of bacteria after performing a cell count was seen between the control group and each of the three treatment groups, favoring the treatment groups (p < 0.0001). Post hoc Dunn’s multiple comparison test revealed statistical significance when comparing ultrasonic instrumentation and hand scalers (p=0.000) as well as when comparing the Er,Cr:YSGG laser to hand scalers (p=0.007), favoring both the ultrasonic instrumentation and Er,Cr:YSGG laser. The only two groups when compared that did not show statistical significance were the Er,Cr:YSGG laser group and the ultrasonic instrumentation group (p=0.374) (Table 1 and Fig. 2b).
Cell attachment
When comparing the cell attachment following treatment in each of the three groups and also without treatment (control), there was a statistical significance between the groups (p< 0.0001) in terms of total cell count (Table 1 and Fig. 3a). The control and laser groups had significantly more attached cells when compared to the two conventional treatment groups (cavitron and scaler). While there was no significant difference between the control and the laser groups (p=0.903), SEM analysis revealed differences in the mode of fibroblast attachment. Fibroblasts demonstrated a more elongated spindle-cell morphology on the laser group compared to the more rounded shapes on all the other surfaces. The fibroblasts on the laser-treated surface appeared flattened with filopodia extension, suggesting focal adhesion kinase–dependent migration and cell growth (Fig. 3b).
Discussion
The Er,Cr:YSGG laser has been shown in an in vitro study to effectively ablate biofilm from titanium surfaces without causing measurable physical changes to the surface [18]. In contrast, another study shows that the Er,Cr:YSGG laser causes a decrease in surface roughness of zirconia with an increase of roughness in titanium [19]. The results of the present study indicate that using the Er,Cr:YSGG laser on zirconia surfaces did not cause noticeable surface changes to the discs and was able to effectively ablate bacteria. The disparities in the reported results could be due to the use of different laser settings. In this study, the settings used for the laser were the same settings recommended to treat peri-implantitis intraorally from the manufacturer (1.5 W, 30 Hz, 40%/50% air/water). This setting has also been used to treat peri-implantitis with successful outcomes in clinical studies [13, 14]. The decontamination effect of the Er,Cr:YSGG laser could be contributed to its wavelength being in the region of the major absorption peak for water; therefore, with the laser irradiation, water quickly expanded and evaporated, creating acoustic waves strong enough for abrupt disintegration of the bacterial cell wall [20]. A study by Gordon et al. has shown that Er,Cr:YSGG laser was able to achieve intratubular water expansion and collapse as deep as 1000 μm in depth [21].
Interestingly, gross inspections of zirconia surfaces revealed damages caused by use of ultrasonic and hand scalers; however, no statistical difference in surface roughness was found when examined by a profilometer. This could be explained by the technical nature of the instruments. The debridement with ultrasonic and hand scalers was performed in a similar fashion to clinical settings (20 strokes per sample) in direct contact with the surface; the strokes left behind marks visible on the surface. These marks were larger in diameter than the profilometer tip and the measurements were performed in multiple spots, some without the strokes; therefore, it was not surprising that the profilometer failed to reveal statistical significance among the groups.
One important factor for dental implants is the mucosal seal around abutments to prevent biofilm accumulation. This is dependent on fibroblast attachment and the material of the abutment. After exposure of biofilm to implant and abutment surfaces, it was seen that an inflammatory lesion forms in the connective tissue that surrounds the implant and abutment [22]. The results of a canine study showed that the material used for the abutment portion of implants affects the location and quality of the attachment of the peri-implant mucosa and implant itself [23]. Fibroblasts are collagen fiber–producing cells that are seen in the connective tissue of peri-implant tissues, and most are seen directly next to implant abutment surfaces [24]. They are important to the soft tissue seal around implants and have been the subject of in vitro studies on attachment, spreading, and proliferation of fibroblasts [25]. The characteristic of fibroblast morphology has also been studied in terms of attachment. Studies focused on morphology of fibroblasts that appeared more attached, elongated, and stretched out onto surfaces [26,27,28].
After treatment of peri-implant disease, it is important to ensure that soft tissue attachment is favorable to have an appropriate mucosal seal. The present study showed that the use of the Er,Cr:YSGG laser allowed more fibroblast attachment compared to the other treatment modalities. Furthermore, the cells appeared more spindle in shape and adherent on the surfaces treated with the laser. Such fibroblast morphology favors soft tissue attachment to zirconia and resembled what was observed on Laser-lok titanium surface morphologically which was shown to induce a direct connective tissue attachment in a human histological study [29,30,31]. To the best of the author’s knowledge, our study is the first to evaluate fibroblast morphology after treatment of zirconia surfaces with a dental laser. We speculate that such result could be due to rise in surface energy and hydrophilicity after application of the laser and could be subjects of future studies.
Conclusion
Although gross examination of the discs shows clear surface changes when using ultrasonic instrumentation and hand scalers compared to the Er,Cr:YSGG laser group and control group, no difference in surface microroughness was seen. The Er,Cr:YSGG laser was able to effectively ablate bacteria from zirconia discs and was more effective than hand instrumentation. Fibroblast attachment on the surfaces of the zirconia discs shows more adherence when treated with Er,Cr:YSGG laser.
References
Branemark PI, Hansson BO, Adell R, Breine U, Lindstrom J, Hallen O, Ohman A (1977) Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand J Plast Reconstr Surg Suppl 16:1–132
Berglundh T, Armitage G, Araujo MG, Avila-Ortiz G, Blanco J, Camargo PM, Chen S, Cochran D, Derks J, Figuero E, Hammerle CHF, Heitz-Mayfield LJA, Huynh-Ba G, Iacono V, Koo KT, Lambert F, McCauley L, Quirynen M, Renvert S, Salvi GE, Schwarz F, Tarnow D, Tomasi C, Wang HL, Zitzmann N (2018) Peri-implant diseases and conditions: consensus report of workgroup 4 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Periodontol 89(Suppl 1):S313–S318
Lindhe J, Meyle J, D.o.E.W.o.P. Group (2008) Peri-implant diseases: consensus report of the Sixth European Workshop on Periodontology. J Clin Periodontol 35(8 Suppl):282–285
Khoshkam V, Suarez-Lopez Del Amo F, Monje A, Lin GH, Chan HL, Wang HL (2016) Long-term radiographic and clinical outcomes of regenerative approach for treating peri-implantitis: a systematic review and meta-analysis. Int J Oral Maxillofac Implants 31(6):1303–1310
Andersson B, Glauser R, Maglione M, Taylor A (2003) Ceramic implant abutments for short-span FPDs: a prospective 5-year multicenter study. Int J Prosthodont 16(6):640–646
Scarano A, Piattelli M, Caputi S, Favero GA, Piattelli A (2004) Bacterial adhesion on commercially pure titanium and zirconium oxide disks: an in vivo human study. J Periodontol 75(2):292–296
Hashim D, Cionca N, Courvoisier DS, Mombelli A (2016) A systematic review of the clinical survival of zirconia implants. Clin Oral Investig 20(7):1403–1417
Hollander J, Lorenz J, Stubinger S, Holscher W, Heidemann D, Ghanaati S, Sader R (2016) Zirconia dental implants: investigation of clinical parameters, patient satisfaction, and microbial contamination. Int J Oral Maxillofac Implants 31(4):855–864
Aoki A, Sasaki KM, Watanabe H, Ishikawa I (2004) Lasers in nonsurgical periodontal therapy. Periodontol 2000(36):59–97
Ting CC, Fukuda M, Watanabe T, Aoki T, Sanaoka A, Noguchi T (2007) Effects of Er,Cr:YSGG laser irradiation on the root surface: morphologic analysis and efficiency of calculus removal. J Periodontol 78(11):2156–2164
Natto ZS, Aladmawy M, Levi PA Jr, Wang HL (2015) Comparison of the efficacy of different types of lasers for the treatment of peri-implantitis: a systematic review. Int J Oral Maxillofac Implants 30(2):338–345
Azzeh MM (2008) Er,Cr:YSGG laser-assisted surgical treatment of peri-implantitis with 1-year reentry and 18-month follow-up. J Periodontol 79(10):2000–2005
Al-Falaki R, Cronshaw M, Hughes FJ (2014) Treatment outcome following use of the erbium, chromium:yttrium, scandium, gallium, garnet laser in the non-surgical management of peri-implantitis: a case series. Br Dent J 217(8):453–457
Nevins M, Benfenati SP, Galletti P, Zuchi A, Sava C, Sava C, Trifan M, Piattelli A, Iezzi G, Chen CY, Kim DM, Rocchietta I (2020) Human histologic evaluations of the use of Er,Cr:YSGG laser to decontaminate an infected dental implant surface in preparation for implant reosseointegration. Int J Periodontics Restorative Dent 40(6):805–812
Ercan E, Arin T, Kara L, Candirli C, Uysal C (2014) Effects of Er,Cr:YSGG laser irradiation on the surface characteristics of titanium discs: an in vitro study. Lasers Med Sci 29(3):875–880
Chegeni E, Espana-Tost A, Figueiredo R, Valmaseda-Castellon E, Arnabat-Dominguez J (2020) Effect of an Er,Cr:YSGG laser on the surface of implants: a descriptive comparative study of 3 different tips and pulse energies. Dent J (Basel) 8(4)
Park SH, Kim OJ, Chung HJ, Kim OS (2020) Effect of a Er,Cr:YSGG laser and a Er:YAG laser treatment on oral biofilm-contaminated titanium. J Appl Oral Sci 28:e20200528
Strever JM, Lee J, Ealick W, Peacock M, Shelby D, Susin C, Mettenberg D, El-Awady A, Rueggeberg F, Cutler CW (2017) Erbium, chromium:yttrium-scandium-gallium-garnet laser effectively ablates single-species biofilms on titanium disks without detectable surface damage. J Periodontol 88(5):484–492
Miranda PV, Rodrigues JA, Blay A, Shibli JA, Cassoni A (2015) Surface alterations of zirconia and titanium substrates after Er,Cr:YSGG irradiation. Lasers Med Sci 30(1):43–48
Turkun M, Turkun LS, Celik EU, Ates M (2006) Bactericidal effect of Er,Cr:YSGG laser on Streptococcus mutans. Dent Mater J 25(1):81–86
Gordon W, Atabakhsh VA, Meza F, Doms A, Nissan R, Rizoiu I, Stevens RH (2007) The antimicrobial efficacy of the erbium, chromium:yttrium-scandium-gallium-garnet laser with radial emitting tips on root canal dentin walls infected with Enterococcus faecalis. J Am Dent Assoc 138(7):992–1002
Zitzmann NU, Abrahamsson I, Berglundh T, Lindhe J (2002) Soft tissue reactions to plaque formation at implant abutments with different surface topography. An experimental study in dogs. J Clin Periodontol 29(5):456–461
Abrahamsson I, Berglundh T, Glantz PO, Lindhe J (1998) The mucosal attachment at different abutments. An experimental study in dogs. J Clin Periodontol 25(9):721–727
Buser D, Weber HP, Donath K, Fiorellini JP, Paquette DW, Williams RC (1992) Soft tissue reactions to non-submerged unloaded titanium implants in beagle dogs. J Periodontol 63(3):225–235
Mustafa K, Wennerberg A, Arvidson K, Messelt EB, Haag P, Karlsson S (2008) Influence of modifying and veneering the surface of ceramic abutments on cellular attachment and proliferation. Clin Oral Implants Res 19(11):1178–1187
Cho YD, Shin JC, Yoon HI, Ku Y, Ryoo HM, Kim DJ, Kim DG, Han JS (2015) Characterization of human gingival fibroblasts on zirconia surfaces containing niobium oxide. Materials (Basel) 8(9):6018–6028
Fischer NG, Wong J, Baruth A, Cerutis DR (2017) Effect of clinically relevant CAD/CAM zirconia polishing on gingival fibroblast proliferation and focal adhesions. Materials (Basel) 10(12)
Zheng M, Yang Y, Liu XQ, Liu MY, Zhang XF, Wang X, Li HP, Tan JG (2015) Enhanced biological behavior of in vitro human gingival fibroblasts on cold plasma-treated zirconia. PLoS One 10(10):e0140278
Esfahanizadeh N, Motalebi S, Daneshparvar N, Akhoundi N, Bonakdar S (2016) Morphology, proliferation, and gene expression of gingival fibroblasts on Laser-Lok, titanium, and zirconia surfaces. Lasers Med Sci 31(5):863–873
Nevins M, Kim DM, Jun SH, Guze K, Schupbach P, Nevins ML (2010) Histologic evidence of a connective tissue attachment to laser microgrooved abutments: a canine study. Int J Periodontics Restorative Dent 30(3):245–255
Nevins M, Nevins ML, Camelo M, Boyesen JL, Kim DM (2008) Human histologic evidence of a connective tissue attachment to a dental implant. Int J Periodontics Restorative Dent 28(2):111–121
Acknowledgements
The study was part of the primary author’s (Charles Pham, HSDM) research thesis submitted in partial fulfillment of the requirements for the MMSc degree. Authors report no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
One sentence summary: Using the Er,Cr:YSGG laser for treatment of peri-implant disease does not cause gross surface damage, can effectively ablate bacteria, and allows for fibroblast adherence.
Rights and permissions
About this article
Cite this article
Pham, C.M., Chen, CY. & Kim, D.M. The effects of using erbium, chromium-doped:yttrium-scandium-gallium-garnet laser on the surface modification, bacterial decontamination, and cell adhesion on zirconia discs: an in vitro study. Lasers Med Sci 36, 1701–1708 (2021). https://doi.org/10.1007/s10103-021-03313-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-021-03313-1