Abstract
The aim of this study was to evaluate the effects of photobiomodulation therapy (PBM) and ozone applications on patients’ quality of life after gingivectomy and gingivoplasty. In this study, 36 patients with chronic inflammatory gingival enlargement underwent gingivectomy and gingivoplasty. The groups were randomly divided into control (n = 12), PBM (n = 12) and ozone (n = 12) groups. GaAlAs diode laser 810 nm wavelength at a non-contact and continuous mode with a power of 0.3 W and a density of 4 J/cm2 used for PBM for 1 min. Ozone was applied for 1 min for every 5 mm2 in contact mode at power level 9 using probe number 3. PBM and ozone applications were performed immediately after the operation, on the 3rd and 7th days. Pain assessment was performed at 3rd, 7th, 14th and 28th days after gingivectomy and gingivoplasty by using visual analogue scale (VAS). Oral Health Impact Profile (OHIP-14) records were obtained from the patients before gingivectomy and gingivoplasty and postoperative 7th and 14th days. OHIP-14 questions were also evaluated individually. VAS pain levels of the control group measured on the 3rd day were higher than the PBM group and on the 7th day were found to be significantly higher than both groups (p < 0.05). The total OHIP-14 score of the control group on the 7th postoperative day was found to be higher than the PBM group (p < 0.05). The mean score obtained from the third question of OHIP-14 at 7th and 14th day of the PBM group was found to be lower than the control and ozone groups (p < 0.05). The PBM and ozone applications after gingivectomy and gingivoplasty reduce the pain levels of patients and have a positive effect on patients’ quality of life.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gingival enlargement is associated with many factors including inflammation, drug use, systemic diseases, and neoplastic conditions and represents an increase in the volume of the gingiva [1]. It is most commonly associated with interdental papillae and can be either generalized or localized. Bacterial plaque-induced chronic inflammation of gingival tissues has been mentioned as the most common cause of gingival enlargement or its exacerbation [2]. Periodontal pocket elimination is made through gingivectomy, and following this procedure, visibility and accessibility are provided for complete removal of calculus and complete correction of the root surface. Gingivoplasty is the reshaping of the gingiva to create physiological contours to the gingiva in the absence of periodontal pockets [3]. The wound site after gingivectomy and gingivoplasty operations is healed by secondary intention [4].
Ozone therapy is a preferred method for wound healing since it is effective on wounds that occur during periodontal surgical operations, prevents complications such as post-surgical infection, and contributes to proper tissue healing. Ozone application increases the perfusion of blood and contributes to wound healing by repairing restorative mechanisms that provide tissue regeneration and improve postoperative quality of life [5, 6]. The photobiomodulation therapy (PBM) laser class referred to as soft lasers includes a semiconductor diode laser. Unlike high-power rigid surgical laser, PBM diodes are compact and cost-effective devices with very high optical and electrical efficiency. Also, PBM lasers do not have a photothermal effect and are used for therapeutic purposes. Based on the biostimulation effect of laser beam on biological soft tissues, the therapy applied by using these lasers is called PBM therapy [7].
The visual analogue scale (VAS) is a simple, reliable and quickly applied method for measuring pain severity in the clinical environment [8, 9]. Oral health-related quality of life (OHRQoL), which was developed based on the World Health Organization’s structure-function-competence-participation model, evaluates the positive and negative effects of oral health on general health of patients [10, 11]. The Oral Health Impact Profile (OHIP) scale is commonly used for this purpose [12]. The OHIP-14 is the simplified version of the OHIP-49, which estimates the people’s attitude of the social impact of disorders influencing the oral cavity, on a question basis [13].
This study aimed to assess the effects of PBM and ozone applications after gingivectomy and gingivoplasty on quality of life and postoperative pain in patients with chronic inflammatory gingival enlargement.
Methods
Study population
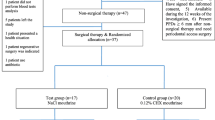
Systemically healthy patients aged 14–27 years with chronic inflammatory gingival enlargement were included in the study. Phase I periodontal treatment was applied to all patients. The patients were called for a follow-up visit 2 weeks later and 36 patients who achieved adequate oral hygiene were scheduled for surgery. All patients underwent gingivectomy and gingivoplasty. Patients were informed in detail about phase I periodontal treatment, gingivectomy and gingivoplasty operation, ozone and PBM applications. This study was carried out in accordance with the Declaration of Helsinki and was approved by the Malatya Clinical Research Ethics Committee (protocol no: 2018/113). Patients willing to participate in this study were asked to sign the informed consent form.
The study groups were randomized by computer-generated block randomization as follows:
-
1.
Control group (n = 12): Patients undergoing only gingivectomy and gingivoplasty
-
2.
Ozone group (n = 12): Patients receiving ozone application following gingivectomy and gingivoplasty
-
3.
Photobiomodulation therapy (PBM) group (n = 12): Patients receiving PBM application following gingivectomy and gingivoplasty (Fig. 1).
Study inclusion criteria were as follows: (i) being systemically healthy, (ii) presence of gingival enlargement involving the mandibular or maxillary anterior region that symmetrically affects at least six teeth, (iii) no attachment and bone loss and (iv) patients with sufficient oral hygiene.
Patients who had a history of periodontal treatment in the last 6 months, smokers and alcohol users, those who used drugs that may cause gingival enlargement in the last 6 months, pregnant women or women in the lactation period, and patients who did not attend controls at designated times were excluded from the study.
Gingivectomy and gingivoplasty operation
Infiltrative anesthesia (Maxicaine Fort, Vem, Turkey, articaine hydrochloride 80 mg/2 mL + epinephrine bitartrate 0.02 mg/2 mL) was applied and the incision lines were determined and an external bevel incision was made. The remaining gingival fragments were removed using periodontal curette and microsurgical scissors. Furthermore, it was aimed to correct gingival topography which was asymmetrical and had no esthetic appearance (Fig. 2). Following the completion of the operation, a periodontal dressing (COE-PAK, Alsip, IL, USA) was placed to the operation site. It was removed at 3rd day, and the wound areas of the patients in all groups were allowed to heal spontaneously in the remaining days. In this single-blind study, gingivectomy and gingivoplasty surgeries, PBM and ozone applications were performed by the same surgeon.
Photobiomodulation therapy application
GaAlAs diode laser (CHEESE™, GIGAA Laser, Wuhan Gigaa Optronics Technology Co., Ltd., China) which had been previously calibrated by the manufacturer was used in the PBM test group. Following the manufacturer’s instructions, the laser beam was directed perpendicularly toward the tissue in the noncontact mode and a continuous mode with a power of 0.3 W and a density of 4 J/cm2 for 1 min (Fig. 3b). PBM and treatment parameters were reported according to the recommendation proposed by Jenkins and Carroll in Tables 1, 2 and 3 [14]. A total of three sessions were performed: immediately after the operation, on the 3rd and 7th days.
Ozone application
Ozone DTA generator (Ozone DTA, Apoza Enterprise Co., New Taipei, Taiwan) which had been previously calibrated by the manufacturer was used in the ozone group. Ozone was applied for 1 min for every 5 mm2 in contact mode at power level 9 using probe number 3 according to the manufacturer’s instructions (Fig. 3d). Ozone device information and treatment parameters are reported in Table 4. A total of three sessions were performed: immediately after the operation, on the 3rd and 7th days.
Postoperative pain
VAS was used for the assessment of pain severity and relief due to the most commonly used method [8, 15]. VAS scores were obtained on the 3rd, 7th, 14th and 28th day without any intervention to the patient. The patients were prescribed paracetamol-containing analgesics (Parol 500 mg, Atabay, Istanbul, Turkey) for pain relief and they were told to use only when necessary (for minimizing the effect of analgesics to VAS scores). Total amount of painkillers was also recorded. It was suggested to protect the wound area with periodontal dressing from trauma, not to consume very hot foods and to eat soft foods.
Postoperative quality of life
The postoperative quality of life was evaluated by OHIP-14 scale separately in all categories of physical pain, functional limitation, psychological disability, social disability, psychological discomfort, physical disability and handicap [16]. The questionnaire was completed by the patients preoperatively and on the 7th and 14th days and summing the scores obtained from all these categories [17].
Evaluation of wound healing
Wound healing was evaluated according to the wound surface epithelialization. A 3% hydrogen peroxide (H2O2) was instilled onto the surface of the operation site through an injector to evaluate the postoperative epithelialization of the wound surface. After the decomposition of H2O2 to water and oxygen through the catalase enzyme released by blood cells in the wound area, epithelialization was evaluated as incomplete if foaming was observed with the formation of oxygen and it was evaluated as completed if there is no foaming. This H2O2 test was performed on the 3rd, 7th, 14th and 28th postoperative days (Fig. 4).
Evaluation of surface epithelialization by H2O2 test. a Clinical view before operation. b H2O2 solution drawn into the injector. c Observation of foaming after H2O2 application on the 3rd day after the gingivectomy and gingivoplasty surgery. d Foaming test positive on the 7th day. e Foaming test negative on the 14th day. f Complete wound healing on 28th day, foaming negative
Statistical analysis
IBM SPSS Statistics 22 (SPSS IBM, Turkey) program was used for statistical analysis. Descriptive data were expressed as mean, standard deviation and frequency. Kruskal-Wallis test was used for the intergroup comparison of quantitative data that was not normally distributed. The Wilcoxon signed rank test was used for intra-group comparisons of not normally distributed parameters. Spearman’s rank correlation coefficient analysis was used to investigate the relationship between the parameters that were not normally distributed. A p value of < 0.05 was considered statistically significant.
Results
The VAS level of the control group was higher than the PBM group on 3rd day and higher than both the ozone and PBM groups on 7th day (p < 0.05). The VAS level of the ozone group was higher than PBM group on 3rd and 7th days (p < 0.05). There was no difference between the groups on the 14th and 28th days (p > 0.05). Intragroup evaluation of the control, ozone and PBM groups revealed a significant decrease measured on 7th, 14th and 28th days compared with 3rd day outcomes (p < 0.05) (Table 5).
The total OHIP-14 score of the control group on the 7th day was higher than the PBM group (p < 0.05) (Fig. 5). No difference was observed between the groups in terms of preoperative and 14th day total OHIP-14 score (p > 0.05) (Fig. 6). Intragroup evaluation of the control, ozone and PBM groups revealed an increase on the 7th and 14th days (p = 0.002). The difference between the total scores measured on the 7th and 14th day was statistically significant (p = 0.002) (Table 6). In the intergroup evaluation, no difference was observed in terms of the mean scores obtained from the questions in OHIP-14 test at T0, T1 and T2 except for the third question (p > 0.05) (Figs. 5, 6 and 7). The mean score obtained from the third question of OHIP-14 at T1 and T2 of the PBM group was lower than the control and ozone groups (p < 0.05). There was no significant difference between control and ozone groups in terms of OHIP-14 third question at T1 and T2 times (p > 0.05).
Foaming was observed in all patients in the control, ozone and PBM groups in the H2O2 test performed on the 3rd and 7th days, meaning that epithelialization was completed in none of the patients. In the H2O2 test performed on 14th day, epithelialization was completed in three patients in the control group, six patients in the ozone group and eight patients in the PBM group; however, there was no statistically significant difference between the groups (p > 0.05). On the other hand, epithelialization was seen to be completed in all patients at 28th day (Table 7).
Analgesic usage of control group was higher than ozone and PBM groups (p < 0.05). There was a positive correlation between analgesic usage and VAS at 80.6%, 73.5% and 37.9%, respectively, on the 3rd, 7th and 14th days (p < 0.05). A positive correlation was found between analgesic usage and preoperative total OHIP-14 score at the level of 43.9%, 70% and 47.1%, respectively, on the 3rd, 7th and 14th days (p = 0.004). Also, significant positive correlation was found between the 3rd and 7th day VAS levels and preoperative and 7th day total OHIP-14 scores at 41.5% and 81.3%, respectively (p < 0.05).
Discussion
In the therapy of gingival enlargements, phase I periodontal treatment aiming at scaling&root planning and providing oral hygiene is applied to prevent the progression of the disease and relieve the inflammation. Phase I periodontal treatment can be performed using mechanical instruments, ultrasonic instruments and laser ablation methods. Surgical treatment is required if gingival enlargements still cause plaque accumulation despite phase I periodontal treatment and cannot be removed through the patient’s oral hygiene motivation [18].
In a clinical study by Sobouti et al. [19], aesthetic gingivectomy was performed in the anterior region using diode laser (diode Epic, BioLase, USA, 940 nm, 30s/per tooth, 400-μm fiber, 0.9 W power) and surgical scalpel and postoperative hemorrhage and pain scores were reported to be significantly lower in patients who was treated with 940 nm diode laser gingivectomy than in the control group. Since we aimed to evaluate the effect of postoperative PBM and ozone applications on the quality of life of the patients, gingivectomy and gingivoplasty operations were performed using a surgical scalpel.
Wound healing is a complex and dynamic process involving coordinated sequence of events including the onset of an acute inflammatory response to the first injury, coagulation&bleeding, regeneration and proliferation of parenchyma cells and connective tissues [20]. Wound healing aims to regenerate tissue integrity, to provide hemostasis and perfusion, to provide oxygenation and nutrition of tissue and to regain patient comfort functionally and aesthetically [21]. This study aimed to assess the effects of PBM and ozone applications on postoperative pain and quality of life of patients during the wound healing period after gingivectomy and gingivoplasty. As fibroblasts start to play an active role in the wound site on the 3rd day of the wound healing process, PBM and ozone applications were performed immediately after the gingivectomy and gingivoplasty and on the 3rd and 7th days in accordance with the manufacturer’s recommendations.
The stimulatory effects of PBM therapy at the cellular level are based on faster healing of tissue as a result of the increased oxygen uptake thanks to the increased blood flow in the damaged area and the formation of new capillaries. It has been reported to have many advantages such as (i) increasing cell respiration and adenosine triphosphate (ATP) synthesis, (ii) increasing in venous and lymphatic flow, (iii) ensuring collagen synthesis, (iv) having anti-inflammatory and analgesic effect, (v) stimulating wound healing, (vi) providing immune system modulation, (vii) increasing periodontal tissue attachment, (viii) increasing bone regeneration and (ix) reducing the inflammation in periodontal pockets [22, 23]. PBM application has been reported to play a role in reducing pain associated with inflammation by lowering prostaglandin E2, tumor necrosis factor-alpha and interleukin-1 beta levels [24]. Considering VAS pain results obtained in this study, pain scores on the third postoperative day were lower in the PBM group than control. On the seventh postoperative day, pain scores were significantly lower in PBM and ozone groups than control and PBM group was observed to have statistically lower pain scores than the ozone group. We preferred to use the VAS as it is easy to apply and explain and that requires a minimum time to reach the result and it is advantageous in terms of providing ease of comparison with similar studies in the literature. Furthermore, control group was found to use a statistically higher number of analgesics than the test groups. These results show the positive effect of PBM and ozone applications on pain response after conventional scalpel gingivectomy. In a clinical study by Kohale et al. [25] which is similar to our study, lower pain scores were reported in the PBM group after gingivectomy. A diode laser (InGaAsP, 940 nm, 4 J/cm2, 40 s/per tooth, 100 mW) was randomly applied to one side of the surgical area on the 1st, 3rd and 7th day postoperatively and PBM provided a better wound healing after gingivectomy. The results of our study are compatible with the results of their study. Amorim et al. investigated gingival healing after gingivectomy and adjunctive use of PBM therapy at bilateral maxillary and mandibular premolar teeth. PBM was performed with a diode laser (model IR 500; Laser Beam, 685 nm, 50 mW, continuous wave, beam diameter of 2 mm, contact mode, 80 s, 4 J/cm2) at immediately after surgery, 24 h, 3 and 7 days post-surgery and wound healing was evaluated at days 3, 7, 14, 21, 28 and 35. This study showed that, as similar results in our study, there was a significant improvement in healing for the laser group after gingivectomy [26]. Similar to these studies, Ozcelik et al. applied a 588-nm diode laser (Ulocks, VSMA Lab, 120 mW, 4 J/cm2, continuous wave mode for 5 min) for 7 days and showed that laser application may enhance epithelialization and improve wound healing after gingivectomy and gingivoplasty operations [27]. Another similar study investigated the effects of PBM therapy on wound healing after gingivectomy by Landry index, and although a better surface epithelialization was observed on the 14th day, there was not any difference between groups on the 3rd and 7th postoperative days [28]. We evaluated the wound healing by H2O2 test and gained similar results with this study. Although there was not any difference between groups on 3rd and 7th days, epithelialization was completed in three patients in the control group, six patients in the ozone group and eight patients in the PBM group on 14th day. Contradictory to these studies, Masse et al. [29] reported that PBM therapy applied after the mucogingival surgical operation was not effective in reducing the postoperative pain of the patient. They used soft laser (As-Ga and He-Ne) in their study and evaluated the postoperative pain by a different scale, modified McGill pain scale. This scale, which consists of 20 main parts with 6 different pain levels, is more complex and can be difficult to understand by patients than VAS scale and this scale and soft laser type may be an explanation for the possible contradictory results. We believe that these different findings in the literature may be due to many reasons such as differences in the laser device selected, wavelengths, application times and the structure of treated tissues.
OHRQoL contains significant information in terms of determining the treatment method to be applied and monitoring the patient’s condition. It is preferred as a comprehensive scale that includes subjective data in the measurement of oral health [12]. This 49-item scale has been shown to be useful in clinical trials. Since OHIP is a method assessing the problems experienced by patients, high scores indicate patients with oral health problems [30]. The original version of OHIP consists of 49 items, resulting in significant time loss and difficulties for patients. Therefore, a more easily understandable OHIP consisting of 14 items, which can be answered in a shorter time, have been developed and used in clinical trials [17]. In our study, the OHIP-14 scale was applied to all patients three times: before the operation, at 7th and 14th days. The scores of the control group on the seventh day were statistically higher than the PBM group. These results indicate that PBM application after scalpel gingivectomy improves patient comfort. The OHIP-14 scores of controls were found to be higher than the PBM and ozone group at all times. The results of our study show that PBM and ozone application have a beneficial effect on the quality of life of the patient.
This is the first study in the literature that evaluates the 14 questions of the OHIP-14 scale separately between the groups and within the groups in patients who underwent with PBM and ozone after gingivectomy. We further performed correlation analyses for the evaluated parameters. Statistically low scores were found in the control group compared to PBM and ozone groups in terms of the mean scores of OHIP-14 question 3 on the seventh and 14th postoperative days. These results support the analgesic effect of postoperative PBM application.
Ozone has been reported to increase the immune system and has an analgesic effect as well as antihypoxic and antimicrobial properties. Ozone is thought to have a salutary effect on wound healing process because of these properties [31]. In a study by Tasdemir et al. [32], the effect of ozone application (Ozonytron, Bionix, CA Probe) on the quality of life of the patients in the early recovery period after free gingival graft application was evaluated with OHIP-14 test and VAS. The first (at operation) and second (at 1st day) ozone applications were at 75% power for 30 s (75 μg/mL), and the third (at 3rd day) was at 30% power for 30 s (30 μg/mL), based on manufacturer’s instructions. They performed OHIP-14 test preoperatively and on the postoperative sixth and 13th days and found that the scores of the control group were higher than the ozone group on the sixth postoperative day. There was not any difference between the groups in terms of scores obtained preoperatively and on the 13th postoperative day. Although significant improvement was mentioned in the quality of life after the sixth day, it was reported to be at a low level for all groups on the 13th postoperative day compared to the preoperative period. In the same study, ozone group was reported to have significantly lower VAS scores in the postoperative first week compared to the control group. Furthermore, analgesic amount was higher in the control group. The results of our study were similar to this study in terms of OHIP, VAS and analgesic amount. Ozcelik et al. [33] reported that the quality of life values of patients treated with different periodontal treatment methods tend to return to baseline values after the first postoperative week. However, different periodontal surgeries may affect wound healing and patient’s quality of life in different ways. In our study, although OHIP-14 scores on the 14th day were lower in all groups than the OHIP-14 scores on the seventh day, these scores were at a slightly higher level compared to the preoperative period.
Kazancioglu et al. [34] investigated the effect of ozone and PBM therapies applied after the extraction of the impacted wisdom tooth on the patient’s quality of life using VAS and OHIP-14 scale. They used a diode laser (GaAlAs, Fotona XD-2, Fotona, with a continuous wavelength of 808 nm, 100 mW, 0.1 W, 120 s, 12 J-total, 4 J/cm2) and an ozone generator (Biozonix GMbH, intensity of 80% for 10 s, with a high frequency 7.5 cm deep tissue probe-Omega probe) in the management of pain, swelling and trismus and applied extraorally at the insertion point of the masseter muscle. They reported that the quality of life was better in the laser and ozone groups than the control group and the rate of pain reliever use was significantly higher in the control group. This study showed that PBM and ozone applications are useful for the reduction of postoperative pain and these therapies increase the quality of life after third-molar surgery. Despite the application area was different in this study, it was shown that ozone and PBM therapies have a positive effect on quality of life and our study is compatible with this study.
Small sample size and lack of histological evaluation of wound healing can be considered as limitations of the study. Within the limitations of the present study, PBM and ozone applications after gingivectomy improve the quality of life of the patients. There is a need for clinical studies involving more patients in which PBM and ozone applications are used in different periodontal surgical procedures and assess from the histological point of view.
References
Fay AA, Satheesh K, Gapski R (2005) Felodipine-influenced gingival enlargement in an uncontrolled type 2 diabetic patient. J Periodontol 76:1217–1222
Seymour RA (2006) Effects of medications on the periodontal tissues in health and disease. Periodontol 2000(40):120–129
Goldman HM (1950) The development of physiologic gingival contours by gingivoplasty. Oral Surg Oral Med Oral Pathol 3:879–888
Witte MB, Barbul A (1997) General principles of wound healing. Surg Clin North Am 77:509–528
Akgul S, Kiziltoprak M, Uslu MO (2018) Ozone therapy in periodontology. Sci J Research & Rev 1:1–3
Gupta G, Mansi B (2012) Ozone therapy in periodontics. J Med Life 5:59–67
Walsh LJ (1997) The current status of low level laser therapy in dentistry. Part 1. Soft tissue applications. Aust Dent J 42:247–254
Carlsson AM (1983) Assessment of chronic pain. I. Aspects of the reliability and validity of the visual analogue scale. Pain 16:87–101
Crichton N (2001) Information point: visual analogue scale (VAS). J Clin Nurs 10:697–706
WHOQOL group (1993) Study protocol for the World Health Organization project to develop a quality of life assessment instrument (WHOQOL). Qual Life Res 2:153–159
John MT, Hujoel P, Miglioretti DL, LeResche L, Koepsell TD, Micheelis W (2004) Dimensions of oral-health-related quality of life. J Dent Res 83:956–960
Basol ME, Karaagaclioglu L, Yilmaz B (2014) Türkçe ağız sağlığı etki ölçeğinin geliştirilmesi-OHIP-14-TR. Turkiye Klinikleri J Dental Sci 20:85–92
Slade GD, Spencer AJ (1994) Development and evaluation of the oral health impact profile. Community Dent Health 11:3–11
Jenkins PA, Carroll JD (2011) How to report low-level laser therapy (LLLT)/photomedicine dose and beam parameters in clinical and laboratory studies. Photomed Laser Surg 29:785–787
Kelly AM (2001) The minimum clinically significant difference in visual analogue scale pain score does not differ with severity of pain. Emerg Med J 18:205–207
Locker D (1988) Measuring oral health:a conceptual framework. Community Dent Health 5:3–18
Slade GD (1997) Derivation and validation of a short-form oral health impact profile. Community Dent Oral Epidemiol 25:284–290
Taskan MM (2015) Laser-assisted gingivectomy techniques used in treatment of chronic inflammatory gingival enlargement: a review. Cumhuriyet Dent J 18:370–379
Sobouti F, Rakhshan V, Chiniforush N, Khatami M (2014) Effects of laser-assisted cosmetic smile lift gingivectomy on postoperative bleeding and pain in fixed orthodontic patients: a controlled clinical trial. Prog Orthod 15:66
Rivera AE, Spencer JM (2007) Clinical aspects of full-thickness wound healing. Clin Dermatol 25:39–48
Enoch S, Leaper DJ (2008) Basic science of wound healing. Surgery (Oxford) 26:31–37
Dogan GE, Demir T, Orbak R (2014) Periodontolojide düşük doz lazer uygulamaları. Clin Exp Health Sci 4:43–50
Tarhan K, Alkan BA (2015) Periodontal tedavide düşük doz lazer tedavisi uygulamaları. J Dent Fac Atatürk Uni 24:61–66
Bjordal JM, Johnson MI, Iversen V, Aimbire F, Lopes-Martins RA (2006) Photoradiation in acute pain: a systematic review of possible mechanisms of action and clinical effects in randomized placebo-controlled trials. Photomed Laser Surg 24:158–168
Kohale BR, Agrawal AA, Raut CP (2018) Effect of low-level laser therapy on wound healing and patients' response after scalpel gingivectomy: a randomized clinical split-mouth study. J Indian Soc Periodontol 22:419–426
Amorim JC, de Sousa GR, de Barros SL, Prates RA, Pinotti M, Ribeiro MS (2006) Clinical study of the gingiva healing after gingivectomy and low-level laser therapy. Photomed Laser Surg 24:588–594
Ozcelik O, Cenk Haytac M, Kunin A, Seydaoglu G (2008) Improved wound healing by low-level laser irradiation after gingivectomy operations: a controlled clinical pilot study. J Clin Periodontol 35:250–254
Lingamaneni S, Mandadi LR, Pathakota KR (2019) Assessment of healing following low-level laser irradiation after gingivectomy operations using a novel soft tissue healing index: a randomized, double-blind, split-mouth clinical pilot study. J Indian Soc Periodontol 23:53–57
Masse JF, Landry RG, Rochette C, Dufour L, Morency R, d'Aoust P (1993) Effectiveness of soft laser treatment in periodontal surgery. Int Dent J 43:121–127
Slade GD, Spencer AJ (1994) Social impact of oral conditions among older adults. Aust Dent J 39:358–364
Bocci V (1999) Biological and clinical effects of ozone. Has ozone therapy a future in medicine? Br J Biomed Sci 56:270–279
Tasdemir Z, Alkan BA, Albayrak H (2016) Effects of ozone therapy on the early healing period of deepithelialized gingival grafts: a randomized placebo-controlled clinical trial. J Periodontol 87:663–671
Ozcelik O, Haytac MC, Seydaoglu G (2007) Immediate post-operative effects of different periodontal treatment modalities on oral health-related quality of life: a randomized clinical trial. J Clin Periodontol 34:788–796
Kazancioglu HO, Ezirganli S, Demirtas N (2014) Comparison of the influence of ozone and laser therapies on pain, swelling, and trismus following impacted third-molar surgery. Lasers Med Sci 29:1313–1319
Acknowledgments
The authors thank statistician Hande Emir, SWOT Statistics, Istanbul, for the help in statistical analysis.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics statement/confirmation of patients’ permission
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional review board of Malatya Clinical Research Ethics Committee (Protocol No: 2018/113) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed and written consent was obtained from all participants individual included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Uslu, M.Ö., Akgül, S. Evaluation of the effects of photobiomodulation therapy and ozone applications after gingivectomy and gingivoplasty on postoperative pain and patients’ oral health-related quality of life. Lasers Med Sci 35, 1637–1647 (2020). https://doi.org/10.1007/s10103-020-03037-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-020-03037-8