Abstract
Objectives
The purpose of this study was to compare the anti-inflammatory efficacy of sodium chloride- and a 0.12% chlorhexidine mouth rinses in patients undergoing minimal invasive periodontal surgery.
Materials and methods
Forty-seven patients with a diagnosis of periodontitis and indication for access flap procedure were randomly selected. Group A: a sodium chloride (salt)water-based mouth rinse (test group) or group B: a 0.12% chlorhexidine mouth rinse (control group) administered after surgery. Gingival Index (GI) were evaluated in the whole mouth and in the surgical site at baseline (T1), a week later (T2), and 12 weeks (T3) after the treatment. Total MMP activity was measured in GCF using a commercial kit and plate reader. Medians of total MMP activity and GI were compared for time intervals T1 vs. T2, T1 vs. T3, and T2 vs T3 using Friedman tests and Wilcoxon signed rank tests, and were also compared between test and control using Mann-WhitneyU tests at each timepoint.
Results
The average GI values showed significant differences between baseline and T2 (p = 0.0005) and baseline and T3 (p = 0.003) in the test group.
Conclusion
The sodium chloride-mouth rinse use after periodontal surgery seems to have similar anti-inflammatory properties as CHX mouth rinse and can be used regularly postoperatively after periodontal surgical procedures.
Clinical relevance
The use of salt water mouthwash showed an anti-inflammatory effect similar to CHX 0.12% after minimal invasive periodontal surgery. Salt water mouthwash is accessible to the world population and can contribute on the healing process after periodontal surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Periodontal diseases are considered one of the most prevalent pathological conditions worldwide [1]. Its impact significantly affects the oral, systemic health, and quality of life of the individual, representing their treatment a high cost for the patients and their relatives [2,3,4,5,6]. Local antimicrobials in the form of rinsing have been used routinely by clinicians to control the supra- and subgingival biofilm, during or after periodontal, implant, or oral surgery [7,8,9,10].
Mouthrinse first appeared as a formal practice, around 2,700 BC, in Chinese medicine, for the treatment of gingival diseases. Also, they became popular among the upper classes in the Roman period as a complement to mechanical cleaning. In fact, the Roman writer and naturalist Plinio recommended the use of saltwater as the mouthwash [11].
In general, the ideal properties of mouth rinses should be fast and safe, capable of eliminating the viability of the biofilm in areas of difficult access, good taste, cheap and easy to use, and able to reach the place of onset of the disease (supragingival for gingivitis; subgingival for periodontitis) [12,13,14].
Chlorhexidine is the most studied antimicrobial globally and is the gold standard for the treatment of gingival inflammation and has been widely used clinically [7]. However, common side effects of CHX mouth rinse have been reported and include reversible dryness of mouth, yellow-brown discoloration of teeth and dorsum of the tongue, mild-to-moderate irritation of oral mucosa, alteration in taste sensation, cytotoxic effects on human gingival fibroblasts, and burning mouth condition [7, 15, 16].
Previous studies have reported that the use of saltwater as a mouth rinse has an anti-inflammatory, anti-plaque effect and can be used on wound healing and complications after dental extractions and in patients with oral mucositis who received radiotherapy or chemotherapy [17,18,19,20,21]. In addition, some benefits include security, cost-effectiveness, and easy access [17]. However, the use of saltwater mouth rinse has been used empirically by the clinician and the general population rather than on demonstrable scientific evidence [22], especially when it is referring to surgical periodontal therapy. It would be of great interest to identify a mouthwash that is accessible to the world population and that contributes to the prevention of highly prevalent oral diseases, such as periodontal diseases and tooth decay, contributing significantly to the oral health and quality of life of many individuals.
Although there is little scientific evidence to support the use of salt water as a mouthwash, there are some recommendations in its use. Alling et al. [23] prepared the saline rinse dissolving one level teaspoon of salt in a glass of warm water (300–350 ml). The saline produced a hypertonic solution that is believed to be bacteriostatic. It is widely known that salt has antibacterial properties and preserves food when it is applied in abundance because it absorbs water molecules [24,25,26].
Furthermore, one of the explanations for the antibacterial effect of salt in the oral cavity is that it produces a change in the pH of the oral cavity, which can inhibit biofilm formation.
The analysis of biomarkers in samples of gingival crevicular fluid (GCF), saliva and oral rinsing can provide, along with traditional clinical and complementary methods, additional information for health professionals regarding the presence of periodontal diseases, the need for treatment, or the efficacy of the medication. This easily collected sample has been used to study the levels of several molecules that are released during oral wound healing in humans [27, 28]. Matrix metalloproteinases (MMPs) are key proteases involved in destructive periodontal diseases and wound healing processes. MMP activity is tightly regulated through gene expression, proenzyme activation, and enzyme inhibition by endogenous inhibitors, such as tissue inhibitors of MMPs (TIMPs) [27]. Accordingly, endogenous total MMP activity might provide a broader vision of periodontal inflammation and wound healing.
To the best of our knowledge, no study has been published from independent researchers/research institutions that focused on comparative results of commercially available 0.12% CHX and a saltwater mouth rinse after periodontal access surgery. The present study aimed to investigate the anti-inflammatory effect of saltwater or 0.12% CHX on periodontal tissue healing after periodontal surgery. Besides, patient satisfaction and postoperative pain using both mouth rinses were evaluated.
Materials and methods
Study design
This was a randomized prospective blind study conducted in the Department of Periodontology, School of Dentistry Pontificia Universidad Católica Madre y Maestra, Santo Domingo, Dominican Republic. The study was conducted based on a study protocol in accordance with the Declaration of Helsinki (1975), as revised in 2013 and was reviewed and approved by the Institutional Review Boards, Bioethics Committee Faculty of Health Sciences Pontificia Universidad Católica Madre y Maestra (COBE-FACS-EST-CSTA-001-3-2014-2015).
Participants
Forty-seven patients (22 males and 25 females), aged between 30 and 68 years, with a diagnosis of periodontitis and an indication of an open flap debridement were included to the study. The investigation was based on the study protocol explained to the patients, and signed informed consent was obtained before enrollment. Patients were included if they (1) were individuals aged 18 years and 75 years; (2) had in general good health; (3) were non-smokers;(4) were available during the 12 weeks of the study; (5) presented periodontitis, defined as the presence of at least three interproximal non-adjacent sites with probing pocket depths (PPDs) of 4 mm or greater and radiographic evidence of alveolar bone loss; and (6) patients, who present PPD ≥ 6 mm after non-surgical therapy and need periodontal access surgery. Patients were excluded if they were (1) pregnant women and (2) taken antibiotics and/oranti-inflammatory drugs in the previous month; (3) patients with orthodontic bands or other orthodontic appliances; (4) with the presence of removable restorations; (5) with the presence of oral pathology; (6) five or more teeth with carious lesions; (7) patients, who have participated in another study 1 month before the start of this study; (8) presented allergic products to personal care; and (9) patients, who had a medical condition that contraindicated them from consuming food or drinking fluids for periods of 4 h. The surgeries were performed from January 2016 to August 2018. After informed consent was obtained, subjects completed the initial visit form and received an evaluation of their oral soft tissues. Also, a full-mouth periodontal examination and radiographic evaluation was performed. A periodontal diagnostic evaluation was performed using a North Carolina periodontal probe (Hu-Friedy- PCP UNC15, Chicago, IL, USA).
Randomization and surgical protocol
A non-surgical periodontal therapy was performed on all 47 patients participants, consisting of oral hygiene instructions, scaling, and root planing using hand instruments and ultrasonics. All participants were instructed to brush their teeth for 1 min, three times a day (morning, afternoon, and evening). Four to six weeks after completion of the non-surgical periodontal therapy, stable conditions, and minimal inflammation of the supracrestal soft tissue was observed. All patients demonstrated adequate plaque control with a full mouth plaque score (O’Leary) [29] ≤ 20 % prior to surgery.
After the initial therapy, the groups were divided into an experimental (test) or control group. Subjects were randomly assigned to treatment groups at the time of surgery, and an operator who performed the intervention were blinded to treatment assignment, which was successfully retained throughout the entire duration of the study. Postgraduate students from the Department of Periodontology participated in the surgical procedures following strict surgical protocol, always supervised by an experienced operator.
After local anesthesia was administered using 2% lidocaine with 1:100,000 epinephrine (DFL, Rio de Janeiro, RJ, Brazil), surgical therapy was performed. A sulcular incision was made with a #15 scalpel, allowing access to the bone crest utilizing a minimal invasive full-thickness flap [30]. Instrumentation was performed by automatic (ultrasonic) and manual root instrumentation. Caution was taken not to elevate beyond 2 mm of the alveolar bone crest. Primary closure, without flap tension, using nylon or vicryl 4.0 suture material was obtained in all cases with a simple, interrupted sutures.
Postoperative instructions
Immediately after surgery, the mouth rinses were distributed according to the previous randomization. Group A (test group) patients were asked to rinse their mouth, 30 min after brushing their teeth, twice per day with 15 ml of saline mouth rinse for 1 min and then to spit it out, and group B (control group) were requested to rinse their mouth with 15 ml of 0.12% CHX mouth rinse (Clorhexidina Lacer®) for a minute; all participants rinse in the morning and in the night, before going to bed. Patients were instructed not to eat or drink for 30 min after rinsing. The subjects were instructed to use only the treatment products during the study period and a soft-bristle brush for adults and regular toothpaste for home use. The treatment products were supplied by the researchers, and there were no restrictions regarding diet and habits during the course of the study. The saltwater mouth rinse was prepared using a sterile 8-ounce container of purified water and 7 g of salt. Participants received the prepared rinses and a measuring cup to use the required 15 ml. Patients were further motivated with respect to oral hygiene habits during the entire period of the study. Additionally, patients were advised to report to the investigators any discomfort, taste disturbance, sensitivity or burning sensation in the mouth that they experienced during postoperative mouthrinse use. After 1 week, the patients returned to remove the sutures, and a postoperative evaluation was performed.
Gingival crevicular fluid sampling
At the selected teeth, GCF samples were obtained from the middle site of each periodontal pocket in the subjects before the start of treatment and at 1 and 12 weeks after surgery. Before gingival GCF samples were obtained, the sites were isolated to avoid saliva by using cotton rolls and drying with the air syringe gently to avoid contamination. A supragingival plaque was removed from the surface using a sterile curette. A sterile paper point (#30, Maillefer, Ballaigues, Switzerland) was carefully inserted 2 mm into the sulcus for 30 s [31]. The collected sample of each periodontal pocket was placed in Eppendorf tubes before freezing at − 20 °C. All GCF samples were stored at − 20 °C until required for laboratory analyses. Sterile paper points contaminated with blood were discarded.
Primary and secondary outcome measures
The primary outcome of the study was the anti-inflammatory effect of saltwater after periodontal surgery. Gingival index (GI) [32] were registered at baseline, 1 week, and 3 months after surgery of the selected teeth. Secondary outcomes included the following: (a) Postoperative pain, (b) Mouthrinse satisfaction, (c) Tasting; and (d) MMP activity. A Visual Analogue Scale for postoperative pain, mouth rinse satisfaction, and tasting were obtained and analyzed. All measurements were performed by a single masked examiner (JC).
Analysis of MMP activity in the gingival crevicular fluid
The collected GCF was subsequently eluted in a constant ratio of 80 μL buffer per strip in TCL buffer containing 50 mM Tris-HCl pH 7.5, 0.2 M NaCl, 5 mM CaCl2, and 0.01% Triton X-100 with the addition of an EDTA-free protease inhibitor cocktail (Roche Diagnostics, Basel, Switzerland).
The total MMP activity levels were determined using a commercial MMP fluorometric activity assay kit (Abcam, USA ab112146 MMP Activity Assay Kit) following the manufacturer’s recommendations. The samples were loaded and mixed into 96-well plates using 5-FAM/QXL TM 520 fluorescence resonance energy transfer (FRET) peptide substrate in assay buffer. The fluorescence of 5-FAM was recovered and monitored at excitation/emission wavelengths (490/525 nm, respectively) at End-point on a microplate reader (Synergy HT; BioTek Instrument Inc., Winooski, VT, USA). Upon cleavage by endogenously active MMP, the total MMP activity was expressed as relative fluorescence units (RFU).
Statistical analysis
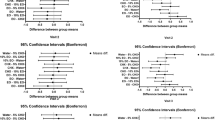
Means and standard deviations of age were calculated for the test and control groups and compared using an independent t test. The percentage of gender was compared between the two experimental groups using a Chi-square test. For repeated measures of ordinal total MMP activity and GI, median and interquartile range were calculated at baseline, 1 week, and 12 weeks for each group. Two series of comparisons were conducted for these repeated measures: (1)within-group comparisons. For each test and control group, the overall significance in timepoints was tested using Friedman tests. If the Friedman test is significant, Wilcoxon signed-rank tests were used to compare between two different time points (T1 vs. T2, T1 vs. T3, and T2 vs. T3) for each group. (2)between-group comparisons. Medians of measures at baseline, T2, and T3 were compared between test and control using Mann-WhitneyU tests. For postoperative pain, mouth rinse pain, satisfaction, and tasting, between-group comparisons were performed between test and control using Mann-WhitneyU tests. Due to the exploratory nature of this study and the small sample size, p values were not adjusted for multiple comparisons, and p value < 0.05 was considered as statistically significant. All statistical analyses were performed using SAS v9.4 (SAS Institute, Cary, NC).
Results
Of the 47 patients invited to participate, 10 were excluded for the following reasons: one was excluded due to decreased probing depth after non-surgical periodontal therapy; one patient did not perform blood tests analysis; in one patient regenerative surgery was indicated; one took antibiotics before surgery; one because of general systemic health reasons; and five missed follow-up appointments. The first 24 patients who were enrolled in the study (11 test and 13 control), completed the 3 samples of MMPs (Fig. 1). The participants in this clinical trial had mean ages of 50.47 (± 12.28) and 47.65 (± 10.71) in the test and the control group, respectively, and 41% (Table 1). Forty-one percent of participants were females in the test group and 60% in the control group. There are no significant differences between test and control groups for age and gender (Table 1).
Anti-inflammatory effectiveness
Medians and interquartile ranges of GI at each time point for each group are presented in Table 2. Overall, there are significant over time in the lower Gingival Index (p = 0.004) and the average Gingival Index (p = 0.003) in the test group. When compared to baseline, the lower Gingival Index of the test group has a significant reduction at T2 (p = 0.02) and T3 (p = 0.001). No significant differences were observed between T2 and T3, though (p = 0.31). Similar results were observed in the average Gingival Index of the test group that significant reductions were observed at T2 (p = 0.005) and T3 (p = 0.003). But no significant differences were found between T2 and T3 (p = 0.52). No significant differences were found when comparing the test and control group at each timepoint (all -values > 0.10).
The p value obtained on the test and control groups for postoperative pain values was 0.58, indicating no significant difference between them. The same was observed when considered the mouth rinse satisfaction; no statistically significant difference was observed between test and control groups (p = 1.00). For the mouth rinse tasting, the p-value of 0.12 indicates no significant difference between the test and control group (Table 3). In addition, none of the patients reported discomfort, taste disturbance, sensitivity, or burning sensation in the mouth with any of the mouthrinses.
Median of MMPs for test and control groups at each timepoint are illustrated in (Table 4). No significant differences were observed in either Test or Control group over time. There were no significant differences found between test and control at each timepoint, either.
Discussion
The present study compared the anti-inflammatory effects of saline mouth rinse with 0.12% CHX. Recently, a randomized controlled pilot study was conducted comparing the effects of two oral rinses: chlorhexidine 0.20% and seawater (Sea 4® Encias) for reducing plaque and gingivitis indices [33]. Both mouth rinses significantly reduced plaque accumulation and Gingival Index when compared to each other. However, in this pilot study, seawater mouth rinse was more effective against plaque regrowth than chlorhexidine.
Aravinth et al. [18] compared the effectiveness of saltwater rinse with chlorhexidine mouth rinse in reducing dental plaque and oral microbial count. The minimum inhibitory concentration of saltwater against S. mutans, L. acidophilus, A. actinomycetemcomitans, and P. gingivalis was determined by macrobroth dilution method. Saltwater was as effective as chlorhexidine in reducing dental plaque (p = 0.19) and A. actinomycetemcomitans (p = 0.35) count and while chlorhexidine was superior against S. mutans (p = 0.001), L. acidophilus (p = 0.001), and P. gingivalis (p = 0.001).
It should be noted that in the present study, the inflammatory response after 1 week of surgery was minimal for both groups. This could be due to the surgical design and flap management that involved interproximal tissue maintenance with minimal exposure to the alveolar bone. Also, the suture technique allowed optimal primary closure in all cases, supporting adequate wound stability for tissue formation and maturation. Apart from the access periodontal flap, no regenerative therapy was performed in any of the cases.
Chen et al. [34] evaluated the effectiveness of natural compounds containing mouth rinse (NCCM) as an adjunct to unsupervised oral hygiene in the management of dental plaque and gingivitis. The authors showed that of the 13 NCCMs tested, eight demonstrated positive results, and few reported any adverse effects or events. However, they conclude that evidence is still insufficient and further high-quality studies are required. For hundreds of years, saltwater mouth rinse has been recommended and used for various oral conditions, but as previously mentioned, most of these indications have not been scientifically proven [22]. Although, in recent years there is evidence in the literature of its use in different dental procedures [17,18,19,20,21,22, 33], the present study provides the first scientific evidence of the use of a saltwater mouth rinse after periodontal surgical treatment. Evaluation of patient outcome reveals that there were significant differences in the test and control groups for GI over time; whereas no significant differences were found when comparing the test and control groups, demonstrating that both chlorhexidine and saline water mouth rinses can improve the periodontal condition after periodontal surgery.
It is widely accepted that mouth rinses containing chlorhexidine in different concentrations have been shown to be effective in controlling inflammation and biofilm and has been used by clinics before, during, and after periodontal therapy [14, 15]. Chye et al. [35] conducted a systematic review to evaluate the effectiveness, side effects, and patient acceptance of different concentrations and formulations of chlorhexidine-based mouthwashes used after periodontal and implant surgery. The authors reported a positive relationship between the use of chlorhexidine and reduction of plaque and decrease of inflammation after periodontal and implant surgery. However, in the healing process, its effectiveness has generated controversy, since CHX has been associated with tissue necrosis, inflammatory reactions, and inhibition of regeneration [36, 37]. In a recent study, Coehlo et al. [16] investigated the cytotoxic effects of an enzymatic mouthwash and of chlorhexidine mouthwash on human gingival fibroblasts. The results showed that the cytotoxic effects of chlorhexidine on fibroblasts were identified at lower concentrations than those used in clinical practice. Therefore, they concluded that the use of chlorhexidine as an antiseptic in surgical and postoperative situations should be limited. In contrast, Huynh et al. [38] investigated the effect of short-term rinsing with a low concentration of NaCl on human gingival fibroblast (hGFs) in an artificial wound in vitro. They concluded that short-term rinsing with NaCl promoted hGFs migration and increased the expression of extracellular matrix as well as cytoskeletal proteins.
In previous publications [39,40,41], CHX has been associated with lower nitrate activity of oral bacteria and increased systolic blood pressure in healthy individuals. Bescos et al. [42] investigated the effect of 7-day use of CHX mouthwash on the salivary microbiome and several saliva and plasma biomarkers in 36 healthy individuals. Saliva and blood samples were taken at the end of each treatment to analyze the abundance and diversity of oral bacteria and pH, lactate, glucose, nitrate, and nitrite concentrations. The results showed that lower saliva and plasma nitrite concentrations were found after using CHX, followed by a trend of increased systolic blood pressure, demonstrating that mouthwash containing CHX is associated with a major shift in the salivary microbiome, leading to more acidic conditions and lower nitrite availability in healthy individuals.
Regarding the daily use regimen of the salt mouth rinse, many recommendations by clinicians and the general population have been given empirically. In the present study, both groups rinsed twice a day for 7 days, with no statistically significant difference in mouthrinse in terms of postoperative pain, satisfaction, and taste values. In this aspect, Osunde et al. [17] conducted a study to evaluate if the use of saline mouth rinse following dental extractions reduces postoperative complications. Group A (n = 40) were instructed to rinse the mouth six times daily with warm saline and group B (n = 40) twice daily; group C (n = 40) were not instructed to irrigate the mouth with warm saline and served as controls. They concluded that warm saline mouth rinse is beneficial in the prevention of alveolar osteitis after dental extractions in comparison with those who did not rinse. In addition, no significant difference was found in the efficacy of the twice-daily or six times daily warm saline mouth rinse regimen, ensuring better compliance with the treatment in the twice-daily saline mouth rinse regimen group. In a recent study, Hoover et al. [22] evaluated a new mouth rinse containing sea salt, xylitol, and lysozyme on biofilm formation and gingival health in a group of young adults. The control group, maintained standardized oral health practices for the duration of the experiment, and the test group rinsed with a tablespoon of the provided sea salt mouth rinse for 30 s once in the morning and at night. Clinical parameters were measured at baseline and after 30-day, the results showed no statistically significant differences in the overall reduction from baseline in the mean plaque and gingivitis scores.
In the current study, no statistically significant differences were found for total MMP activity at the follow-up period compared to the baseline for any of the study groups. A previous study confirm these findings regarding MMP activity and levels, proposing a more prolonged inflammatory response after a surgical procedure, which might involve in turn a lingering wound healing when compared to conservative periodontal treatment only [43]. Also, in our study, no significant difference was found for total MMP activity between test and control groups, revealing that none of the study mouth rinses had a perceivable impact on the overall proteolytic activity at the analyzed follow-up period.
Because this was a prospective study, the periodontal diagnosis was initially based on the 1999 classification of periodontal diseases [44], but with the 2017 Classification of Periodontal and Peri-Implant Diseases and Conditions, these patients would be diagnosed with periodontitis stages III–IV, grade A [1].
As this is the first study comparing a saltwater mouth rinse in inflammation after minimal invasive periodontal surgery, it is not possible to compare with the results of other studies. Therefore, further research is needed to determine the efficacy of saltwater on periodontal inflammation and biofilm control. Limitations of the present study also included that treatment was provided by different operators, although supervised and finalized by one experienced supervisor.
Conclusions
Within the limitation of the present study, it appears that the use of saline mouth rinse after minimal invasive periodontal flap surgery has similar clinical and anti-inflammatory properties as CHX mouth rinse and can be used regularly at earlier stages of wound healing.
References
Papapanou PN, Sanz M, Buduneli N, Dietrich T, Feres M, Fine DH, Flemmig TF, Garcia R, Giannobile WV, Graziani F, Greenwell H, Herrera D, Kao RT, Kebschull M, Kinane DF, Kirkwood KL, Kocher T, Kornman KS, Kumar PS, Loos BG, Machtei E, Meng H, Mombelli A, Needleman I, Offenbacher S, Seymour GJ, Teles R, Tonetti MS (2018) Periodontitis: consensus report of workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Clin Periodontol 45(Suppl 1):S162–S170
Carrizales-Sepúlveda EF, Ordaz-Farías A, Vera-Pineda R, Flores-Ramírez R (2018) Periodontal disease, systemic inflammation and the risk of cardiovascular disease. Heart Lung Circ 27:1327–1334. https://doi.org/10.1016/j.hlc.2018.05.102
Tonetti MS, Jepsen S, Jin L, Otomo-Corgel J (2017) Impact of the global burden of periodontal diseases on health, nutrition and wellbeing of mankind: a call for global action. J Clin Periodontol 44:456–462. https://doi.org/10.1111/jcpe.12732
Collins JR, Elías AR, Brache M, Veras K, Ogando G, Toro M, Rivas-Tumanyan S, Rajendra AB (2019) Association between gingival parameters and oral health-related quality of life in Caribbean adults: a population-based cross-sectional study. BMC Oral Health 19:234. https://doi.org/10.1186/s12903-019-0931-1 PMID: 31675959; PMCID: PMC6825342
Reynolds I, Duane B (2018) Periodontal disease has an impact on patients' quality of life. Evid Based Dent 19:14–15
Gaber A, Galarneau C, Feine JS, Emami E (2018)Rural-urban disparity in oral health-related quality of life. Community Dent Oral Epidemiol 46:132–142
Gürgan CA, Zaim E, Bakirsoy I, Soykan E (2006)Short-term side effects of 0.2% alcohol-free chlorhexidine mouthrinse used as an adjunct to non-surgical periodontal treatment: a double-blind clinical study. J Periodontol 77:370–384. https://doi.org/10.1902/jop.2006.050141 PMID: 16512751
Gjermo P, Bonesvoll P, Rölla G (1974) Relationship between plaque-inhibiting effect and retention of chlorhexidine in the human oral cavity. Arch Oral Biol 19:1031–1034. https://doi.org/10.1016/0003-9969(74)90090-9 PMID: 4531857
Burkhardt R, Lang NP (2014) Fundamental principles in periodontal plastic surgery and mucosal augmentation--a narrative review. J Clin Periodontol 4:S98–S107. https://doi.org/10.1111/jcpe.12193 PMID: 24641005
Chambrone L (2015)Evidence-based periodontal and peri-implant plastic surgery. A clinical roadmap from function to aesthetics. Springer Publishing, Cham
Bihani SN, Damle SG (1997) Evaluation of an alum-containing mouthrinse on plaque and gingivitis inhibition over 2 weeks of supervised use. J Indian Soc Pedod Prev Dent 15:34–38
Tsourounakis I, Palaiologou-Gallis AA, Stoute D, Maney P, Lallier TE (2013) Effect of essential oil and chlorhexidine mouthwashes on gingival fibroblast survival and migration. J Periodontol 84:1211–1220. https://doi.org/10.1902/jop.2012.120312 Epub 2012 Oct 29. Erratum in: J Periodontol. 2014 ;85(6):876. PMID: 23106509
Luís H, Luís L, Bernardo M, dos Santos N (2017) Randomized controlled trial on mouth rinse and flossing efficacy on interproximal gingivitis and dental plaque. Int J Dent Hyg 16:e73–e78
Gunsolley JC (2010) Clinical efficacy of antimicrobial mouthrinses. J Dent Suppl 1:S6–S10
Santos GOD, Milanesi FC, Greggianin BF, Fernandes MI, Oppermann RV, Weidlich P (2017) Chlorhexidine with or without alcohol against biofilm formation: efficacy, adverse events and taste preference. Braz Oral Res 31:e32. https://doi.org/10.1590/1807-3107BOR-2017
Coelho AS, Laranjo M, Gonçalves AC, Paula A, Paulo S, Abrantes AM, Caramelo F, Ferreira MM, Silva MJ, Carrilho E, Botelho MF (2020) Cytotoxic effects of a chlorhexidine mouthwash and of an enzymatic mouthwash on human gingival fibroblasts. Odontology 108:260–270
Osunde OD, Adebola RA, Adeoye JB, Bassey GO (2014) Comparative study of the effect of warm saline mouth rinse on complications after dental extractions. Int J Oral Maxillofac Surg 43:649–653. https://doi.org/10.1016/j.ijom.2013.09.016
Aravinth V, Narayanan MB, Kumar SG, Selvamary AL, Sujatha A (2017) Comparative evaluation of salt water rinse with chlorhexidine against oral microbes: a school-based randomized controlled trial. J Indian Soc Pedod Prev Dent 35:319–326
Osunde OD, Anyanechi CE, Bassey GO (2017) Prevention of alveolar osteitis after third molar surgery: comparative study of the effect of warm saline and chlorhexidine mouth rinses. Niger J Clin Pract 20:470–473
Huang BS, Wu SC, Lin CY, Fan KH, Chang JT, Chen SC (2018) The effectiveness of a saline mouth rinse regimen and education programme on radiation-induced oral mucositis and quality of life in oral cavity cancer patients: a randomised controlled trial. Eur J Cancer Care (Engl) 27:e12819. https://doi.org/10.1111/ecc.12819
Stewart M, Levey E, Nayyer N (2015) Salt water mouthwash post extraction reduced post operative complications. Evid Based Dent 16:27–28
Hoover J, Tovar E, Zlatnik T, Karunanayake C (2017) Efficacy of a rinse containing sea salt and lysozyme on biofilm and gingival health in a group of young adults: a pilot study. Int J Dent 2017:4056708–4056705. https://doi.org/10.1155/2017/4056708
Alling CC, Helfrick JF, Alling RD (1993) Impacted teeth. WB Saunders, Philadelphia, p 193
Rupesh S, Winnier JJ, Nayak UA, Rao AP, Reddy NV (2010) Comparative evaluation of the effects of an alum-containing mouthrinse and a saturated saline rinse on the salivary levels of Streptococcus mutans. J Indian Soc Pedod Prev Dent 28:138–144. https://doi.org/10.4103/0970-4388.73780
White GE, Armaleh MT (2004) Tongue scraping as a means of reducing oral mutans streptococci. J Clin Pediatr Dent 28:163–166. https://doi.org/10.17796/jcpd.28.2.n18275821658263v
Mariutti LR, Bragagnolo N (2017) Influence of salt on lipid oxidation in meat and seafood products: a review. Food Res Int 94:90–100. https://doi.org/10.1016/j.foodres.2017.02.003
Franco C, Patricia HR, Timo S, Claudia B, Marcela H (2017) Matrix metalloproteinases as regulators of periodontal inflammation. Int J Mol Sci 18:440. https://doi.org/10.3390/ijms18020440
Eren G, Tervahartiala T, Sorsa T, Atilla G (2016) Cytokine (interleukin-1beta) and MMP levels in gingival crevicular fluid after use of platelet-rich fibrin or connective tissue graft in the treatment of localized gingival recessions. J Periodontal Res 5:481–488
O’Leary TJ, Drake R, Naylor J (1972) The plaque control record. J Periodontol 43:38
Cortellini P, Tonetti MS (2007) A minimally invasive surgical technique with an enamel matrix derivative in the regenerative treatment of intra-bony defects: a novel approach to limit morbidity. J Clin Periodontol 34:87–93. https://doi.org/10.1111/j.1600-051X.2006.01020.x
Collins JR, Arredondo A, Roa A, Valdez Y, León R, Blanc V (2016) Periodontal pathogens and tetracycline resistance genes in subgingival biofilm of periodontally healthy and diseased Dominican adults. Clin Oral Investig 20:349–356. https://doi.org/10.1007/s00784-015-1516-2
Löe H, Silness J (1963) Periodontal disease in pregnancy. Acta Odontol Scand 21:533–551
Calvo-Guirado JL, Fernández Domínguez M, Aragoneses JM, Martínez González JM, Fernández-Boderau E, Garcés-Villalá MA, Romanos GE, Delgado-Ruiz R (2020) Evaluation of new seawater-based mouthrinse versus chlorhexidine 0.2% reducing plaque and gingivitis indexes. A randomized controlled pilot study. Appl Sci 10:982
Chen Y, Wong RW, McGrath C, Hagg U, Seneviratne CJ (2014) Natural compounds containing mouthrinses in the management of dental plaque and gingivitis: a systematic review. Clin Oral Investig 18:1–16
Chye RML, Perrotti V, Piattelli A, Iaculli F, Quaranta A (2019) Effectiveness of different commercial chlorhexidine-based mouthwashes after periodontal and implant surgery: a systematic review. Implant Dent 28:74–85. https://doi.org/10.1097/ID.0000000000000854
Giannelli M, Chellini F, Margheri M, Tonelli P, Tani A (2008) Effect of chlorhexidine digluconate on different cell types: a molecular and ultrastructural investigation. Toxicol in Vitro 22:308–317
Pucher JJ, Daniel JC (1992) The effects of chlorhexidine digluconate on human fibroblasts in vitro. J Periodontol 63:526–532
Huynh NC-N, Everts V, Leethanakul C, Pavasant P, Ampornaramveth RS (2016) Rinsing with saline promotes human gingival fibroblast wound healing in vitro. PLoS One 11:e0159843. https://doi.org/10.1371/journal.pone.0159843
Kapil V, Haydar SM, Pearl V, Lundberg JO, Weitzberg E, Ahluwalia A (2013) Physiological role for nitrate-reducing oral bacteria in blood pressure control. Free Radic Biol Med 55:93–100
Govoni M, Jansson EA, Weitzberg E, Lundberg JO (2008) The increase in plasma nitrite after a dietary nitrate load is markedly attenuated by an antibacterial mouthwash. Nitric Oxide 19:333–337
Bondonno CP, Liu AH, Croft KD, Considine MJ, Puddey IB, Woodman RJ, Hodgson JM (2015) Antibacterial mouthwash blunts oral nitrate reduction and increases blood pressure in treated hypertensive men and women. Am J Hypertens 28:572–575
Bescos R, Ashworth A, Cutler C, Brookes ZL, Belfield L, Rodiles A, Casas-Agustench P, Farnham G, Liddle L, Burleigh M, White D, Easton C, Hickson M (2020) Effects of Chlorhexidine mouthwash on the oral microbiome. Sci Rep 10:5254. https://doi.org/10.1038/s41598-020-61912-4
Aljateeli M, Koticha T, Bashutski J, Sugai JV, Braun TM, Giannobile WV, Wang H-L(2014) Surgical periodontal therapy with and without initial scaling and root planing in the management of chronic periodontitis: a randomized clinical trial. J Clin Periodontol 41:693–700. https://doi.org/10.1111/jcpe.12259
Armitage GC (1999) Development of a classification system for periodontal diseases and conditions. Ann Periodontol 4:1–6
Funding
This study was funded by the Pontifcia Universidad Católica Madre y Maestra and a competitive fund (V Competitive Research Fund, PUCMM 2014–2015), Santo Domingo, Dominican Republic.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in this study were in accordance with the ethical consideration of the Institutional Review Boards, Bioethics Committee Faculty of Health Sciences Pontificia Universidad Católica Madre y Maestra (COBE-FACS-EST-CSTA-001-3-2014-2015) and with the Declaration of Helsinki (1975), as revised in 2013.
Informed consent
All subjects signed an informed consent before enrolment.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Collins, J.R., Veras, K., Hernández, M. et al. Anti-inflammatory effect of salt water and chlorhexidine 0.12% mouthrinse after periodontal surgery: a randomized prospective clinical study. Clin Oral Invest 25, 4349–4357 (2021). https://doi.org/10.1007/s00784-020-03748-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-020-03748-w