Abstract
To explore the advantages and limitations of holmium laser resection of the bladder tumor (HOLRBT) versus standard transurethral resection of the bladder tumor (TURBT) in the treatment of non-muscle-invasive bladder cancer (NMIBC), the eligible studies were selected from the following databases: PubMed, Cochrane Library, and Embase. Studies comparing HOLRBT and TURBT for patients with NMIBC were included. The outcomes of interest were time of operation, catheterization and hospitalization, rates of recurrence, and perioperative complications, including obturator nerve reflex, bladder perforation, bladder irritation, and urethral stricture. Results of all data were compared and analyzed by Review Manager 5.3. A total of 9 comparative studies were finally included for this analysis. Pooled data demonstrated that HOLRBT significantly reduced the time to catheterization and hospitalization, the rate of recurrence in 2 years of follow-up, obturator nerve reflex, bladder perforation, and bladder irritation, compared with those in TURBT, respectively. However, no significant difference found between HOLRBT and TURBT in the time of operation, rate of recurrence in 1-year follow-up, and urethral stricture. The results of this research reached that HOLRBT would be a better choice than TURBT for patients with NMIBC.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Bladder cancer is the tenth most common cancer worldwide, with estimated 549,000 new cases and 200,000 deaths in 2018 [1]. According to the depth of invasion, bladder cancer was divided into two types, non-muscle-invasive bladder cancer (NMIBC) and muscle-invasive disease, and 75% of bladder cancer belongs to the former [2]. NMIBC is defined as the tumor is confined to the mucosa or submucosa of bladder.
Previously, the patients with NMIBC were usually treated by transurethral resection of the bladder tumor (TURBT) combined with intravesical chemotherapy or immunotherapy [3]. This strategy above was the “golden standard” according to the guideline of European Association of Urology [4]. However, the limitations of TURBT were gradually presented, such as the occurrences of obturator nerve reflex, bladder perforation, bladder irritation, and postoperative bleeding. Holmium laser resection of the bladder tumor (HOLRBT) was applied to overcome these shortages, which showed satisfactory outcomes, especially in tissue cutting, vaporization, and hemostasis [5]. The aim of our study was to compare the safety and effectiveness of HOLRBT and TURBT for patients with NMIBC.
Methods
Search strategy
This study was performed following the principle of preferred reporting items for systematic review and meta-analysis protocols (PRISMA) [6]. The databases included PubMed, Cochrane Library, and EMBASE and were respectively searched with the term in title/abstract: “superficial bladder cancer,” “non-muscle-invasive bladder cancer,” “holmium laser,” and “transurethral resection” up to March 2019. The reference lists from the identified documents were also searched. To avoid data duplication, the latest report was used if multiple studies described the same population.
Inclusion and exclusion criteria
All comparative studies, including randomized controlled studies (RCT), cohort studies (CS), and case-control studies (CCS), focusing on HOLRBT and TURBT for patients with NMIBC were included. On the other hand, studies would be excluded if (1) studies included patients with muscle-invasive-bladder cancer or distant metastasis; (2) none of the following outcomes of interest were reported, including time of operation, catheterization and hospitalization, rate of recurrence, and complications, such as obturator nerve reflex, bladder perforation, bladder irritation, and urethral stricture; (3) data of studies were not sufficient for a meta-analysis; and (4) studies presented as conference abstracts.
Data extraction
Data were extracted from these studies by 2 independent reviewers. If the two reviewers disagreed, a consensus was reached after a discussion between them. To keep the baselines as similar as possible, the only comparison between HOLRBT and TURBT was extracted when the patients were divided into ≥ 3 groups in studies. When articles were not written in English, they were translated for data extraction if possible.
Outcomes of interest
The outcomes of interest were time of operation, catheterization and hospitalization, rate of recurrence, and perioperative complications, including obturator nerve reflex, bladder perforation, bladder irritation, and urethral stricture.
Quality assessment and statistical analysis
The level of evidence of the included studies was graded according to the criteria by the Centre for Evidence-Based Medicine in Oxford, UK [7]. In addition, the quality of each included CS or CCS was evaluated by the Newcastle-Ottawa scale (NOS). The NOS was a widely used quality assessment method in meta-analysis [8]. In the modified Newcastle-Ottawa scale, a score of 1–9 stars was allocated, and more stars stood for higher quality.
The meta-analysis was performed by Review Manager 5.3. The odd ratio (OR) and mean difference (MD) were used for describing results of dichotomous and continuous variables, respectively. All results were reported with 95% confidence intervals (CI). The P < 0.05 was regarded to be statistically significant.
In addition, statistical heterogeneities among trials were evaluated by I2 and χ2 tests. I2 value of 25%, 50%, and 75% was corresponded to low, medium, and high levels of heterogeneity, respectively. When I2 < 50% and P > 0.10, a fixed-effect model was used. Otherwise, the random-effect model was applied.
Results
Study selection
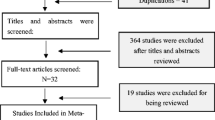
Through the search strategy, a total of 317 articles were initially found. After software and manual checking, 85 papers were excluded because of duplications. Then, 203 documents were excluded after screening of the title and abstract. Of the 29 remaining records, 20 articles were excluded after evaluation of the full text. Finally, 9 studies [9,10,11,12,13,14,15,16,17] with a total of 1166 patients were included in the meta-analysis, in which 473 patients were treated by HOLRBT and 693 patients were treated by TURBT (Fig. 1).
Eight studies had described the gender of patients, in which 335 were males in HOLRBT group (74.8%) and 506 were males in the TURBT group (77.7%). The chi-square test showed that there was an insignificant difference in gender between two groups (P = 0.26). More, the pooled average age of patients between two groups was similar, which was calculated to be 64.34 in HOLRBT group and 66.17 in TURBT group, respectively. The characteristics of all available studies are shown in Table 1.
Totally, 1 RCT, 3 prospective CS, and 5 retrospective CCS were included in this analysis. According to the postoperative intravesical instilled chemotherapy scheme, 4 studies used mitomycin C, 2 studies used epirubicin, 2 studies used pirarubicin, and 1 study did not describe the chemotherapy scheme. Five studies [9,10,11, 15, 17] described a comparison of ≥ 3 groups, in which only data describing HOLRBT and TURBT for NMIBC were extracted. One study was published in Chinese, however had an English abstract [12].
Outcomes of interest
Operation time
Eight studies including a total of 1142 patients [9,10,11,12, 14,15,16,17] had evaluated data of operation time, which revealed that there was no significant difference in operation time between two groups (MD = − 0.76, 95% CI [− 3.10, 1.58], P = 0.53) (Fig. 2).
Catheterization time
When catheterization time was compared, 8 studies including 1142 patients [9,10,11,12, 14,15,16,17] were analyzed. Pooled data demonstrated a significantly less time in catheterization time in the HOLRBT group compared to TURBT group (MD = − 1.02, 95% CI [− 1.35, − 0.68], P < 0.00001) (Fig. 3).
Hospitalization time
Seven studies including 1002 patients [9,10,11, 14,15,16,17] are pooled, which indicated that hospitalization time was significantly less in HOLRBT group compared to TURBT group (MD = − 1.11, 95% CI [− 1.65, − 0.58], P < 0.0001) (Fig. 4).
1-year recurrence
Data describing the rate of 1-year recurrence were pooled from 5 studies [12,13,14, 16, 17] of 493 patients. Result of meta-analysis showed that there was an insignificant difference between two groups (OR = 0.72; 95% CI [0.45, 1.16], P = 0.18). Considering the large impact on recurrence by different chemotherapy schemes, a subgroup analysis was carried out, which showed that there was an insignificance in mitomycin C, epirubicin, pirarubicin, and subgroups that did not mention chemotherapy scheme (Fig. 5).
2-year recurrence
When the rate of 2-year recurrence was compared between two groups, pooled data from 8 studies including a total of 939 patients [9, 10, 12,13,14,15,16,17] revealed that the recurrence was significantly higher in TURBT group (OR = 0.69; 95% CI [0.51, 0.94], P = 0.02). However, in the subgroup analysis, all results became insignificant in mitomycin C, epirubicin, pirarubicin subgroups, and in the subgroup that did not describe chemotherapy scheme (Fig. 6).
Complications
Four studies [10, 12, 15, 17] evaluated the incidence of obturator nerve reflex, which revealed significantly lower rate of occurrence in the HOLRBT group (OR = 0.06; 95% CI [0.01, 0.23], P < 0.0001) (Fig. 7).
Additionally, seven studies including 860 patients [9, 10, 12, 14,15,16,17] were pooled, which presented that the incidence of bladder perforation was significant lower in the HOLRBT group (OR = 0.15; 95% CI [0.05, 0.45], P = 0.0008) (Fig. 8).
What is more, six studies including 648 patients [9, 10, 12, 14,15,16] evaluated the incidence of bladder irritation and revealed a significant difference between two groups and lower incidence of bladder irritation in HOLRBT group (OR = 0.45; 95% CI [0.31, 0.66], P < 0.0001) (Fig. 9).
When urethral stricture was compared between HOLRBT and TURBT groups, 4 studies [10, 12, 15, 16] including 444 patients were pooled. The result of meta-analysis showed that there was an insignificance in urethral stricture between two groups (OR = 0.86, 95% CI [0.37, 1.98], P = 0.73) (Fig. 10).
Sensitivity analysis and publication bias
To analyze the potential publication bias, a funnel plot of operation time was performed, which revealed that 2 studies had potential publication bias. After the studies were excluded, similar results in all outcomes of interest were shown (Fig. 11).
Discussion
With the increasing of patients with NMIBC, it became a key issue how to improve the survival and quality of patients’ life. Nowadays, TURBT still played an important role in the diagnosis and treatment of NMIBC, because it could provide adequate tissue for pathological examination followed with all visible tumors being effectively removed [18, 19]. However, thermal injury was the main factor which leads to complications by TURBT, due to the radiofrequency that had developed an electrical resistance at a temperature that ranged from 100 to 300 °C in the treatment site [20]. According to the reason above, the occurrence of obturator nerve reflex was frequent during TURBT, especially for tumors at the lateral wall of bladder, which possibly leaded to bladder perforation [21]. In order to avoid these complications, inadequate resection depth of the tumors might occur [22]. Meanwhile, the time to catheterization and hospitalization might be longer by thermal injury.
Fortunately, after laser was firstly applied in urology in 1978 [23], holmium laser was gradually used in the resection of bladder tumors since 2001 [24]. In the beginning, the most obvious shortage of laser was unable to reach sufficient tissue for pathological examination in the treatment of NMIBC. Nonetheless, holmium laser can not only offer adequate tissue for pathological examination, and even accomplish en bloc resection of NMIBC [25, 26]. Holmium laser had a wavelength of 2100 nm. At this wavelength, the tissue penetration depth of the laser was about 400 μm, which was considered safely. The temperature of the treatment regions in HOLRBT ranged from 40 to 75 °C, which was large lower than in TURBT. Thus, the thermal injury in the treatment site was minimal as well [26]. It made a necessary to compare these two technologies.
Our results showed that the time of catheterization and hospitalization was significantly shorter in the HOLRBT group than the TURBT group; however, there was no significant difference in operation time. The same conclusions were reported by Teng et al. [27]. For the time of catheterization and hospitalization, rapider postoperative recovery was shown in the HOLRBT group because of thermal damage caused by TURBT. Nonetheless, significant heterogeneities among studies could be found, and the accuracy of results might be influenced.
Our study revealed that HOLRT had a significant benefit in 2-year recurrence compare with TUBRT, which could be calculated to be 26.1% in HOLRBT group and 34.3% in TURBT group, respectively. In addition, the rate of 1-year recurrence was insignificant. Considering the difference of postoperative intravesical instilled chemotherapy scheme, subgroup analysis was carried out. Though postoperative adjuvant intravesical chemotherapy was an important factor which may affected the recurrence of cancer [28], no significant difference was found in our study. However, more evidence should be discovered to verify this conclusion.
Our study further confirmed the incidences of several perioperative complications, including obturator nerve reflex, bladder perforation, and bladder irritation, which presented large advantages in the HOLRBT group. The rate of obturator nerve reflex, bladder perforation, and bladder irritation could be calculated to be 0%, 0.2%, and 22.0% in HOLRBT group and 11.2%, 5.3%, and 39.1% in TURBT group, respectively. In addition, our study showed that there was an insignificance in the rate of urethral stricture between two groups, which could be calculated to be 4.8% in HOLRBT group and 5.8% in TURBT group, respectively. Based on these results, it seemed that HOLRBT would be safer than TURBT for patients with NMIBC.
Above all, some limitations should be taken into consideration in this study. Firstly, only one RCT was included for analysis, which would lower the quality of pooled results. Secondly, some important parameters were not analyzed because the description of them could not be uniformed, such as pre- and postoperative bleeding. Thirdly, high heterogeneity could be observed in outcomes of operation time, catheterization time, and hospitalization time. These might due to the differences of patient’s condition, surgeons’ technique and custom, etc.
Conclusions
Based on the results of our meta-analysis, HOLRBT showed similar effectiveness and superior safety than TURBT for patients with NMIBC, though sporadical insignificance between two groups was found. However, more high-quality clinical trials were needed to further confirm our conclusions.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- HOLRBT:
-
Holmium laser resection of the bladder tumor
- TURBT:
-
Transurethral resection of the bladder tumor
- NMIBC:
-
Non-muscle-invasive bladder cancer
- PRISMA:
-
Preferred reporting items for systematic review and meta-analysis protocols
- NOS:
-
Newcastle-Ottawa scale
- RCT:
-
Randomized controlled studies
- CS:
-
Cohort studies
- CCS:
-
Case-control studies
- OR:
-
Odd ratio
- MD:
-
Mean difference
- CI:
-
Confidence intervals
- LOE:
-
Level of evidence
- NA:
-
Not available
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424. https://doi.org/10.3322/caac.21492
Burger M, Catto JW, Dalbagni G et al (2013) Epidemiology and risk factors of urothelial bladder cancer. Eur Urol 63(2):234–241. https://doi.org/10.1016/j.eururo.2012.07.033
Babjuk M, Bohle A, Burger M et al (2017) EAU guidelines on non-muscle-invasive urothelial carcinoma of the bladder: update 2016. Eur Urol 71(3):447–461
Kaufman DS, Shipley WU, Feldman AS (2009) Bladder cancer, Lancet (London, England). 374(9685):239–249. https://doi.org/10.1016/s0140-6736(09)60491-8
Zarrabi A, Gross AJ (2011) The evolution of lasers in urology. Ther Adv Urol 3(2):81–89. https://doi.org/10.1177/1756287211400494
Moher D, Liberati A, Tetzlaff J, Altman DG (2010) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg (London, England) 8(5):336–341. https://doi.org/10.1016/j.ijsu.2010.02.007
Phillips B (2004) GRADE: levels of evidence and grades of recommendation. Arch Dis Child 89(5):489
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25(9):603–605. https://doi.org/10.1007/s10654-010-9491-z
Chen GF, Shi TP, Wang BJ, Wang XY, Zang Q (2015) Efficacy of different resections on non-muscle-invasive bladder cancer and analysis of the optimal surgical method. J Biol Regul Homeost Agents 29(2):465–470
Huang JH, Hu YY, Liu M, Wang GC, Peng B, Yao XD (2016) Comparative study of 2 um laser versus holmium laser for the resection of non-muscle invasive bladder cancer. Int J Clin Exp Med 9(12):23618–23623
Kramer MW, Rassweiler JJ, Klein J et al (2015) En bloc resection of urothelium carcinoma of the bladder (EBRUC): a European multicenter study to compare safety, efficacy, and outcome of laser and electrical en bloc transurethral resection of bladder tumor. World J Urol 33(12):1937–1943. https://doi.org/10.1007/s00345-015-1568-6
Luo Y, Cao ZG, Liu J, Su JH, Zhu JG, Xu Z (2008) A comparison of clinical outcome between holmium laser resection and transurethral resection for superficial bladder carcinoma. Tumor 28(11):1001–1003. https://doi.org/10.3781/j.issn.1000-7431.2008.11.022
Muraro GB, Grifoni R, Spazzafumo L (2005) Endoscopic therapy of superficial bladder cancer in high-risk patients: holmium laser versus transurethral resection. Surg Technol Int 14:222–226
Verma A, D'Souza N (2016) Holmium laser transurethral resection of bladder tumor: our experience. Indian J Urol 32
Xishuang S, Deyong Y, Xiangyu C et al (2010) Comparing the safety and efficiency of conventional monopolar, plasmakinetic, and holmium laser transurethral resection of primary non-muscle invasive bladder cancer. J Endourol 24(1):69–73. https://doi.org/10.1089/end.2009.0171
Zhong C, Guo S, Tang Y, Xia S (2010) Clinical observation on 2 micron laser for non-muscle-invasive bladder tumor treatment: single-center experience. World J Urol 28(2):157–161. https://doi.org/10.1007/s00345-010-0532-8
Zhu Y, Jiang X, Zhang J, Chen W, Shi B, Xu Z (2008) Safety and efficacy of holmium laser resection for primary nonmuscle-invasive bladder cancer versus transurethral electroresection: single-center experience. Urology 72(3):608–612. https://doi.org/10.1016/j.urology.2008.05.028
Babjuk M, Bohle A, Burger M et al (2017) EAU guidelines on non-muscle-invasive urothelial carcinoma of the bladder: update 2016. Eur Urol 71(3):447–461. https://doi.org/10.1016/j.eururo.2016.05.041
Herrmann TR, Liatsikos EN, Nagele U, Traxer O, Merseburger AS (2012) EAU guidelines on laser technologies. Eur Urol 61(4):783–795. https://doi.org/10.1016/j.eururo.2012.01.010
Issa MM (20008) Technological advances in transurethral resection of the prostate: bipolar versus monopolar TURP. J Endourol 22:1587–1595
Khorrami MH, Javid A, Saryazdi H, Javid M (2010) Transvesical blockade of the obturator nerve to prevent adductor contraction in transurethral bladder surgery. J Endourol 24(10):1651–1654. https://doi.org/10.1089/end.2009.0659
Mariappan P, Zachou A, Grigor KM (2010) Detrusor muscle in the first, apparently complete transurethral resection of bladder tumour specimen is a surrogate marker of resection quality, predicts risk of early recurrence, and is dependent on operator experience. Eur Urol 57(5):843–849. https://doi.org/10.1016/j.eururo.2009.05.047
Staehler G, Schmiedt E, Hofstetter A (1978) Destruction of bladder neoplasms by means of transurethral neodym-YAG-laser coagulation. Helv Chir Acta 45(3):307–311
Saito S (2001) Transurethral en bloc resection of bladder tumors. J Urol 166(6):2148–2150
Hurle R, Lazzeri M, Colombo P et al (2016) “En bloc” resection of nonmuscle invasive bladder cancer: a prospective single-center study. World J Urol 33:1937–1943
Kramer MW, Wolters M, Herrmann TR (2016) En bloc resection of bladder tumors: ready for prime time? Eur Urol 69:967–968
Teng JF, Wang K, Yin L, Qu FJ, Zhang DX, Cui XG, Xu DF (2013) Holmium laser versus conventional transurethral resection of the bladder tumor. Chin Med J 126(9):1761–1765
Oosterlinck W, Decaestecker K (2018) Update on early instillation of chemotherapy after transurethral resection of non-muscle-invasive bladder cancer. Expert Rev Anticancer Ther 18(5):437–443. https://doi.org/10.1080/14737140.2018.1451748
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Statement of informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, C., Gao, L., Zhang, J. et al. The effect of holmium laser resection versus standard transurethral resection on non-muscle-invasive bladder cancer: a systematic review and meta-analysis. Lasers Med Sci 35, 1025–1034 (2020). https://doi.org/10.1007/s10103-020-02972-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-020-02972-w