Abstract
Onychomycoses represent approximately 50 % of all nail diseases worldwide. In warmer and more humid countries like Brazil, the incidence of onychomycoses caused by non-dermatophyte molds (NDM, including Fusarium spp.) or yeasts (including Candida albicans) has been increasing. Traditional antifungal treatments used for the dermatophyte-borne disease are less effective against onychomycoses caused by NDM. Although some laser and light treatments have demonstrated clinical efficacy against onychomycosis, their US Food and Drug Administration (FDA) approval as “first-line” therapy is pending, partly due to the lack of well-demonstrated fungicidal activity in a reliable in vitro model. Here, we describe a reliable new in vitro model to determine the fungicidal activity of laser and light therapies against onychomycosis caused by Fusarium oxysporum and C. albicans. Biofilms formed in vitro on sterile human nail fragments were treated with 1064 nm neodymium-doped yttrium aluminum garnet laser (Nd:YAG), 420 nm intense pulsed light (IPL) IPL 420, followed by Nd:YAG, or near-infrared light ((NIR) 700–1400 nm). Light and laser antibiofilm effects were evaluated using cell viability assay and scanning electron microscopy (SEM). All treatments were highly effective against C. albicans and F. oxysporum biofilms, resulting in decreases in cell viability of 45–60 % for C. albicans and 92–100 % for F. oxysporum. The model described here yielded fungicidal activities that matched more closely to those observed in the clinic, when compared to published in vitro models for laser and light therapies. Thus, our model might represent an important tool for the initial testing, validation, and “fine-tuning” of laser and light therapies against onychomycosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Onychomycosis is a nail infection caused by a variety of fungal agents, and which affects approximately 5 % of the population worldwide [1], representing up to 50 % of all nail diseases [2]. In the Northern Hemisphere, onychomycosis caused by Trichophyton mentagrophytes or Trichophyton rubrum is more common [2–5] while in warmer and more humid countries, the incidence of non-dermatophyte molds (NDM), such as Fusarium sp. or yeasts such as Candida albicans, as the causative agent of these infections has been increasing [6].
Traditional topical or systemic antifungal treatments used for onychomycosis caused by dermatophytes—such as polyenes (amphotericin B), triazoles (fluconazole, itraconazole), imidazoles (clotrimazole, ketoconazole, miconazole), morpholines (amorolfine), and allylamines (terbinafine) [7, 8]—are less effective against onychomycosis caused by NDM (including Fusarium spp.), which are resistant in vitro to many of the antifungal compounds licensed for the treatment of fungal infections [9, 10]. In 2010, Bourgeois and co-workers reported a case of disseminated Fusarium infection originating from a toenail mycose in a neutropenic patient, where combined treatment with amphotericin B and voriconazole failed to contain the infection and the patient died from fusariosis [11]. Aside from the poor efficacy of the current treatment regimens, patients with renal or hepatic diseases may not be able to use systemic drugs against onychomycosis, reinforcing that alternative treatments are urgently needed, especially for onychomycoses caused by NDM fungi and yeasts.
The chronic nature of onychomycosis is often attributed to the difficulty in eliminating the pathogen [7] which can remain in reservoirs of difficult access by antifungal drugs [7, 12], with 30–50 % of cases failing to reach total cure using a combination of oral and topical antifungals and with a recurrence rate of 10–53 % [13, 14]. The need for noninvasive, safe, and effective therapy alternatives to treat onychomycosis has led to the testing of laser- and light-based treatments [15]. Although the exact mechanism of laser and light therapies is still under investigation, it may combine the direct fungicidal effects (apoptosis induced by heat) with local immune system modifications [16]. Previous studies have shown that near-infrared (NIR) application at physiological temperatures leads to photoinactivation of Staphylococcus aureus, Escherichia coli, C. albicans, and T. rubrum by changing the electrical potential across cell membranes and increasing the levels of reactive oxygen species (ROS) [17].
The efficacy of NIR [17, 18] and of 1064 nm neodymium-doped yttrium aluminum garnet (Nd:YAG) [14, 19–21] light and laser systems in the treatment of onychomycosis has been demonstrated in clinical trials [14, 17–19] and in vitro studies [20, 21]. In clinical trials, Nd:YAG laser treatment led to 87–51 % of negative cultures after 1–3 sessions of treatment [14, 19] while NIR treatment led to 100 % of negative cultures [17] and was effective against mild, moderate, and severe cases of onychomycosis [18]. Local application of blue light, as intense pulsed light (IPL) 420 nm, has been described as a successful treatment for acne [22–25]; however, no clinical or in vitro study has demonstrated the use of IPL 420 nm in the treatment of nail fungal infections.
Despite the available evidence for the efficacy of several laser and light uses in the treatment of onychomycosis, the US Food and Drug Administration (FDA) has approved the use of laser systems only for the increase of clear nails in onychomycosis [26], since these systems have only been tested in limited clinical trials, and basic studies are still lacking [27]. In fact, there is a clear discrepancy between the large number of available laser systems and the reduced amount of published data concerning their therapeutic benefit [28].
Analysis of laser efficacy usually uses patient’s nail fragments collected after laser application for in vitro culture growth observation [17–19]. Although this model is effective to evaluate patient’s response to the treatment, it is not applicable for the testing of newly developed lasers and of novel laser and/or light combination therapy regimens that are not FDA approved. Well-established and reliable in vitro models are necessary for high-throughput initial screening of novel laser and light therapies. In vitro studies attempting to evaluate the fungicidal activity of laser and light therapies mostly use cell cultures or fungal colonies as substrates for laser irradiation [20, 29, 30]. A recent in vitro work using T. rubrum colonies showed no inhibition of fungal growth with Nd:YAG laser treatment [30]. These results are not in agreement with those from Paasch and colleagues [31], who reported growth inhibition of T. rubrum, Trichophyton interdigitale, Microsporum gypseum, Candida parapsilosis, and Candida guilliermondii on nail clippings obtained from patients with onychomycosis after treatment with 1064 or 980 nm laser systems. These results suggest that fungal cultures or colonies are not appropriate for the testing of laser treatment efficacy. It is possible that the reliability of in vitro laser and light testing could be improved by using substrates closely related to the in vivo system.
In nails, fungal cells usually form thick biomasses embedded in an extracellular matrix and containing dormant fungal elements [12]. These features led to a recent debate on whether onychomycosis lesions should be considered biofilms. Several factors including firm adherence of dermatophytes to the nail plate, presence of dormant fungal elements, the ability of yeasts to form biofilms, and the difficulty of infection eradication suggest that biofilms are likely to be an important factor in onychomycosis pathogenesis [32].
Given the lack of suitable in vitro methods to test the fungicidal potential of laser and light treatments, and the importance of biofilm formation in onychomycosis, the aim of this work was to examine the potential of a new in vitro model of fungal biofilms developed on human nail fragments for the evaluation of the fungicidal activity of four different laser and/or light treatments: Nd:YAG 1064 nm, intense pulsed light (IPL) 420 nm, NIR 700–1400 nm, and the combined application of IPL 420 followed by Nd:YAG. C. albicans and F. oxysporum were chosen as models for this study because in vitro biofilm formation by these species is well established in our laboratory [33], and also, these species are particularly relevant onychomycosis pathogens in Brazil, where the study was performed, since the frequent use of “open” footwear exposes the feet to fungi found in the soil (such as F. oxysporum), while the common practice of manicure with complete cuticle removal (often performed without adequate cleaning and sterilization) exposes nails to C. albicans infections.
Materials and methods
Microorganisms
C. albicans SC 5314 and F. oxysporum ATCC 48112 reference strains were used in this study. Both strains were maintained in Sabouraud dextrose agar (SDA), at 4 °C, and these stocks were kept for no longer than 30 days. Prior to use in experiments, F. oxysporum was subcultured on SDA for 10 days at 28 °C, and Candida albicans was subcultured on Sabouraud dextrose broth, for 24 h, at 35 °C. After growth period, F. oxysporum colonies were gently scraped from the agar media, and the conidia were separated by filtration and washed in 0.1 M phosphate buffer saline ((PBS) pH 7.2) prior to use in experiments. C. albicans cells grown in liquid culture were collected by centrifugation and washed twice in PBS (pH 7.2) prior to use in experiments.
Human nail collection and preparation
Fingernail fragments were aseptically collected using scissors from healthy volunteers, cut into small pieces (each fingernail fragment was cut in the middle, using sterile razor blades, generating fragments of approximately 0.5 cm in length), and autoclaved prior to use. All volunteers were adult females with no fungal infection history, and nails were at least 2 weeks polish-free.
In vitro nail biofilm model
Biofilms were formed on the inner surface of sterile sections of human nails placed inside wells of polystyrene, flat-bottomed 96-well plates (TPP Techno Plastic Products AG, Switzerland). Aliquots of 100 μL of standardized cell suspensions of C. albicans yeasts (107 colony-forming units or CFU/mL) or F. oxysporum conidia (106 CFU/mL) were transferred into each well containing nail fragments, and plates were incubated for 90 min at 36 °C (adhesion phase), under constant agitation (at 150 rpm). Then, cell suspensions were gently aspirated, 100 μL of RPMI 1640 (Sigma-Aldrich Co., USA) supplemented with 2 % glucose and 20 % fetal bovine serum (FBS) (Gibco®, USA) were added to each well, and the plates were incubated for 24 h (C. albicans) or 48 h (F. oxysporum) at 36 °C, and under constant agitation (150 rpm), to allow biofilm growth along the inner surface of the nail.
Laser and light treatments
Before experiments, nails containing mature biofilms formed in vitro were washed in 0.1 M PBS (pH 7.2) placed inside wells of 6-well plates (TPP Techno Plastic Products AG, Switzerland) and then subjected to one of following laser/light treatments using a Sciton JOULE 7 (Sciton Inc., CA, USA): (i) Nd:YAG (1064 nm), (ii) intense pulsed light 420 nm filter (IPL 420), (iii) a combination of IPL 420 and Nd:YAG, and (iv) near infrared (NIR 700–1400 nm). Control nails with mature biofilms were maintained at the 96-well plate. At least four nail fragments were subjected to each treatment, at the same time, and inside the same well. Laser application was directed to the entire nail fragment.
The Nd:YAG 1064 nm laser was used with a pulse duration of 0.3 ms, at low energy (5 to 7 J/cm2), with a frequency of 4.0 Hz, and using a 6-mm spot. Nails were subjected to 1032 or 1344 laser pulses (for C. albicans and F. oxysporum, respectively). The temperature inside (as determined by an integrated infrared thermometer within the laser tip) did not exceed 44 °C.
IPL 420 was applied with a 420-nm bandpass filter, i.e., excluding wavelengths other than 420 nm, and nails were subjected to 256 pulses of 200 ms each, at low energy (8 J/cm2). The final temperature inside wells after light treatment was determined manually using a high-temperature infrared thermometer Instrutherm IT-870 (Instrutherm, Brazil), and it did not exceed 37 °C (physiological hyperthermia).
The combined use of laser and light treatment was performed with the application of 256 pulses of IPL 420 nm followed by 357 or 309 pulses of Nd:YAG 1064 nm, for C. albicans and F. oxysporum, respectively, using the same parameters described above.
NIR (700–1400 nm) was used at 150 J/cm2, with a pulse duration of 12 ms. Nails were subjected to 27 pulses for both C. albicans and F. oxysporum biofilms. Temperature during light application was monitored manually using a high-temperature infrared thermometer Instrutherm IT-870 (Instrutherm, Brazil) and was maintained between 40 and 43 °C.
Scanning electron microscopy
Nail sections containing biofilms were processed for scanning electron microscopy (SEM) as previously described [33]. Briefly, nails were washed in 0.01 M PBS, pH 7.2, and fixed for 1 h at room temperature in 2.5 % glutaraldehyde and 4 % formaldehyde, in 0.1 M cacodylate buffer. Then, nails were washed in the same buffer, postfixed in 1 % osmium tetroxide and 1.25 % potassium ferrocyanide for 2 h, and dehydrated in a series of ethanol solutions of increasing concentrations (30, 50, 70, 90, 100 % and ultra-dry ethanol), for 30 min at each concentration. Samples were critically point dried in CO2, coated with gold, and observed in a FEI Quanta 250 scanning electron microscope (FEI, The Netherlands).
Biofilm cell viability assay
After laser and/or light application, nails containing biofilms were transferred to microcentrifuge tubes containing 1 mL of PBS 0.1 M, pH 7.2, and biofilms were disrupted by sonication (10 min) followed by vortexing (2 min). An aliquot (10 μL) of the suspension containing the biofilm-disrupted cells was plated in fresh SDA for 48 h at 35 °C (for C. albicans) or 10 days at 28 °C (for F. oxysporum). C. albicans samples were diluted (1:100) in PBS prior to plating. The number of colonies formed after incubation was determined by manual counting, and biofilm cell viability was expressed as CFU/10 μL of biofilm cell suspension. The percentage of inhibition associated to each treatment was calculated in relation to the CFU of control group, using the following formula: % of inhibition = [100 − (100 × Ct/Cc)], where Ct stands for the CFU of control group and Ct corresponds to the CFU of the treated group.
Results
C. albicans and F. oxysporum formed dense and highly filamentous biofilms over nail fragments in vitro
After 24 h of in vitro incubation of C. albicans yeast cells with nail fragments, the entire fragment surface was covered by a dense C. albicans biofilm. The typical C. albicans biofilm structure [33–35] could be observed, with a complex network of interconnected hyphae and numerous buds (Fig. 1a–c). During in vitro biofilm development, F. oxysporum conidia converted to mycelia, forming filamentous biofilms (Fig. 2a–c). Nail fragments incubated with F. oxysporum cultures displayed a less dense biofilm than those incubated with C. albicans cultures (Figs. 1 and 2a–c).
Scanning electron microscopy (SEM) analysis of Candida albicans nail biofilms after laser and/or light treatments. Biofilms were formed in vitro on sterile human nail fragments, for 24 h, at 36 °C and under constant agitation (150 rpm). Untreated control biofilms (a–c) or biofilms treated with 1064 nm neodymium-doped yttrium aluminum garnet (Nd:YAG) (d–f), 420 nm intense pulsed light (IPL) (g–i), IPL 420 followed by Nd:YAG (j–l), or near-infrared (NIR) light (m–o) were examined by SEM. Nd:YAG and IPL 420, used alone or in combination, led to the appearance of large amounts of extracellular matrix (white arrows in f, i, and l) in biofilms. However, no significant surface alterations were observed on biofilm cells after laser or light treatments. Scale bars indicate 500 μm (a, m); 1 mm (d, g, j); 25 μm (b, e, h, n); 10 μm (k); and 2.5 μm (c, f, i, l, o)
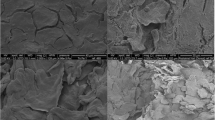
Scanning electron microscopy analysis of Fusarium oxysporum nail biofilms after laser and/or light treatments. Biofilms were formed in vitro on sterile human nail fragments, for 48 h, at 36 °C and under constant agitation (150 rpm). Untreated control biofilms (a–c) or biofilms treated with 1064 nm neodymium-doped yttrium aluminum garnet (Nd:YAG) (d–f), 420 nm intense pulsed light (IPL) (g–i), IPL 420 followed by Nd:YAG (j–l), or near-infrared light (NIR) (m–o) were examined by SEM. Extracellular matrix (ECM) was observed around the cells of control biofilms and covered biofilm cells after IPL 420 application (white arrows in c and i). After Nd:YAG and NIR applications, some cells appeared to have a “hole” in their surface, with a possible leakage of intracellular material (f and white arrowhead in o). Cell surface damage was clear after IPL 420 application (narrow white arrow in i), and large buds were observed after NIR (narrow white arrow in n). Scale bars indicate 500 μm (a); 2 mm (d, g, j, m); 25 μm (b); 20 μm (e, h, k, n); 10 μm (c, i, o); 5 μm (l); and 2.5 μm (f)
Laser and/or light treatments of C. albicans nail biofilms formed in vitro leads to a 45–60 % decrease in biofilm cell viability
Mature C. albicans biofilms formed on sterile human nail fragments in vitro were submitted to different laser and/or light treatments, and treatment effects were evaluated by SEM and biofilm cell viability (i.e., colony growth after plating on fresh agar medium) analyses. Nd:YAG 1064 nm and IPL 420 nm, used alone or in combination, led to the appearance of large amounts of extracellular matrix (ECM) in biofilms (Fig. 1, white arrows in f, i, and l), which was not observed in control, untreated biofilms (Fig. 1c), or after NIR treatment (Fig. 1o). No relevant surface alterations were observed on biofilm cells after laser or light treatment; however, plating of biofilm cells after treatment showed that all treatments tested led to a decrease in biofilm cell viability (Fig. 3a). When compared to untreated biofilms, laser and/or light treatments induced a reduction of approximately 50 % on C. albicans biofilm cell viability (Table 1). Also, the application of Nd:YAG 1064 nm after IPL 420 nm had improved fungicidal activity compared to that observed using IPL 420 nm alone (53 and 45 % decrease in biofilm cell viability, respectively), although the combination of IPL 420 nm with Nd:YAG 1064 nm was as effective as Nd:YAG 1064 nm alone, resulting in a decrease of 52 % in biofilm cell viability (Fig. 3a; Table 1). Importantly, the largest decrease in biofilm cell viability was obtained after NIR application (60 %) (Table 1).
Biofilm cell viability after laser and/or light treatments. The following laser and/or light treatments were tested: neodymium-doped yttrium aluminum garnet (Nd:YAG), 420 nm intense pulsed light (IPL), IPL 420, followed by Nd:YAG, and near-infrared light (NIR). Biofilm cell viability after treatment was estimated by plating untreated or treated Candida albicans (a) and Fusarium oxysporum (b) biofilm cells (removed from nail fragments by sonication and vortexing) on Sabouraud dextrose agar and determining the number of colony-forming units (CFU) per 10 μL of biofilm cell suspension after growth for 48 h at 36 °C (for C. albicans) or for 10 days at 28 °C (for F. oxysporum). For both fungal species, all treatments led to a reduction in biofilm cell viability. F. oxysporum biofilms were more sensitive to treatments (particularly to ND:YAG and to IPL 420, alone or in combination) than C. albicans biofilms
Laser and/or light treatments are highly effective against F. oxysporum nail biofilms formed in vitro
Mature F. oxysporum biofilms formed on sterile human nail fragments in vitro were submitted to laser and/or light treatments, and their effects were evaluated as described above for C. albicans biofilms. Laser and light treatments were highly effective against F. oxysporum biofilms (Table 1 and Figs. 2 and 3b). Unlike untreated C. albicans biofilms, which lacked a clearly visible ECM when observed by SEM, limited amounts of ECM material were observed around the cells of F. oxysporum untreated control biofilms (Fig. 2, white arrows in c). ECM material also appeared to cover F. oxysporum cells after IPL 420 nm treatment (Fig. 2, white arrows in i). After treatment with Nd:YAG 1064 nm or NIR, some cells displayed a “hole” on their surface, suggestive of a leakage of intracellular material (Fig. 2, f and white arrowhead in o). Cell surface damage was also apparent after IPL 420 nm treatment (Fig. 2, narrow white arrow in i), while NIR treatment led to the appearance of large cell buds (Fig. 2, narrow white arrow in n).
Nd:YAG 1064 nm and IPL 420 nm, used alone or in combination, were highly effective against F. oxysporum biofilms, leading to a complete elimination of viable cells within biofilms (Fig. 3b, Table 1). NIR was slightly less effective than Nd:YAG 1064 nm and IPL 420 nm, but still showed a considerable decrease (92 %) in the number of viable biofilm cells (Table 1).
Discussion
In vitro assays allow cost-effective, fast, and high-throughput evaluation of treatments prior to clinical studies. To our knowledge, the model described here is the first in vitro nail biofilm model for the evaluation of novel therapy against onychomycoses caused by NDM and yeasts. Laser systems appear to be promising new treatment alternatives to traditional antifungal pharmacotherapy against onychomycosis [15]. Nd:YAG 1064 nm lasers were approved by the FDA only for nail clearance [26], and these systems have been tested in a limited number of clinical trials; therefore, it is not possible to compare their efficacy to the oral and topical drugs currently used for onychomycosis treatment [16].
Here, we show that biofilms of the pathogens C. albicans and F. oxysporum formed in vitro on human nail fragments were susceptible to both Nd:YAG (1064 nm) alone or in combination with IPL 420 nm filter and also to NIR (700–1400 nm) treatment (Figs. 1, 2, and 3). Our findings highlight the potential of an in vitro model using fungal biofilms formed in human nail fragments to test the fungicidal efficacy of laser and light treatments, both as single agents or in combination therapy. The model described here could be used for fast, high-throughput screening of potential novel laser and light therapies, as well as for standardization of laser/light parameters in the treatment of chronic onychomycoses, when conventional topical and/or systemic therapy has failed—a common scenario for NDM nail infections. Also, given that laser systems have not been approved by the FDA for use in fungal eradication, the in vitro system described here could become an important tool in the validation of laser or light treatments already used in patients, but whose fungicidal activity remains poorly characterized, undermining their full approval for use as “first-line” therapy against onychomycosis.
It is important to remember that there are no published reports on the testing of laser and light treatments against onychomycosis in systematic clinical studies (i.e., with a large number of patients, a sufficiently long follow-up, recording the rate of recurrence after therapy and, also, based on a precise definition of “cure”) [27]. Thus, our in vitro nail biofilm models could help clinicians in the determination of the ideal laser configuration and parameters to be tested in patients, in future clinical studies.
Even though dermatophytes mainly T. rubrum and T. mentagrophytes are the predominant causative agents of onychomycosis worldwide [2, 4, 5, 36], Candida spp. are more prevalent than dermatophytes in fingernail infections, being responsible for up to 75 % of cases of this type of onychomycosis [4]. Non-dermatophyte onychomycosis (including F. oxysporum infections) is more frequent in the toenails, and most common in elderly patients, in individuals with skin diseases that affect the nails or in immunocompromised patients [5, 37]. C. albicans and F. oxysporum were selected as model organisms in this work due to their well-described ability to form biofilms in vitro, using several abiotic surfaces [34, 35, 38–41] and because onychomycoses caused by NDM and yeasts are difficult to treat with conventional topic and/or oral therapy. Thus, the in vitro system described here adds to our knowledge on the potential applications of in vitro biofilm formation assays as tools in preclinical research.
Nevertheless, Paasch and colleagues [31] reported that heating of nail clippings with a 1064-nm laser did not affect C. albicans growth, while we show here that 1064 nm Nd:YAG had good fungicidal activity towards F. oxysporum, and caused a considerable reduction in the viability of C. albicans biofilm cells (Table 1). This discrepancy may be due to differences in laser parameters during application or due to the higher complexity (and increased drug resistance) of the in vivo-formed colonies studied by Paasch and co-workers [31].
On the other hand, NIR efficacy has been demonstrated in vivo in a human pilot study [17]. Also, application of femtosecond (fsec) NIR successfully inhibited the growth of T. rubrum in nail cuttings obtained from patients [42]. These results are in agreement with our data showing that NIR (700–1400 nm) has good fungicidal activity against both C. albicans and F. oxysporum nail biofilms, confirming that there is a good correlation between the results yielded by our in vitro nail biofilm model and those obtained from clinical samples.
An irradiation from blue light source (emitting wavelengths between 407 and 420 nm) reduced the number of Propionibacterium acnes in a clinical study [23], and, using an animal model of acne, Fan and co-workers [43] suggested that IPL irradiation at 420 nm may clear the skin by affecting bacterial viability and, hence, reducing local inflammatory response. Here, we demonstrate that the local “physiological hyperthermia” generated by IPL 420 nm reduced the viability of both C. albicans and F. oxysporum biofilm cells (Table 1, Fig. 3). Indeed, when compared to the other treatments tested, IPL 420 nm was as effective as Nd:YAG 1064 nm and NIR 700–1400 nm at reducing the viability of C. albicans biofilm cells and was more effective than NIR 700–1400 nm at reducing viability of F. oxysporum biofilm cells (Table 1). This is an important finding because the antifungal effects of IPL 420 and the potential of this type of light treatment against onychomycosis had not been described yet, despite its known effectiveness in the treatment of acne [22–25].
Taken together, the results described here confirm the fungicidal activity of both laser (Nd:YAG 1064 nm) and light (NIR 700–1400 nm and IPL 420 nm) therapies towards “surrogate” onychomycosis lesions represented by in vitro-formed fungal biofilms and provide strong evidence that the efficacy of laser and light treatments against onychomycosis reported in a limited number of clinical trials [14, 15, 42, 44] is indeed due to the negative effect of these therapies on fungal cell viability. It is important to emphasize that both laser and light were applied in a small fragment of nail when the in vitro model was used, and a significant loss of energy by the time the light reaches the undersurface of the nail or—more relevant for dystrophic nails—the matrix should be considered for the in vivo treatment. Although all parameters used in this work were designed based on reports of patients’ experiences in the clinic (mild discomfort and heat, but no pain with intermittent application), and the physiological temperature was respected, excessive heat and pain could represent limiting factors for some patients, and adjustments of the laser/light parameters used in vitro may be required before application in the clinical practice. Another important limitation of the laser therapy is its high costs for both clinicians (who need to acquire expensive laser systems) and for patients.
This limitation highlights the importance of in vitro models such as the one described here, which yields fungicidal activities that match more closely to those observed in the clinic, when compared to published in vitro models for laser and light therapy testing, and might represent an important tool for the initial testing, validation, and “fine-tuning” of laser and light therapies against NDM and yeast onychomycosis.
References
Murray S, Dawber R (2002) Onychomycosis of toenails: orthopaedic and podiatric considerations. Australas J Dermatol 43:105–112
Ghannoum MA, Hajjeh RA, Scher R et al (2000) A large-scale North American study of fungal isolates from nails: the frequency of onychomycosis, fungal distribution, and antifungal susceptibility patterns. J Am Acad Dermatol 43:641–648. doi:10.1067/mjd.2000.107754
Nenoff P, Krüger C, Ginter-Hanselmayer G, Tietz H-J (2014) Mycology—an update. Part 1: dermatomycoses: causative agents, epidemiology and pathogenesis. J Dtsch Dermatol Ges 12:188–212. doi:10.1111/ddg.12245
Foster K, Ghannoum M, Elewski B (2004) Epidemiologic surveillance of cutaneous fungal infection in the United States from 1999 to 2002. J Am Acad Dermatol 50:748–752
Kaur R, Kashyap B, Bhalla P (2008) Onychomycosis—epidemiology, diagnosis and management. Indian J Med Microbiol 26:108–116
De Araújo AJ, Souza MAJ, Bastos OM, de Oliveira JC (2003) Ocorrência de onicomicose em pacientes atendidos em consultórios dermatológicos da cidade do Rio de Janeiro. An Bras Dermatol 78:299–308
Jayatilake J, Tilakaratne W, Panagoda G (2009) Candidal onychomycosis: a mini-review. Mycopathologia 168:165–173. doi:10.1007/s11046-009-9212-x
Jo Siu W, Tatsumi Y, Senda H et al (2013) Comparison of in vitro antifungal activities of efinaconazole and currently available antifungal agents against a variety of pathogenic fungi associated with onychomycosis. Antimicrob Agents Chemother 57:1610–1616
Cuenca-Estrella M, Gomez-Lopez A, Mellado E et al (2006) Head-to-head comparison of the activities of currently available antifungal agents against 3,378 Spanish clinical isolates of yeasts and filamentous fungi. Antimicrob Agents Chemother 50:917–921. doi:10.1128/AAC.50.3.917
Alastruey-Izquierdo A, Cuenca-Estrella M, Monzón A et al (2008) Antifungal susceptibility profile of clinical Fusarium spp. isolates identified by molecular methods. J Antimicrob Chemother 61:805–809. doi:10.1093/jac/dkn022
Bourgeois GP, Cafardi JA, Sellheyer K, Andea AA (2010) Disseminated Fusarium originating from toenail paronychia in a neutropenic patient. Cutis 85:191–194
Burkharta CN, Burkhart CG, Gupta AK (2002) Dermatophytoma: recalcitrance to treatment because of existence of fungal biofilm. J Am Acad Dermatol 47:629–631. doi:10.1067/mjd.2002.124699
Scher RK, Tavakkol A, Sigurgeirsson B et al (2007) Onychomycosis: diagnosis and definition of cure. J Am Acad Dermatol 56:939–944. doi:10.1016/j.jaad.2006.12.019
Kimura U, Takeuchi K, Kinoshita A et al (2012) Treating onychomycosis of the toenail: clinical efficacy of the sub-millisecond 1,064 nm Nd:YAG laser using a 5 mm spot diameter. J Drugs Dermatol 11:496–504
Ortiz AE, Avram MM, Wanner MA (2013) A review of lasers and light for the treatment of onychomycosis. Lasers Surg Med 46:117–124. doi:10.1002/lsm.22211
Gupta AK, Simpson F (2012) Device-based therapies for onychomycosis treatment. Skin Ther Lett 17:4–9
Bornstein E, Hermans W, Gridley S, Manni J (2009) Near-infrared photoinactivation of bacteria and fungi at physiologic temperatures. Photochem Photobiol 85:1364–1374
Landsman A, Robbins A, Angelini P et al (2010) Treatment of mild, moderate, and severe onychomycosis using 870- and 930-nm light exposure. J Am Podiatr Med Assoc 100:166–177
Hochman L (2011) Laser treatment of onychomycosis using a novel .65 millisecond pulsed ND:YAG 1064 nm laser. J Cosmet Laser Ther 13:2–5
Vural E, Winfield HL, Shingleton AW et al (2007) The effects of laser irradiation on Trichophyton rubrum growth. Lasers Med Sci 23:349–353. doi:10.1007/s10103-007-0492-4
Meral G, Tasar F, Kocagöz S, Sener C (2003) Factors affecting the antibacterial effects of Nd:YAG laser in vivo. Lasers Surg Med 32:197–202. doi:10.1002/lsm.10128
Lee G (2012) Inflammatory acne in the Asian skin type III treated with a square pulse, time resolved spectral distribution IPL system: a preliminary study. Laser Ther 21:105–111
Kawada A, Aragane Y, Kameyama H, Sangen Y (2002) Acne phototherapy with a high-intensity, enhanced, narrow-band, blue light source: an open study and in vitro investigation. J Dermatol Sci 30:129–135
Omi T, Bjerring P, Sato S et al (2004) 420 nm intense continuous light therapy for acne. J Cosmet Laser Ther 6:156–162. doi:10.1080/14764170410023785
Gold MH, Sensing W, Biron JA (2011) Clinical efficacy of home-use blue-light therapy for mild-to moderate acne. J Cosmet Laser Ther 13:308–314. doi:10.3109/14764172.2011.630081
Gupta AK, Simpson F (2012) Medical devices for the treatment of onychomycosis. Dermatol Ther (Heidelb) 25:574–581
Nenoff P, Grunewald S, Paasch U (2013) Laser therapy of onychomycosis. J Dtsch Dermatol Ges 12:33–38. doi:10.1111/ddg.12251
Gupta AK, Simpson F (2012) Newly approved laser systems for onychomycosis. J Am Podiatr Med Assoc 102:428–430
Xu Z, Xu J, Zhuo F et al (2012) Effects of laser irradiation on Trichophyton rubrum growth and ultrastructure. Chin Med J (Engl) 125:3697–3700
Hees H, Raulin C, Baumler W (2012) Laser treatment of onychomycosis: an in vitro pilot study. J Dtsch Dermatol Ges 10:913–918
Paasch U, Mock A, Grunewald S et al (2013) Antifungal efficacy of lasers against dermatophytes and yeasts in vitro. Int J Hyperth 29:544–550
Nusbaum AG, Kirsner RS, Charles CA (2012) Biofilms in dermatology. Skin Ther Lett 17:1–5
Vila TVM, Ishida K, de Souza W et al (2012) Effect of alkylphospholipids on Candida albicans biofilm formation and maturation. J Antimicrob Chemother 68:113–125. doi:10.1093/jac/dks353
Chandra J, Kuhn DM, Mukherjee PK et al (2001) Biofilm formation by the fungal pathogen Candida albicans: development, architecture, and drug resistance. J Bacteriol 183:5385–5394. doi:10.1128/JB.183.18.5385-5394.2001
Ramage G, VandeWalle K, Wickes BL, Lopez-Ribot JL (2001) Characteristics of biofilm formation by Candida albicans. Rev Iberoam Micol 18:163–170
Faergemann J, Baran R (2003) Epidemiology, clinical presentation and diagnosis of onychomycosis. Br J Dermatol 149:1–4
Greer DL (1995) Evolving role of nondermatophytes in onychomycosis. Int J Dermatol 34:521–524
Chandra J, Patel JD, Li J et al (2005) Modification of surface properties of biomaterials influences the ability of Candida albicans to form biofilms. Appl Environ Microbiol 71:8795–8801. doi:10.1128/AEM.71.12.8795–8801.2005
Ramage G, Wickes BL, Lopez-Ribot JL (2008) A seed and feed model for the formation of Candida albicans biofilms under flow conditions using an improved modified Robbins device. Rev Iberoam Micol 25:37–40
Imamura Y, Chandra J, Mukherjee PK et al (2008) Fusarium and Candida albicans biofilms on soft contact lenses: model development, influence of lens type, and susceptibility to lens care solutions. Antimicrob Agents Chemother 52:171–182. doi:10.1128/AAC. 00387-07
Mukherjee PK, Chandra J, Yu C et al (2012) Characterization of Fusarium keratitis outbreak isolates: contribution of biofilms to antimicrobial resistance and pathogenesis. Invest Ophthalmol Vis Sci 53:4450–4457. doi:10.1167/iovs. 12-9848
Manevitch Z, Lev D, Hochberg M et al (2010) Direct antifungal effect of femtosecond laser on Trichophyton rubrum onychomycosis. Photochem Photobiol 86:476–479
Fan X, Xing Y-Z, Liu L-H et al (2013) Effects of 420-nm intense pulsed light in an acne animal model. J Eur Acad Dermatol Venereol 27:1168–1171. doi:10.1111/j.1468-3083.2012.04487.x
Kozarev J, Vizintin Z (2010) Novel laser therapy in treatment of onychomycosis. J Laser Health Acad 1:1–8
Acknowledgments
The authors thank Dr. Wanderley de Souza from the Laboratory of Cellular Ultrastructure Hertha Mayer (Federal University of Rio de Janeiro, RJ, Brazil) for providing the microscopy platform used in this work and Beatriz Bastos Fonseca for her help with SEM sample preparation. The work was supported by Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), Fundação Carlos Chagas Filho de Amparo à Pesquisa do Rio de Janeiro (FAPERJ), and Fundação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES).
Conflict of interest
None to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vila, T.V.M., Rozental, S. & de Sá Guimarães, C.M.D. A new model of in vitro fungal biofilms formed on human nail fragments allows reliable testing of laser and light therapies against onychomycosis. Lasers Med Sci 30, 1031–1039 (2015). https://doi.org/10.1007/s10103-014-1689-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-014-1689-y