Abstract
Several clinical treatments have been proposed to manage symptoms of fibromyalgia. Low-level laser therapy (LLLT) may be a useful tool to treat this dysfunction. The aim of this study was to evaluate the effects of LLLT in patients with fibromyalgia. A placebo-controlled, randomized clinical trial was carried out with 20 patients divided randomly into either an LLLT group (n = 10) or a placebo group (n = 10). The LLLT group was treated with a GaAlAs laser (670 nm, 4 J/cm2 on 18 tender points) three times a week over 4 weeks. Before and after treatment, patients were evaluated with the Fibromyalgia Impact Questionnaire (FIQ), McGill Pain Questionnaire, and visual analog scale (VAS). Data from the FIQ and McGill questionnaire for the treated and control groups were analyzed by paired t tests, and Wilcoxon tests were used to analyze data from the VAS. After LLLT or sham treatment, the number of tender points was significantly reduced in both groups (LLLT, p < 0.0001; placebo, p = 0.0001). However, all other fibromyalgia symptoms showed significant improvements after LLLT compared to placebo (FIQ, p = 0.0003; McGill, p = 0.0078; and VAS, p = 0.0020). LLLT provided relief from fibromyalgia symptoms in patients and should be further investigated as a therapeutic tool for management in fibromyalgia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fibromyalgia is defined as a noninflammatory chronic pain syndrome. Symptoms are usually manifested in the musculoskeletal system, but other systems can also be affected. Fibromyalgia is characterized by myalgia and focal muscular tenderness to palpation at multiple loci (tender points). Most patients experience fatigue accompanied by sleep and mood disorders [1–3].
Onset of symptoms typically occurs between 20 and 40 years of age. Symptoms emerge insidiously and range from localized pain, muscle spasms, and nerve irritation. Symptoms gradually spread throughout the body and can result in severe disability [4].
A systematic review found marked disagreement among rheumatologists regarding how to manage fibromyalgia. While some favored aerobic exercise and cognitive behavioral therapy, others preferred to prescribe aggressive multicomponent and pharmacological therapies [5]. However, most agreed that new therapies, especially nonpharmacological, need to be explored [6–8].
Numerous treatment strategies have been proposed to induce clinical remission. These treatments aim to eliminate tender points, restore range of motion and muscle strength, and improve quality of life and sleep [9].
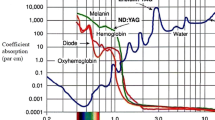
Low-level laser therapy (LLLT) may be a viable option to treat musculoskeletal disorders such as fibromyalgia. Several studies have demonstrated laser therapy to be safe and, in most cases, efficient [10–17]. Studies showed beneficial effects of 904 nm Gallium Arsenide LLLT [7, 10, 18, 19].
An analgesic effect of LLLT may be mediated by hormonal/opioid mechanisms, the responses of which depend directly on the dose and wavelength used to irradiate the tissue [20]. Thus, the parameters directly affect the results. LLLT is also reported to act on peripheral neural stimulation and the regulation of microcirculation, interrupting pain mechanisms and promoting analgesia [21]. The normalization of microcirculation and the capacity of neural transmission obtained through LLLT have been described as responsible for the interruption of the vicious circle that gives rise to and perpetuates pain [7].
However, little is known about the use of LLLT to treat fibromyalgia, and studies to investigate optimal parameters, indications, and limitations of the therapy are needed. Previous studies [18, 22–24] have used laser therapy to treat fibromyalgia, but employed different treatment regimens and parameters than this study. The goal of this study was to evaluate the ability of LLLT to relieve pain and other symptoms in patients with fibromyalgia.
Material and methods
This was a placebo-controlled, randomized clinical trial. The study was approved by the Ethics Committee of the Universidade Estadual do Oeste do Paraná (ruling number 168/2005). It adhered to Brazilian laws and guidelines concerning research in humans. Subjects signed informed consent forms.
Subjects were referred after being clinically diagnosed with fibromyalgia by a rheumatologist according to the criteria of the American College of Rheumatology (ACR) [25, 26]. Participants were excluded if they had uncontrolled diabetes, known history of cancer, and long-term corticosteroid use and if they were taking medications that caused sensitivity to light therapy.
Twenty patients were randomly divided (randomized by a free software, Research Randomizer, version 4.0, available at http://www.randomizer.org/) into two groups: a treatment laser group receiving LLLT (n = 10) and a placebo group (n = 10) that was subjected to the same procedures as the LLLT group, but received a sham laser exposure (0 W of laser power). An aluminum/gallium/arsenide (GaAlAs) diode laser (Ibramed, model Laserpulse, code 000689, serial number 1320) was used at a wavelength of 670 nm with an output of 20 mW (measured by Lasercheck, Coherent) to reduce local inflammation and assist in the tissue repair. The laser was calibrated and received a certificate of compliance (from Instituto São Paulo).
The chosen energy density of exposures was 4 J/cm2 using a beam with a focal spot area of 0.035 cm2. The exposure time at each point was 7 s. All 18 fibromyalgia tender points, according to the ACR, were irradiated. Radiation was applied at four locations around each point, with each location separated by a distance of 1 cm. The entire area encompassed by LLLT was 1 cm2 per point. Each patient received a total of 72 applications of radiation totaling 504 s (8 min and 24 s). The power density obtained was 0.57 W/cm2.
Prior to LLLT, the skin of subjects was cleaned around the 18 tender points. The laser pen was applied directly to the skin at an angle of 90°. LLLT or sham laser treatments were conducted three times a week over 4 weeks for a total of 12 treatments. Subjects were analyzed with regard to age and the number of tender points. Additionally, the impact of their fibromyalgia symptoms on quality of life and pain were assessed before and after treatment. The irradiation parameters were carefully considered and are consistent with those of previous studies [6, 27].
To assess the impact of fibromyalgia, the Brazilian version of the Fibromyalgia Impact Questionnaire (FIQ) was used. The FIQ contained 10 items: physical function (10 subitems), feel good (1 item), missed work (1 item), do job (1 item), pain (1 item), fatigue (1 item), rested (1 item), stiffness (1 item), anxiety (1 item), and depression (1 item) [28, 29].
Pain was evaluated by the McGill Pain Questionnaire [30] and visual analog scale (VAS). Parametric data from the FIQ and McGill Pain Questionnaire were analyzed by paired t tests. Nonparametric data from the VAS were analyzed by Wilcoxon tests. Data analysis was performed with GraphPad Instat (version 3.05). Differences with p values <0.05 were considered significant.
Results
The placebo group was composed of 90 % (n = 9) female subjects with a mean age of 43.4 years (range, 33–55 years). The baseline number of tender points prior to treatment was 11.8 ± 1.5. After sham treatment, the number of tender points was reduced to 10.4 ± 1.5 (p = 0.0001). The treated group (n = 10) was composed entirely of female subjects with a mean age of 39.4 years (range, 34–45 years). The number of tender points at baseline prior to treatment was 11.6 ± 2.4, which was significantly reduced to 7.3 ± 2 after LLLT (p < 0.0001).
Table 1 summarizes the FIQ results from patients who received sham (placebo) or LLLT. Pre and post-treatment scores for each criterion assessed by the FIQ are shown. For the LLLT group, all criteria of the FIQ were significantly improved after treatment, but only physical impairment and pain were significantly improved in the control group.
When the treated and control groups were compared to each other, significant improvements were observed in all FIQ criteria except for “feel good,” “difficult to work,” and “rested” (Table 2).
For the McGill Pain Questionnaire, the LLLT group had an average baseline score of 45, which improved to 32.1 after LLLT. The sham group had an average baseline score of 47.5 and a score of 42.6 after sham treatment. The average change in McGill scores before and after treatment was significantly greater in the LLLT group compared to control group (p = 0.0078). Regarding data from the VAS, the LLLT group had a median baseline score of 6.58 that improved to 4.06 after treatment. The sham group had a median baseline score of 5.81 and a score of 5.34 after sham treatment. The median change in VAS score before and after treatment was significantly greater in the LLLT group compared to the control group (p = 0.002).
Discussion
Factors such as dosimetry, light spectrum, potency, and radiation phase influenced the biomodulation of the biological responses to the phototherapy. In the present study, the irradiation parameters were carefully considered and are consistent with those of previous studies [6, 27]. The exposure time is an especially important consideration for biosafety. The energy density recommended for LLLT to promote tissue repair (increase vascularization, epithelialization, the number of fibroblasts, and collagen fibers) and pain control must be less than 5 J/cm2 because larger doses (e.g., 8.7 or 16 J/cm2) showed no improvements. The energy density used in this study was 4 J/cm2 and is consistent with previous reports [31, 32]. Doses greater than 4 J/cm2 were not used because cells absorb more energy and become incapacitated. Such doses have only been used to treat rheumatoid arthritis by inhibiting the rheumatic process [33]. In addition to tissue repair and pain control, irradiation was also accompanied by increased muscle activity and prevention of fatigue [34], but these variables were not measured in this study.
The clinical benefits of LLLT demonstrated in this study were likely the results of improvements of several factors, such as decreased pain and increased quality of life. Characteristics of connective tissue and its reorganization in fibromyalgia can also be considered. LLLT has biostimulatory effects at energy densities between 2 and 4 J/cm2, which result in increased proliferation of the connective tissue cells and neovascularization [35]. Furthermore, significant increases of collagen deposition due to angiogenesis have been observed in mice subjected to cryoinjury followed by LLLT for 7 days post-injury [36]. Fibroblasts and capillaries are present within 24 h after injury and most pronounced by 7 to 10 days. Furthermore, the initiation of the repair process occurs after 3 to 4 days [37]. In our study, the patients were treated with LLLT for 4 weeks, long enough to produce these effects. LLLT may accelerate recovery from fibromyalgia by stimulating a proinflammatory effect.
The duration of treatment for our study was consistent with that of other reports [17, 38], which demonstrated that two to three treatments per week produced beneficial responses. This fact suggests that repeated low doses of energy with time between exposures induce greater improvement than high doses of energy applied over short periods of time. This concept is especially true for connective tissue repair.
One study compared collagen in the muscle tissues of 27 patients with fibromyalgia to that of healthy subjects [39]. Less intramuscular collagen was observed in fibromyalgia patients. This situation may render the muscle of fibromyalgia patients more susceptible to microlesions and result in nonspecific signs of muscle diseases. The relationship between repetitive injury and subsequent repair is not understood, but injuries often create deposits of collagen in the interstitium of muscle. These deposits are frequently observed in fibromyalgia, especially at tender points [40].
For the Brazilian population, nine or more points of pain provide great diagnostic accuracy [3]. The patients in our study who were treated with LLLT presented with 11.6 ± 2.4 tender points before treatment. This number was reduced to 7.3 ± 2 after treatment. Considering the diagnostic criteria from the above study [3], patients in our study did not present with fibromyalgia. However, updated diagnostic criteria using a combination of scales have been proposed [41]. These criteria recommend removing tender points as a required symptom for diagnosis. Failure to present with tender points represents approximately 25 % of patients who otherwise would be diagnosed with fibromyalgia. Given the difficulty and inaccuracy in diagnosing fibromyalgia [42], it is clear that tender points should be one of several criteria evaluated to diagnose fibromyalgia. Questions in the FIQ were answered based on the activities and perceptions of the previous 7 days. Severe cases were considered those having a score ≥70 [28]. The group receiving LLLT had a mean baseline score of 67.5 ± 13.2 that was significantly reduced to 48.9 ± 7.2 after LLLT (p < 0.0001).
Pain is a multidimensional experience involving quantitative and perceptive factors that have biological, psychological, and social repercussions [43]. Chronic pain has no apparent biological function and its persistence increases the likelihoods of depression, sleep disorders, and loss of libido [44]. We used the McGill Pain Questionnaire to specifically evaluate pain. This questionnaire is the most widely used and considered the most accurate tool for qualitative and quantitative evaluation of pain [30]. Higher scores reflect greater pain with a maximum score of 78. The VAS was used as an additional resource to assess pain. In the results presented in this study, patients who received LLLT showed significant improvements in pain compared to patients receiving sham treatment (McGill, p = 0.0078; VAS, p = 0.0020). Our results substantiate other studies [7, 45] that found positive responses from treated groups. In addition to these studies, a meta-analysis has shown that laser phototherapy effectively relieves pain associated with several etiologies and could be a valuable tool for pain management [46]. Moreover, patients treated with LLLT in our study reported no side effects or complications. These reports are consistent with other studies [10, 14, 45].
One potential limitation of this study is the difficulty controlling the effects associated with the laser pen directly contacting the skin of patients in the placebo group. This contact could have therapeutic effects by stimulating the nervous system and triggering an efferent response at the contact point. This study was limited to a small number of subjects that reduces the power of statistical analysis. It is suggested to continue the study, but a longitudinal research, to identify better the factors that affect the quality of life and the functioning of these patients, and a follow-up to assess the medium and long-term effects of the intervention.
Conclusion
This study suggests that LLLT provides relief from the symptoms of fibromyalgia and could be an important therapeutic tool to lessen the impact of the disease, decrease pain, and improve quality of life for patients.
References
Wolfe F, Ross K, Anderson J, Russel IJ, Hebert L (1995) The prevalence and characteristics of fibromyalgia in the general population. Arthritis Rheum 38(1):19–28. doi:10.1002/art.1780380104
Provenza JR, Pollak DF, Martinez JE, Paiva ES, Helfenstein M, Heymann R, Matos JMC, Souza EJR (2004) Fibromialgia. Rev Bras Reumatol 44(6):443–449. doi:10.1590/S0482-50042004000600008
Haun MVA, Ferraz MB, Pollack DF (1999) Validation of the American College of Rheumatology 1990 criteria for the classification of fibromyalgia in a Brazilian population. Rev Bras Reumatol 39(4):221–230. doi:10.1590/S0482-50042006000100006
Fan PT, Blantom ME (1992) Clinical features and diagnosis of fibromyalgia. J Musculoskelet Med 9(4):24–42
Häuser W, Thieme K, Turk DC (2010) Guidelines on the management of fibromyalgia syndrome—a systematic review. Eur J Pain 14(1):5–10. doi:10.1016/j.ejpain.2009.01.006
Goldenberg DL, Burckhardt C, Crofford L (2004) Management of fibromyalgia syndrome. JAMA 292(19):2388–2395. doi:10.1001/jama.292.19.2388
Gür A, Karakoc M, Nas K, Cevik R, Sarac AJ, Ataoglu S (2002) Effects of low power laser and low dose amitriptyline therapy on clinical symptoms and quality of life in fibromyalgia: a single-blind, placebo-controlled trial. Rheumatol Int 22(5):188–193. doi:10.1007/s00296-002-0221-z
Vitorino DFM, Martins FLM, Souza AC, Galdino D, Prado GF (2004) Using SF-36 in clinical trials of fibromyalgia patients: determining minimal criterios for clinical improvement. Rev Neurociências 12(3):147–151
Souza LPM, Forgione MCR, Alves VLR (2000) The relaxation techniques in psychotherapy for patients with chronic pain: a proposal. Acta Fisiatr 7(2):56–60
Gür A, Karakoç M, Nas K, Cevik R, Nas K, Sarac AJ, Demir E (2002) Efficacy of low power laser therapy in fibromyalgia: a single-blind, placebo-controlled trial. Lasers Med Sci 17(1):57–61. doi:10.1007/s101030200010
Gür A (2006) Physical therapy modalities in management of fibromyalgia. Curr Pharm Des 12(1):29–35
Longo L, Simunovic Z, Postiglione M, Postiglione M (1997) Laser therapy for fibromyositic rheumatisms. J Clin Laser Med Surg 15(5):217–220
Marques AP, Matsutani LA, Ferreira EAG, Mendonça LLF (2002) Physical therapy in the treatment of patients with fibromyalgia: a literature review. Rev Bras Reumatol 42(1):42–48
Schochat T, Raspe H (2003) Elements of fibromyalgia in an open population. Rheumatology 42(7):829–835. doi:10.1093/rheumatology/keg199
Sprott H (2003) What can rehabilitation interventions achieve in patients with primary fibromyalgia? Curr Opin Rheumatol 15(2):145–150
Thorsen H, Gam AN, Jensen H, Højmark L, Wahlstrøm L (1991) Low energy laser treatment-effect in localized fibromyalgia in the neck and shoulder regions. Ugeskr Laeger 153(25):1801–1804
Ricci NA, Dias CN, Driusso P (2010) The use of electrothermal and phototherapeutic methods for the treatment of fibromyalgia syndrome: a systematic review. Rev Bras Fisioter 14(1):1–9. doi:10.1590/S1413-35552010000100002
Matsutani LA, Marques AP, Ferreira EA, Assumpção A, Lage LV, Casarotto RA, Pereira CAB (2007) Effectiveness of muscle stretching exercises with and without laser therapy at tender points for patients with fibromyalgia. Clin Exp Rheumatol 25(3):410–415
Armagan O, Tascioglu F, Ekim A, Oner C (2006) Long-term efficacy of low level laser therapy in women with fibromyalgia: a placebo-controlled study. J Back Musculoskelet Rehabil 19:135–140
Laakso EL (1994) Plasma ACTH and B-endorphin levels in response to low level laser therapy (LLLT) for myofascial trigger points. Laser Therapy 6:133–142. doi:10.5978/islsm.94-OR-07
Allen RJ (2006) Physical agents used in the management of chronic pain by physical therapists. Phys Med Rehabil Clin N Am 17:315–345
Panton L, Simonavice E, Williams K, Mojock C, Kim JS, Kingsley JD, McMillan V, Mathis R (2012) Effects of Class IV laser therapy on fibromyalgia impact and function in women with fibromyalgia. J Altern Complement Med. doi:10.1089/acm.2011.0398
de Carvalho PT, Leal-Junior EC, Alves AC, Rambo CS, Sampaio LM, Oliveira CS, Albertini R, de Oliveira LV (2012) Effect of low-level laser therapy on pain, quality of life and sleep in patients with fibromyalgia: study protocol for a double-blinded randomized controlled trial. Trials 13:221. doi:10.1186/1745-6215-13-221
Fernández García R, Suárez Holgado JD, Formieles Ortiz I, Zurita Ortega F, Valverde Cepeda M, Fernández Sánchez M (2011) Using a laser based program in patients diagnosed with fibromyalgia. Reumatol Clin 7(2):94–97. doi:10.1016/j.reuma.2010.01.007
Crofford LJ, Clauw DJ (2002) Fibromyalgia: where are we a decade after the American College of Rheumatology classification criteria were developed? Arthritis Rheum 46(5):1136–1138. doi:10.1002/art.10217
Wolfe F, Smythe HA, Yunus MB, Bennet RM, Bombardier C, Goldenberg DL, Tugwell P, Campbell SM, Abeles M, Clark P et al (1990) The American College of Rheumatology 1990 criteria for the classification of fibromyalgia: report of the multicentre criteria committee. Arthritis Rheum 33(2):160–172
Esper MAL, Nicolau RA, Arisawa EA (2011) The effect of two phototherapy protocols on pain control in orthodontic procedure—a preliminary clinical study. Lasers Med Sci 26(5):657–663. doi:10.1007/s10103-011-0938-6
Burckhardt CS, Clark SR, Bennett RM (1991) The Fibromyalgia Impact Questionnaire: development and validation. J Rheumatol 18(5):728–733
Marques AP, Santos AMB, Assumpção A, Matsutani LA, Lage LV, Pereira CAB (2006) Validation of the Brazilian version of the Fibromyalgia Impact Questionnaire (FIQ). Rev Bras Reumatol 46(1):24–31. doi:10.1590/S0482-50042006000100006
Teixeira MJ, Pimenta CAM (1996) Questionário de dor McGill: proposta de adaptação para a língua portuguesa. Rev Esc Enf USP 30(3):473–483
Piva JAAC, Abreu EMC, SILVA VS, Nicolau RA (2011) Effect of low-level laser therapy on the initial stages of tissue repair: basic principles. An Bras Dermatol 86(5):947–954. doi:10.1590/S0365-05962011000500013
Lins RDAU, Dantas EM, Lucena KCR, Catão MHCV, Granville-Garcia AF, Carvalho Neto LG (2010) Biostimulation effects of low-power laser in the repair process. An Bras Dermatol 85(6):849–855. doi:10.1590/S0365-05962010000600011
Ortiz MC, Carrinho PM, Santos AAS, Gonçalves RC, Parizzoto NA (2001) Laser de baixa intensidade: princípios e generalidades – parte 1. Fisioter Bras 2(4):221–240
Kelencz CA, Muñoz IS, Amorim CF, Nicolau RA (2010) Effect of low-power gallium-aluminum-arsenium noncoherent light (640 nm) on muscle activity: a clinical study. Photomed Laser Surg 28(5):647–652. doi:10.1089/pho.2008.2467
Schimitt I, Raiser AG, Graça DL, Castagna CD, Gehver C, Maiorka P (1993) The effects of laser therapy AsGa on canine tendon healing. Braz J Vet Res Anim Sci 30(2):145–149
Souza TO, Mesquita DA, Ferrari RA, Dos Santos PD, Jr CL, Bussadori SK, Fernandes KP, Martins MD (2011) Phototherapy with low-level laser affects the remodeling of types I and III collagen in skeletal muscle repair. Lasers Med Sci 26(6):803–814. doi:10.1007/s10103-011-0951-9
Tatarunas AC, Matera JMD, Dagli MLZ (1998) Clinical and anatomopathological study of cutaneous healing in domestic cat: use of low-power GAAS laser (904 nm). Acta Cir Bras 13(2). doi: 10.1590/S0102-86501998000200004
Mester E, Mester AF, Mester A (1985) The biomedical effects of laser application. Lasers Surg Med 5(1):31–39. doi:10.1002/lsm.1900050105
Gronemann ST, Ribel-Madsen S, Bartels EM, Danneskiold-Samsøe B, Bliddal H (2004) Collagen and muscle pathology in fibromyalgia. Rheumatology 43(1):27–31. doi:10.1093/rheumatology/keg452
Warhol MJ, Siegel AJ, Evans WJ, Silverman LM (1985) Skeletal muscle injury and repair in marathon runners after competition. American J Pathol 118(2):331–339
Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Katz RS, Mease P, Russell AS, Russell IJ, Winfield JB, Yunus MB (2010) The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res 62(5):600–610. doi:10.1002/acr.20140
Fitzcharles MA, Boulos P (2003) Inaccuracy in the diagnosis of fibromyalgia syndrome: analysis of referrals. Rheumatology 42(2):263–267. doi:10.1093/rheumatology/keg075
Marques AP, Rhoden L, Siqueira JO, João SMA (2001) Pain evaluation of patients with fibromyalgia, osteoarthritis, and low back pain. Rev Hosp Clin 56(1):5–10. doi:10.1590/S0041-87812001000100002
Dourado E, Fernandes TCA, Meireles JSS, Monteiro IS (2004) Dor e efeito placebo. Rev Cir Traumatol Buco-maxilo-fac 4(3):197–203
Caballero-Uribe CV, Abuchaibe I (1997) Treatment of tender points in patients with fibromyalgia syndrome (FMS) with therapeutic infrared laser ray. Arthritis Rheum 40:S44
Fulop AM, Dhimmer S, Deluca JR, Johanson DD, Lenz RV, Patel KB, Douris PC, Enwemeka CS (2010) A meta-analysis of the efficacy of laser phototherapy on pain relief. Clin J Pain 26(8):729–736. doi:10.1097/AJP.0b013e3181f09713
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ruaro, J.A., Fréz, A.R., Ruaro, M.B. et al. Low-level laser therapy to treat fibromyalgia. Lasers Med Sci 29, 1815–1819 (2014). https://doi.org/10.1007/s10103-014-1566-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-014-1566-8