Abstract
The aim of this study was to evaluate bone repair in anemic and non-anemic rats submitted or not to laser phototherapy and hydroxyapatite graft. Animals were divided in eight groups of five animals: Clot; Laser; Graft; Graft + Laser; iron deficiency anemia (IDA) + Clot; IDA + Laser; IDA + graft; IDA + graft + Laser. When appropriate irradiation with infrared laser was done during 15 days at a 48-h interval. Animals were killed at day 30; samples were analyzed by Raman spectroscopy. Three shifts were studied and statistically analyzed: ~960, ~1,070, and ~1,454 cm−1. Graft + laser showed highest ~960 peak was statistically different from all other healthy groups. No statistical difference was found between Clot and IDA + Clot in any shift. The IDA + Graft and IDA + Graft + Laser groups had low mean peak values for shifts ~960, ~1,070, and ~1,454 cm−1. The results in this study indicate that using hydroxyapatite (HA) and laser irradiation in healthy subjects is favorable to mineral deposition and bone maturation, this being of importance for some groups at risk, such as astronauts. In iron deficiency anemia cases, the use of graft, associated or not to laser irradiation, resulted in low collagen and low carbonate and phosphate HA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anemia is functionally best characterized by a hemoglobin concentration below normal and causes tissue hypoxia as a result of a low oxygen-carrying capacity of the blood. A variety of factors cause the disease, including iron deficiency; hemolysis; a decrease in the production of red blood cells; folic acid deficiency; or a combination of these [1].
The occurrence of anemia due to iron deficiency is called iron deficiency anemia (IDA). It is the most common nutritional disorder in the world, affecting infants and women in childbearing age, in communities of both developing and highly industrialized countries [2–6]. There are three stages of development of the disease: At the first stage, there is a depletion of iron; on the second, known as iron-deficient erythropoiesis, biochemical changes make the normal and regular production of hemoglobin impossible; and finally, on the third stage, there is a reduction of the level of hemoglobin causing severe imbalance of the organism [7]. The physiologic role of oxygen and blood supply on the fracture healing process has demonstrated that iron deficiency anemia could delay fracture healing [8].
The treatment of bone defects using biomaterials has been studied throughout time. Many studies have tried to develop techniques to improve the treatment of bone defects, which include the use of various types of grafts, membranes, and bone morphogenetic proteins or a combination of them [9, 10]. One of the most commonly used biomaterials is the HA (calcium HA (CHA)), which can be used isolated, associated to a membrane, or mixed to autologous bone graft. This type of biomaterial has been found to be effective in improving bone formation [9]. It is clear that the use of a graft prevents fibrosis of the lesion and also protects the cavity as a framework for the deposition of new bone [9]. Recently, it has been demonstrated that the use of phototherapy can improve bone repair [9, 11, 12] including that when associated to biomaterials [9, 10, 13–15].
Wound healing is a complex process, and several studies have reported that laser phototherapy (LPT) can biomodulate and accelerate the repair process [16–18], increasing cell proliferation and vascularization in injured tissues with a biostimulating effect on bone remodeling by modulating the initial inflammatory response and anticipating the resolution to normal conditions at the earlier periods. Parameters, however, are an important issue as regarding how much energy is necessary to reach a suitable clinical laser application to yield significant new tissue formation with higher quality of organization within a shorter time [17].
No studies, however, are found in the literature concerning the effects of LPT on grafted bone defects in iron deficiency anemia cases.
Therefore, the objective of this research is to analyze, through Raman spectroscopy, the healing of a tibial bone defect in rats suffering or not of iron deficiency anemia submitted or not to λ780 nm laser phototherapy associated or not to hydroxyapatite graft.
Material and methods
Following approval by the Animal Experimentation Ethics Committee of institutionFootnote 1, forty 21-day-old Wistar rats weighing 50 g were kept at the Animal Experimentation Laboratory of the institution in plastic cages bedded with wood chips and maintained at 20–24 °C in a day–night light cycle. Half the animals were fed with standard pelted laboratory dietFootnote 2 and had water ad libitum. The other half was fed with iron-free pelted laboratory dietFootnote 3 to induce iron deficiency anemia. After 15 days of induction, 100 μL blood was collected with EDTA to avoid coagulation and submitted to hematologic test for erythrocytes, hemoglobin (Hb), and ferritin counting. Rats with Hb under under 11 g/dL were considered anemic and those above 11 g/dL were considered normal [19].
The rats were divided in eight groups with five rats each: Clot; Laser; Graft; Graft + Laser; Iron deficiency anemia + Clot (IDA + Clot); Iron deficiency anemia + Laser (IDA + Laser); Iron deficiency anemia + Graft (IDA + Graft); Iron deficiency anemia + Graft + Laser (IDA + Graft + Laser). After regular quarantine, under intraperitoneal general anesthesia with 60 mg/kg of ketamineFootnote 4 and 10 mg/kg of xylazineFootnote 5, the dorsum of each animal was shaved and cleaned with 2 % chlorhexidine. A 2-cm-long incision was created with a no. 15 scalpel blade exposing the animal’s left tibia, and a defect (~10 mm) was created with round steel n°8 bur and a water-cooled high-speed hand piece. The bone defects in groups Clot and IDA + Clot were filled only by the blood clot. Those in groups Graft; Graft + Laser; IDA + Graft; and IDA + Graft + Laser were grafted with a 0.5 mm particle ceramic graft .Footnote 6 The animals in groups Laser; Graft + Laser; IDA + Laser; and IDA + Graft + Laser were further irradiated. Laser phototherapy (λ780 nm, 70 mW, Φ = 0.04 cm2, 4 J/cm2 per point (4 × 4), total dose 16 J/cm2, CW) started immediately after surgery and was repeated at a 48-h interval for 2 weeks (Table 1). All wounds were routinely sutured. It was requested to the manufacturer that the laser equipment used in this research be calibrated considering the area of 1 cm2 in the calculus for its supply of the energy dosage. The animals were fed the same pelted laboratory diet according to each group during the rest of the experiment. The animals were killed with an overdose of general anesthetics (ketamine and xylazine) 30 days after surgery. The tibia was removed and sliced in two halves with a diamond disc with a water-cooled high-speed hand piece. The bone was stored in a Safe-Lock micro tubeFootnote 7 and placed in liquid nitrogen. Liquid nitrogen is used to minimize bacterial growth and also because chemical fixation is not advisable due to fluorescence emissions from fixative substances [10]. Samples were analyzed by Raman spectroscopy that was carried out at the surface of the defects and also on the surface on bone without defect (basal).
Raman spectroscopy
For Raman measurements, a dispersive near-infrared Raman spectrometerFootnote 8 was used. The equipment uses a wavelength-stabilized diode laser tuned at 785 nmFootnote 9 coupled to a fiber-optic "Raman Probe"Footnote 10 in order to provide excitation of the sample and collection of the Raman spectra in repeatable excitation-collection geometry, by using an excitation fiber of 105 μm and a collecting fiber of 200 μm. The collection fiber is coupled to a dispersive spectrometer, composed of an imaging spectrograph and a back thinned, deep depletion CCD camera,Footnote 11 which disperses and detects the Raman scattered light (Fig. 1).
The Raman system was controlled by the Solis softwareFootnote 12 installed in a Windows-based microcomputer, which controls both CCD camera and spectrograph in terms of grating position, slit aperture, number of accumulations and time exposure, as well as performs the spectral calibration of the Raman shift and stores and pre-processes the spectral data [9, 14, 20–23]. The slit and grating configurations provided a spectral resolution of about 4 cm−1 in the spectral range from 400 to 1,800 cm−1. The laser power measured at the excitation tip of the Raman probe was 300 mw, and the spectral acquisition time for each collection spot was 20 s. Five points were measured at the surface of the cortical area of the defect in each one of the samples, resulting in total of 200 spectra (Fig. 1). All spectra were acquired on the same day and room conditions.
For spectrograph calibration,Footnote 13 it was used as a spectral irradiance lampFootnote 14 with known spectral curve, which has been measured with long exposure time (~10 min) and used to correct the differences in the intensity response of all optical components along the spectral range, and seven major bands of the naphthalene in the spectral region 700–1,700 cm−1, where measured pixel position and known Raman shift were fitted with a third-order polynomial and used as abscissa (x-axis) [9, 14, 20–23]. The calibration of the spectral data was performed using a routine developed under Matlab® 5.1 software.Footnote 15
Absolute peak intensities as well as their standard deviations were calculated and plotted using Microsoft Excel or Minitab software. The statistical analysis (ANOVA, general linear model) in the peak intensities was performed using Minitab 15.0® software (Minitab, Belo Horizonte, MG, Brazil). The data were initially analyzed to verify their normality. We conducted a two-way ANOVA analysis with balanced design. Predictor variables were health (non-anemic and IDA); use of phototherapy (non-irradiated and Irradiated); use of graft (non-grafted and grafted); and the use of the association of graft + laser (non-associated and associated) being in each analysis transformed into a ¨dummy variable¨ taking the non-treated as reference. All testing were conducted with a significance level of 5 %, and adequacy of the models was evaluated with the adjusted R 2.
Results and discussion
The intensity of the Raman shift at ~960, ~1,070, and ~1,454 cm−1 was obtained on bone without surgical defect for both Non-anemic and IDA groups. A statistically significant difference was observed between the mean values obtained when the groups were compared with regards all peaks (p < 0.05) but with regards the ~1,454 one (Fig. 2). This may be indicative that IDA influenced the level of mineralization on the animals suffering from the condition.
The Raman shift at ~960, ~1,070, and ~1,454 cm−1 were also analyzed in groups with surgical bone defect (healthy and anemic), and the mean peak values observed were submitted to statistical analysis for comparison. A summary of the ANOVA analysis may be seen on Table 2.
For all peaks studied on the experimental groups, significant differences on the intensities were observed between healthy and anemic animals (p < 0.05) being higher peaks observed on healthy animals. This is indicative that the IDA affected the bone quality on anemic animals. When all treatments were analyzed together (Laser/Graft/Laser + Graft), the same was seen (p < 0.05).
With regards the use of the laser light, it was found that it caused significant differences for all peaks on healthy animals (p < 0.05). However, on anemic ones, it influenced the ~1,070 and ~1,454 cm−1 peaks but not the ~960 cm−1. When using the graft, significant differences were found between the ~1,070 and ~1,454 cm−1 peaks (p < 0.05), but not for the ~960 cm−1 (p > 0.05) on both healthy and anemic animals. The use of the association only influenced the ~960 cm−1 peak on healthy animals (p = 0.001). However, on anemic animals, all peaks significantly differed (p < 0.05).
The intensity of the Raman shift at ~960 cm−1 (relative to mineral phosphate) is directly related to the concentration/incorporation of phosphate HA in the bone. Higher intensities represent higher concentrations of phosphate HA (Table 3). In this study, the mean peak values for phosphate HA (~960 cm−1) showed significant statistical difference between all healthy subjects (Clot, Laser, Graft, and Graft + Laser). Groups Graft and Graft + Laser showed high mean peak values, with group Graft + Laser presenting the highest peak. Recent reports have indicated that near-infrared laser phototherapy is effective on improving bone repair [10, 13, 17, 24, 25] especially when associated to a variety types of grafts [9, 10, 24, 26, 27], producing even better results than when laser or grafts are used alone [13, 24].
Light irradiation increases the number and activity of osteoblasts [28]. The higher number of cells results in a larger deposition of bone matrix, which later incorporates HA, characterizing maturation of the bone [28, 29]. Off all biomaterials used as grafts to improve bone healing, HA is the most investigated, and other studies have found that its association to laser irradiation enhances phosphate HA concentration [9]. It is well accepted that deposition of HA represents bone maturation, and larger amounts of HA is an indicative of a more resistant and calcified bone [9]. On the other hand, when laser was used as the unique treatment, phosphate HA concentration in the bone defect was not as high as it was when it was associated to the graft, as seen in previous studies [13, 24].
No statistical difference was found in the mean peak values for phosphate HA between group Clot and group IDA + Clot. This result was also seen in the basal healthy bone when compared with the IDA bone of specimens that were not submitted to surgical defect in this work. Even though studies have reported that iron deficiency may alter bone metabolism influencing in enzymes and intestinal calcium absorption with altered bone mineral composition and strength [30], in this study, it did not affect the bone formation process. Recent reports have demonstrated that, while severely low iron conditions inhibit osteoblast activity, mild–low iron promotes osteoblast activity [31]. In this work, the animals presented, according to blood tests, low but not severe iron depletion, which could account for the results found (Table 3).
Significant statistical difference in for phosphate HA was found between all anemic groups (IDA + Clot, IDA + Laser, IDA + Graft, and IDA + Graft + Laser). Groups IDA + Clot and IDA + Laser presented higher mean peaks, considering the other anemic group’s values, and no statistical difference was found between them. No studies using laser in IDA bone were found in the literature for comparison. A recent research that analyzed another aspect of the wound healing process in IDA animals, but using soft tissue healing as target of the study, found no influence of laser in anemia cases as to mast cell proliferation and degranulation, which are considered important on the inflammatory process. In that study, no significant difference in the number of mast cells was found following LPT when comparing anemic and healthy animals [32] (Table 3).
On the other hand, group IDA + Clot presented statistical significant difference when compared with group IDA + Graft. IDA + Clot showed also statistical difference to IDA + Graft + Laser. IDA + Graft and IDA + Graft + Laser presented lower mean peak values than group IDA + Clot. Despite that the presence of the graft is expected to facilitate the process of bone deposition, in anemic animals, it apparently delayed the process. It seems as if a “foreign body-type reaction” was produced in the presence of the graft in IDA subjects. This will be assessed in a histological study that will follow the present one. Since we were unable to find any previous reports in the literature concerning the use of grafts or laser in bone repair in iron deficiency anemia, it makes our discussion of our results very difficult in this aspect (Table 3).
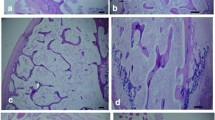
Skeletal graft incorporation is a multifaceted process in which multiple variables determine success or failure [33]. Reparative osteogenesis of bone defects may be influenced by biological factors such as the coexistence of chronic diseases such as diabetes mellitus, by the use of chemical substances such as calcitonin and bisphosphonates, or by physical procedures such as techniques for graft preparation and insertion, consequently accelerating or delaying bone repair [10]. Moreover, iron deficiency affects humoral and cell-mediated immunity, with significant lower mean levels of T lymphocytes (CD3+ and CD4+) [3, 6], IgG4 and IL-6 [6]. Perhaps the association of these factors, low immunity, and grafts presence, could have contributed to the results of IDA and Graft groups. The use of laser associated to graft in IDA animals also did not have the same influence on increasing phosphate HA deposition as it did in healthy ones. Again, the reason for this is not clear and needs clarification in a future study (Figs. 3, 4, and 5).
Significant statistical difference was found when comparing carbonate HA ~1,070 cm−1 peak between the healthy groups Clot, Laser, Graft, and Graft + Laser.
As bone maturation occurs, the carbonate-to-phosphate ratio is altered with greater level intensity of carbonate substitution in phosphate positions [34]. When analyzing the mean peak values for carbonate HA, a statistical difference was found between the healthy groups (Clot, Laser, Graft, and Graft + Laser) (Table 4). When comparing individually, groups Clot and Graft, statistical difference was found between them, with higher intensity of carbonate HA in the Clot group. Perhaps the presence of a greater concentration of phosphate HA in the graft’s composition and slow reabsorption of the graft contributed to the lesser carbonate HA level in this particular group. Furthermore, group Graft + Laser showed the lowest mean peak value for carbonate HA between all groups studied in this research. The use of laser light is known to stimulate bone maturation [10]; consequently, it could be expected to reduce carbonated HA levels when it is used. This may explain this finding.
No statistical difference was found as to carbonate HA concentrations between group Clot and IDA as well as seen in the phosphate HA concentrations. The mean peak values for carbonate HA among the anemic groups also followed similar patterns as to the results found for phosphate HA deposition in these same groups. No statistical difference was found between IDA + Clot and IDA + Laser groups. On the other hand, significant statistical difference was found between group IDA + Clot and IDA + Graft and IDA + Graft + Laser. Both anemic graft groups presented low mean peak values compared with the IDA + Clot group. Group IDA + Laser also had significant statistical difference to groups IDA + Graft and IDA + Graft + Laser. We could infer to these findings the same speculations accounted for the low mean peak values found for phosphate HA in the grafted anemic groups (Table 3).
The intensity of the Raman shift at ~1,454 cm−1 (relative to lipids and proteins) represents presence of collagen. Significant statistical difference was found between the healthy groups: Clot, Laser, Graft, and Graft + Laser (Table 5). The Laser group presented lower mean peak value. The use of laser irradiation is known to stimulate proliferation of fibroblasts that are major secretors of collagen [10, 27]. However, in an ongoing bone repair situation, collagen concentration diminishes while bone maturation advances with an increased mineral-to-matrix ratio emerging [34]. The Graft and Graft + Laser groups showed higher mean peak values for collagen than the Clot or Laser groups. Even though both graft groups had a high concentration of phosphate HA and low presence of carbonated HA indicating bone maturation, due to this high level of collagen observed, we cannot affirm with certainty if the high peak of phosphate HA found is related to a more mature bone or if the presence of the graft, which contains only inorganic components (phosphate HA), could have influenced the results of these groups.
No significant difference was obtained between groups Clot and IDA + Clot concerning collagen deposition. Recent studies in soft tissue wounds of IDA cases detected that laser phototherapy in anemic animals does stimulates fibroblastic proliferation inducing production of collagen [7]. Both grafted groups (IDA + Graft and IDA + Graft + Laser) showed lower mean peak values. Again, the presence of graft in IDA subjects apparently influences negatively bone repair. Although less collagen observed in these groups which could signal bone maturation, both IDA-grafted groups also presented low mean peaks of carbonated and phosphate HA, not compatible with bone formation and maturation.
It is important to remember that the natural processes of repair should be allowed to take their usual course, and any interference should only be attempted when there is a demonstrable need or substantial advantage for the patient [10, 14]. In this study, the highest mineral concentration was observed associating graft and laser on both healthy and anemic animals. What is clinically important in this study is that it evidenced that the association of the two treatments on anemic animals caused similar results to the one observed on healthy ones.
Finally, it is important to remember that low-level (low intensity) laser irradiation is accepted to induce an acceleration of wound healing processes, to reduce inflammations, to support neuro-regeneration, to promote vascular and lymphatic microcirculation, to stimulate the immune system, and to reduce pain nonthermal radio-biological therapeutic effects relevant for civilians, military personnel, and astronauts [35].
Conclusion
The results in this study indicate that, in healthy situations, the use of HA graft associated to laser irradiation produced favorable outcomes regarding mineral deposition and bone maturation. Iron deficiency anemia did not significantly affect bone mineralization. However, the use of graft, without or with laser, in iron deficiency anemia cases resulted in low concentrations of collagen and low carbonate and phosphate HA.
Notes
Protocol no05/10
Labina®, Purina, São Paulo Brazil
AIN93-G iron-free, São Paulo, Brazil
Vetaset®, São Paulo, SP, Brazil
Coopazine®, Cooper, Brazil
GenPhos® HATCP.BAUMER®; Mogi Mirim, São Paulo, Brazil
Eppendorf®, Brazil
Andor Technology, model Shamrock SR-303i®, Belfast, Northern Ireland
B&W TEK, model BRM-785-0.30-100-0.22.s, Newark, DE, USA
B&W TEK, model BAC-100-785, Newark, DE, USA
Andor Technology, model IDUs® DU401A-BR-DD, Belfast, Northern Ireland, 1,024 × 128 pixels, Peltier-cooled down to -70 °C
Andor Technology, Solis (i) software, Belfast, Northern Ireland
Intensity correction and wavenumber calibration.
Oriel Instruments, model 63358, Strattford, CT, USA
The Mathworks, Newark, NJ, USA
References
Gorustovich AA, Steimetz T, Giglio MJ, Guglielmotti MB (2006) A histomorphometric study of alveolar bone modeling and remodeling under experimental anaemia and polycythaemia in rats. Arch Oral Biol 51:246–251
Killip S, Bennett JM, Chambers MD (2007) Iron deficiency anemia. Am Fam Physician 75:671–678
Mullick S, Rusia U, Sikka M, Faridi M (2006) Impact of iron deficiency anaemia on T lymphocytes & their subsets in children. Indian J Med Res 124:647–654
Coutinho GG, Goloni-Bertolo EM, Bertelli EC (2005) Iron deficiency anemia in children: a challenge for public health and for society. Sao Paulo Med J 123:88–92
Benoist B, McLean E, Egli I, Cogswell M. Worldwide prevalence of anaemia 1993–2005: WHO global database on anaemia (2012) Geneva: WHO Press. http://www.who.int/nutrition/publications/en. Accessed 12 December 2012
Ekiz C, Agaoglu L, Karakas Z, Gurel N, Yalcin I (2005) The effect of iron deficiency anemia on the function of the immune system. Hematol J 5:579–583
Sampaio SC, Monteiro JS, Cangussu MC, Pires Santos GM, Dos Santos MA, Dos Santos JN, Pinheiro AL (2012) Effect of laser and LED phototherapies on the healing of cutaneous wound on healthy and iron-deficient Wistar rats and their impact on fibroblastic activity during wound healing. Lasers Med Sci. doi:10.1007/s10103-012-1161-9
Heppenstall R, Bruce MD, Brighton CT (1977) Fracture healing in the presence of anemia. Clin Orthop Relat Res 123:253–258
Pinheiro AL, Santos NR, Oliveira PC, Aciole GT, Ramos TA, Gonzales TA, da Silva LN, Barbosa AF, Junior LS (2013) The efficacy of the use of IR laser phototherapy associated to biphasic ceramic graft and guided bone regeneration on surgical fractures treated with miniplates: a Raman spectral study on rabbits. Lasers Med Sci 28:513–518
Pinheiro AL, Soares LG, Aciole GT, Correia NA, Barbosa AF, Ramalho LM, Dos Santos JN (2011) Light microscopic description of the effects of laser phototherapy on bone defects grafted with mineral trioxide aggrerate, bone morphogenetic proteins, and guided bone regeneration in a rodent model. J Biomed Mater Res A 98:212–221
Demir H, Menku P, Kirnap M, Ikizceli I (2004) Comparison of the effects of laser, ultrasound, and combined laser + ultrasound treatments in experimental tendon healing. Lasers Surg Med 35:84–89
Medrado AP, Pugliese LS, Reis SR, Andrade ZA (2003) Influence of low level laser therapy on wound healing and its biological action upon myofibroblasts. Lasers Med Sci 32:239–244
Rosa AP, Sousa LG, Regalo SC, Issa JP, Barbosa AP, Pitol DL, de Oliveira RH, de Vasconcelos PB, Dias FJ, Chimello DT, Siéssere S (2012) Effects of the combination of low-level laser irradiation and recombinant human bone morphogenetic protein-2 in bone repair. Lasers Med Sci 27:971–977
Lopes CB, Pacheco MT, Silveira Junior L, Cangussu MC, Pinheiro AL (2010) The effect of the association of near infrared laser therapy, bone morphogenetic proteins, and guided bone regeneration on tibial fractures treated with internal rigid fixation: a Raman spectroscopic study. J Biomed Mater Res A 94:1257–1263
Torres CS, Santos JN, Monteiro JS, Amorim PG, Pinheiro AL (2008) Does the use of laser photobiomodulation, bone morphogenetic proteins, and guided bone regeneration improve the outcome of autologous bone grafts? An in vivo study in a rodent model. Photomed Laser Surg 26:371–377
Tajali SB, Dermid JC, Houghton P, Grewal R (2010) Effects of low power laser irradiation on bone healing in animals: a meta-analysis. J Orthop Surg Res 5:1–10
Pretel H, Lizarelli RF, Ramalho LT (2007) Effect of low-level laser therapy on bone repair: histological study in rats. Lasers Surg Med 39:788–796
Luger EJ, Rochkind S, Wollman Y, Kogan G, Dekel S (1998) Effect of low-power laser irradiation on the mechanical properties of bone fracture healing in rats. Lasers Surg Med 22:97–102
Chhabra D, Grafals M, Skaro AI, Parker M, Gallon L (2008) Impact of anemia after renal transplantation on patient and graft survival and on rate of acute refection. Clin J Am Soc Nephrol 3:1168–1174
Pinheiro AL, Aciole GT, Cangussú MC, Pacheco MT, Silveira L Jr (2010) Effects of laser phototherapy on bone defects grafted with mineral trioxide aggregate, bone morphogenetic proteins, and guided bone regeneration: a Raman spectroscopic study. J Biomed Mater Res A 95(4):1041–1047
Timlin JA, Carden A, Morris MD (1999) Chemical microstructure of cortical bone probed by Raman transects. Appl Spectrosc 53(11):1429–1435
Carvalho FB, Aciole GT, Aciole JM, Silveira-Junior L, Santos JN, Pinheiro AL (2001). Assessment of bone healing on tibial fractures treated with wire osteosynthesis associated or not with infrared laser light and biphasic ceramic bone graft (HATCP) and guided bone regeneration (GBR): Raman spectroscopy study. Proceedings–SPIE 7887:7887OT-1-7887OT-6
Pinheiro AL, Lopes CB, Pacheco MT, Brugnera A, Zanin FA, Cangussú MC, Silveira-Junior L (2010) Raman spectroscopy validation of DIAGNOdent-assisted fluorescence readings on tibial fractures treated with laser phototherapy, BMPs, guided bone regeneration and miniplates. Photomed Laser Surg 28:89–97
Denadai AS, Carvalho PT, Reis FA, Belchior AC, Pereira DM, Dourado DM, Silva IS, de Oliveira LV (2009) Morphometric and histological analysis of low-power laser influence on bone morphogenetic protein in bone defects repair. Lasers Med Sci 24:689–695
Nicolau RA, Jorgetti V, Rigau J, Pacheco MT, dos Reis LM, Zângaro RA (2003) Effect of low-power GaAlAs laser (660 nm) on bone structure and cell activity: an experimental animal study. Lasers Med Sci 18:89–94
Pinheiro AL, Santos NR, Oliveira PC, Aciole GT, Ramos TA, Gonzalez TA, da Silva LN, Barbosa AF, Silveira L Jr (2012) The efficacy of the use of IR laser phototherapy associated to biphasic ceramic graft and guided bone regeneration on surgical fractures treated with wire osteosynthesis: a comparative laser fluorescence and Raman spectral study on rabbits. Lasers Med Sci. doi:10.1007/s10103-012-1166-4
Pinheiro AL, Soares LG, Cangussu MC, Santos NR, Barbosa AF, Silveira Junior L (2012) Effects of LED phototherapy on bone defects grafted with MTA, bone morphogenetic proteins and guided bone regeneration: a Raman spectroscopic study. Lasers Med Sci 5:903–916
Pinheiro ALB, Gerbi ME (2006) Photoengineering of bone repair processes. Photomed Laser Surg 24:169–178
Stein A, Benayahu D, Maltz L, Oron U (2005) Low-level laser irradiation promotes proliferation and differentiation of human osteoblasts in vitro. Photomed Laser Surg 23:161–166
Lobo AR, Gaievski EHS, Colli C (2011) Hemoglobin regeneration efficiency in anemic rats: effects on bone mineral composition and biomechanical properties. Biol Trace Elem Res 143:403–411
Zhao G, Zhao L, He Y, Li GF, Gao C, Li K, Xu YJ (2012) A comparison of the biological activities of human osteoblast hFOB1.19 between iron excess and iron deficiency. Biol Trace Elem Res 150:487–495
Rosa CB, Sampaio SC, Monteiro JS,Ferreira MF, Zanini FA, Santos JN, Cangussu MC, Pinheiro AL (2011) Influence of laser and LED irradiation on mast cells of cutaneous wounds of rats with iron deficiency anemia. Proc. of SPIE 7887: 7887OS-1-7887OS-6
Shegarfi H, Reikeras O (2009) Review article: bone transplantation and immune response. J Orthop Surg 17:206–211
Morris MD, Mandair GS (2011) Raman assessment of bone quality. Clin Orthop Relat Res 469:2160–2169
Mester AR, and Sommer AP (2002) How It All Started: Dr. Endre Mester’s Pioneering Work. Proceedings of the Second International Conference on Near-field optical analysis, photodynamic therapy & photobiology effects, Houston, Texas, USA, May 31–June 1, 2001 (Nasa/CP-2002-210786)
Acknowledgments
We would like to thank the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) for providing financial support for this project.
Conflicts of interest
The authors received a grant from Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), a government research agency, but have full control of all primary data and agree to allow the journal to review their data if requested.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rosa, C.B., de Castro, I.C.V., Júnior, J.A.R. et al. The efficacy of the use of IR laser phototherapy (LPT) on bone defect grafted with biphasic ceramic on rats with iron deficiency anemia: Raman spectroscopy analysis. Lasers Med Sci 29, 1251–1259 (2014). https://doi.org/10.1007/s10103-013-1496-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-013-1496-x








