Abstract
The objective of this study was to investigate the effect of Er:YAG laser irradiation on shear bond strength and microleakage between resin cements and yttrium-stabilized tetragonal zirconia (Y-TZP) ceramics. Eighty disc specimens of Y-TZP ceramics (6 mm × 4 mm) were prepared. The specimens were divided into two groups according to surface treatment (control and Er:YAG laser-treated). The control and lased specimens were separated into two groups for shear bond strength test (n = 20), and microleakage evaluation (n = 10). Specimens were subjected to shear bond strength test by a universal testing machine with a crosshead speed of 1 mm/min. Specimens for microleakage evaluation were then sealed with nail varnish, stained with 0.5% basic fuchsin for 24 h, sectioned, and evaluated under a stereomicroscope. The data were analyzed with one-way ANOVA and post hoc Tukey-Kramer multiple comparisons tests (α = 0.05) for shear bond strengths and a two related-samples tests (α = 0.05) for microleakage scores. Higher bond strength values were found in the laser-treated groups compared to the control groups. Microleakage scores among the groups showed that the laser-treated specimens had lower microleakage scores than those of control specimens in the adhesive-ceramic interface. Roughening surface of Y-TZP ceramic by Er:YAG laser increased the shear bond strengths of ceramic to dentin and reduced the microleakage scores.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Advanced ceramic materials such as zirconia have great potential as substitutes for traditional materials in many dental applications including orthodontic brackets, posts, implant abutments, and frameworks for inlays, crowns, and bridges [1]. The mechanical properties of zirconia are the highest ever reported for any dental ceramic with a high flexural strength and toughness [2–4]. This may allow the realization of posterior fixed partial dentures and permit a substantial reduction in core thickness. These capabilities are highly attractive in prosthetic dentistry, where strength and esthetics are paramount [5]. In addition, the development of new technology, such as computer-aided design/computer aided manufacturing (CAD/CAM), allows the fabrication of zirconia-based restorations for all-ceramic crowns (or fixed partial dentures) to be more a practical process [4].
Zirconia is a well-known polymorph that occurs in three forms: monoclinic (m), cubic (c), and tetragonal (t). Pure zirconia is monoclinic at room temperature and pressure. This phase is stable up to 1,170°C. Above this temperature it transforms into tetragonal and then into cubic phase at 2,370°C [5–7]. The remarkable mechanical properties of zirconia, already exploited in several medical and engineering applications, are mainly due to the tetragonal to monoclinic (t → m) phase transformation [2]. External stresses such as sandblasting, grinding, impact, and thermal aging can trigger t → m phase transformation [8]. Although many types of zirconia-containing ceramic systems are currently available, only three are used to date in dentistry. These are yttrium-stabilized tetragonal zirconia polycrystals (Y-TZP), magnesium cation-doped partially stabilized zirconia (Mg-PSZ), and zirconia-toughened alumina (ZTA) [5]. The mechanical properties of Y-TZP ceramics, such as flexural and fracture resistance, are considerably higher than those of other dental ceramics [1]. The flexural resistance of Y-TZP ceramics can reach values from 700 to 1,200 MPa [1, 3, 9]. These values exceed the maximal occlusal loads during normal chewing [9]. Y-TZP ceramics might also exhibit fracture resistance higher than 2,000 N, which is almost twice the value obtained for alumina-based materials and at least three times the value demonstrated by lithium disilicate-based ceramics [1].
Glass structure in ceramics reacts with moisture from saliva. This causes the subcritical crack propagation and stress corrosion, leading to decomposition of the glass structure and impairment of long-term stability of the ceramics. However, zirconia cores are composed of glass-free, polycrystalline microstructure, and consequently show off outstanding long-term stability [10]. Although improved mechanical properties are important, long-term retention of the restoration depends primarily on the strength and durability of the bond of the luting composite resin to the tooth and the porcelain substrates to prevent fracture, marginal discoloration, and secondary caries [11]. One of the problems is the inferior adhesion capability of resin cements to such ceramics. This is related to glass-free composition structure, characterizing zirconia as an acid-resistant material [10]. Hydrofluoric etching and silanization, which enhances the resin bond to conventional silica-based ceramics, does not improve the resin bond strength to Y-TZP ceramics [12]. For this reason, there have been considerable efforts by many researchers to modify the surface properties of zirconia, mechanically and chemically, by various surface treatments [10, 13]. Several techniques, especially the airborne particle abrasion with alumina [10], silica coating, and various adhesive monomer and metal primers [10] have been reported to facilitate the bond strength between resin cement and Y-TZP ceramic.
On the other hand, interactions at the cement-ceramic transition may also influence the bonding between cement and tooth. This transition is particularly sensitive, as insufficient sealing may allow the penetration of bacteria. Under clinical conditions, the continuing decrease of marginal adaptation may culminate in a loss of the restoration due to microleakage and resulting secondary caries [14, 15]. Therefore, there is a continuing search for materials and techniques that minimize potential for microleakage. In dentistry, laser technology is one of the last developments that may have an impact on the reduction of microleakage [16]. Recently, lasers have been shown to provide a relatively safe and easy means of altering the surface of materials. Together with reducing microleakage, they have been used to etch metals before the application of porcelain [17], Y-TZP ceramic for improving surface roughness [1], and for processing dental materials, especially for fusing the materials on or into tooth surfaces [13].
The purpose of this study was to investigate the effect of Er:YAG laser irradiation on shear bond strength and microleakage between resin cements and Y-TZP ceramics. The null hypothesis was that the shear bond strength and microleakage score obtained after Er:YAG laser treatment of Y-TZP ceramic is similar to the one obtained in untreated ceramic.
Materials and methods
Sixty human maxillary first molar teeth free of caries, cracks, fractures, and restoration and measuring approximately 9 mm in mesiodistal length were selected. After extraction, the teeth were cleaned of surface debris and stored in 0.1% thymol solution for less than 6 months. The teeth were sectioned 3 mm below the occlusal surfaces with a slow-speed diamond saw sectioning machine (Isomet, Buehler Ltd., Lake Bluff, IL). The teeth were then lowered in a metal ring and positioned in the center of the ring with the buccal cementoenamel junction 3 mm above the top of the metal mounting ring. The ring was then filled with autopolymerizing acrylic resin (Meliodent, Bayer Dental Ltd., Newbury, UK). Sixty dentin specimens were obtained in this manner and stored in distilled water at 37°C.
Sixty commercially available Y-TZP core materials (Zirkonzahn, Zirkonzahn GmbH, Bruneck, Italy) were selected for this study. Disc-shaped specimens were made of (6 mm in diameter and 4 mm in thickness) by an authorized dental laboratory according to the manufacturer's recommendations. Specimens were randomly separated into two groups (n = 30), according to the surface treatments applied.
Group 1—untreated (control): No treatment was applied to the acrylic resin specimen surfaces, this group served as a control.
Group 2—Er:YAG laser irradiated: Bonding surfaces of specimens were irradiated by Er:YAG laser (Smart 2940D Plus, Deka Laser, Florence, Italy). Laser energy was delivered in pulse mode with a wavelength of 2.94 μm at 150 mJ, 10 Hz, 1 W, and long pulse (LP) for 20 s. Water irrigation was used during the lasing of the samples.
Following the surface treatments, Y-TZP disc-shaped specimens were cemented (NX3, Kerr Co., Orange, CA) onto the dentin specimens according to the manufacturer's recommendations. The ceramic discs were positioned and stabilized on the dentin surface and excess cement was removed using a microbrush. The control and lased specimens were separated into two groups for shear bond strength test (n = 20), and microleakage evaluation (n = 10).
Shear bond strength test
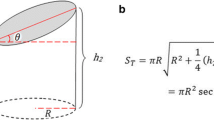
Shear bond strength specimens were stored in distilled water at 37°C for 1 week. The specimens were mounted in the custom jig of a universal testing machine (Lloyd LF Plus, Ametek Inc, Lloyd Instruments, Leicester, UK), and load was applied to the adhesive interface at a constant crosshead speed of 1 mm/min until failure occurred. The maximum force to produce fracture was recorded and the bond strength (S) values (expressed in MPa) were calculated using the formula:
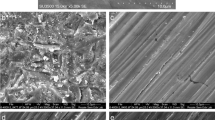
where F is the force (in N) and A is the adhesive area (in mm2). In addition, the adhered surfaces for each group were examined by scanning electron microscope (SEM, LEO 440, Zeiss, Oberkochen, Germany). Representative specimens were photographed at 1000x magnification. SEM micrographs of the Er:YAG laser-treated and control group specimens are presented in Figs. 1 and 2. The mean value and standard deviation of the specimens were statistically evaluated by two related-samples tests (α = .05).
Microleakage evaluation
Two consecutive layers of nail varnish were applied to the entire surface of the tooth, except for an area approximately 1 mm away from the ceramics. The teeth were immersed in 0.5% solution of basic fuchsin for 24 h at room temperature. After rinsing with distilled water, the samples were air-dried and each specimen was sliced longitudinally with a low-speed diamond saw (Isomet, Buehler, Lake Bluff, IL) under water coolant in the buccolingual direction. All sections were examined by two calibrated investigators with a stereomicroscope (40 × magnifications) (SMZ 800, Nikon, Tokyo, Japan) for dye penetration. Each section was scored for microleakage at the incisal and gingival levels along both interfaces (ceramic-adhesive interface and adhesive-dentin interface). Scoring was made according to the following criteria [18]:
-
Score 0: No dye penetration between the ceramic-adhesive or adhesive-dentin interface.
-
Score 1: Dye penetration restricted to 1 mm of the ceramic-adhesive or adhesive-dentin interface.
-
Score 2: Dye penetration into the inner half (2 mm) of the ceramic-adhesive or adhesive-dentin interface.
-
Score 3: Dye penetration into 3 mm of the ceramic-adhesive or adhesive-dentin interface.
In cases of disagreement between scoring, consensus was obtained by using the greater score. Figure 3 demonstrates individual examples of scoring. Statistical evaluation of microleakage scores was subjected to one-way ANOVA and among the test groups was performed by Kruskal-Wallis test with significance set at p = 0.05.
Results
Two related-samples tests results for shear bond strength measurements of the groups are summarized in Table 1. Laser-treated specimens demonstrated higher bond strength values compared to untreated control specimens, and differences in bond strength between laser-treated and control groups were found to be statistically significant (p = 0.002).
Statistical results of the one-way ANOVA for microleakage scores of the groups are summarized in Table 2 (df = 3, MS = 4.092, F = 6.851, p < 0.05). Microleakage scores among the groups showed that laser-treated specimens had lower microleakage score than those of control specimens in the adhesive-ceramic interface. A statistically significant difference in shear bond strength was found between laser treated group and control group (p < 0.05). In addition, in microleakage analysis, no significant differences were found among the groups in dentin-adhesive interface (p = 0.991).
On the other hand, it can be seen that the morphology of the Er:YAG laser-treated specimen appears to be increased in roughness (Figs. 1 and 2). Er:YAG laser application resulted in irregularities on the surface of Y-TZP ceramic. In addition, it can be seen that untreated specimens showed more flat surfaces than laser-treated specimens.
Discussion
The results of the present study support rejection of the hypothesis because altering the Y-TZP ceramic surface by Er:YAG laser significantly increased the shear bond strengths of ceramic to dentin and reduced microleakage scores. This result is in accordance with the study of Cavalcanti et al. [1] who compared the surface treatments (lasing and air abrasion with Al2O3 particles), and metal primer application of Y-TZP ceramics. Consistent with the present study, Ersu et al. [13] found that CO2 laser irradiation demonstrated higher bond strengths compared to other surface treatments (control, sandblasted, and hydrofluoric acid-etched) applied on In-Ceram Zirconia and Gokce et al. [19] suggested the use of erbium:yttrium-aluminum-garnet (Er:YAG) laser to enhance the bond strength of adhesive materials to resin composites used for indirect restorations and Lithia-based ceramics. On the other hand, only a few studies have been conducted on laser treatment of Y-TZP ceramic. However, researchers have worked on increasing surface roughness of titanium by laser treatment. Watanabe et al. [20] advocated that the neodymium:yttrium–aluminum-garnet (Nd:YAG) laser treatment significantly improved the mechanical properties of cast titanium. Kim and Cho [21] found that laser etching of titanium surfaces using an Nd:YAG laser was effective in improving bond strength with low-fusing porcelain, as compared to acid-etching and machining surface treatment methods. In addition, Gaggl et al. [22] suggested that laser processing is a new method of treating implant surfaces to produce a high degree of purity with adequate surface roughness, in comparison with other surface treatments. Moreover, Cho and Jung [23] reported that laser etching is an effective method for producing an appropriate surface roughness for titanium. Results of the present study were consistent with Watanabe et al. [20], Kim and Cho [21], Gaggl et al. [22], and Cho and Jung [23].
Different levels of Er:YAG laser energy were used by researchers [24–27]. In addition, de Oliveira Ortolan et al. [27] reported that setting 160 mJ and 2 Hz promoted a good ablation rate with fewer surface alterations in primary dentine. On the other hand, the fact that both sandblasting and metal primers influence the bond strength of dental ceramics has been demonstrated in previous studies [1, 10, 12]. However, airborne particle abrasion and mechanical grinding have the possibility to create subcritical microcracks and phase transformation within the zirconia surface, consequently causing unfavorable changes of superior mechanical properties of zirconia ceramics [8, 10]. In addition, the mechanical properties of Y-TZP ceramics can be negatively affected by changes in temperature, which can induce phase transformation [1]. Higher laser power settings (400 and 600 mJ) cause excessive material deterioration, making them unsuitable as surface treatments for zirconia surfaces [28]. Hence, in the present study, a lower power setting for the Er:YAG laser was selected in accordance with the results of preliminary investigation and the surfaces were irradiated with constant water cooling. Microcracks were not observed in SEM micrographs of the Er:YAG laser-treated ceramic. Furthermore, the results of the shear bond test can suggest that the laser treatment does not induce any internal weakening of the ceramic.
The shear bond test is one of the most commonly used bond strength tests. Shear stresses are believed to be major stresses involved in in vivo bonding failures of restorative materials [13]. Hence, the shear bond test was used in the present study to evaluate the bond strength of Y-TZP ceramics with modified surface to dentin.
Moreover, modes of failure were assessed. Both the control and Er:YAG laser-treated groups had a tendency to fail at the zirconia ceramic–resin cement interface, and most portions of their surface areas were free of cement. Control-group specimens were predominated in adhesive failures between ceramic and cement (90%) and they also presented mixed failures (10%). However, 100% of the adhesive failures between ceramic and cement were seen in Er:YAG laser-treated specimens. These results are in accordance with those of Cavalcanti et al. [1] and Yun et al. [10].
In restorative dentistry, microleakage is the seeping and leaking of fluids and bacteria between the tooth and the restoration junction and interface. Microleakage increases the likelihood of recurrent caries and postoperative sensitivity. In the present study, basic fuchsin was used to detect microleakage. Different methods have been employed to disclose microleakage of which dye leakage is probably the most common. The principal advantages of this technique are its low cost and ease of application [16]. However, previous studies compared only the shear bond strength of laser irradiation with other surface treatments. There were only a few studies about the effects of lasers on microleakage of the restorations in the literature. Obeidi et al. [15] stated that the level of microleakage was significantly less in laser-treated cavities compared to non-lased cavities. Moreover, Siso et al. [16] reported that the use of pulsed KTP laser energy showed a decrease in microleakage around the restorations. However, Navarro et al. [29] demonstrated that laser irradiation used for cavity preparation with Er:YAG has no influence on microleakage. In addition, Aranha et al. [30] advocated that the cavity preparation method (Er:YAG laser and bur preparation) did not influence the levels of microleakage of the resin composite restorations. In the present study, microleakage scores among the groups showed that laser-treated specimens had lower microleakage scores than those of control specimens in the adhesive-ceramic interface. These results contradict those of Navarro et al. [29] and Aranha et al. [30] but were consistent with those of Obeidi et al. [15], and Siso et al. [16].
Conclusions
Within the limitations of this study, Er:YAG laser surface treatment of Y-TZP ceramic resulted in higher mean tensile bond strengths than those of control specimens. Moreover, Er:YAG laser surface treatments were found effective for decreasing microleakage in the adhesive-ceramic interface.
References
Cavalcanti AN, Foxton RM, Watson TF, Oliveira MT, Giannini M, Marchi GM (2009) Bond strength of resin cements to a zirconia ceramic with different surface treatments. Oper Dent 34(3):280–287
Guazzato M, Albakry M, Ringer SP, Swain MV (2004) Strength, fracture toughness and microstructure of a selection of all-ceramic materials. Part II. Zirconia-based dental ceramics. Dent Mater 20:449–456
Yilmaz H, Aydin C, Gul BE (2007) Flexural strength and fracture toughness of dental core ceramics. J Prosthet Dent 98:120–128
Chaiyabutr Y, McGowan S, Phillips KM, Kois JC, Giordano RA (2008) The effect of hydrofluoric acid surface treatment and bond strength of a zirconia veneering ceramic. J Prosthet Dent 100:194–202
Denry I, Kelly JR (2008) State of the art of zirconia for dental applications. Dent Mater 24:299–307
Kelly JR, Denry I (2008) Stabilized zirconia as a structural ceramic. An overview. Dent Mater 24:289–298
Piconi C, Maccauro G (1999) Zirconia as a ceramic biomaterial. Biomaterials 20:1–25
Karakoca S, Yilmaz H (2009) Influence of surface treatments on surface roughness, phase transformation, and biaxial flexural strength of Y-TZP ceramics. J Biomed Mater Res B Appl Biomater 91B:930–937
Papanagiotou HP, Morgano SM, Giordano RA, Pober R (2006) In vitro evaluation of low-temperature aging effects and finishing procedures on the flexural strength and structurel stability of Y-TZP dental ceramics. J Prosthet Dent 96(3):154–164
Yun JY, Ha SR, Lee JB, Kim SH (2010) Effect of sandblasting and various metal primers on the shear bond strength of resin cement to Y-TZP ceramic. Dent Mater 26(7):650–658
Ayad MF, Fahmy NZ, Rosenstiel SF (2008) Effect of surface treatment on roughness and bond strength of a heat-pressed ceramic. J Prosthet Dent 99:123–130
Kern M, Wegner SM (1998) Bonding to zirconia ceramic: adhesion methods and their durability. Dent Mater 14:64–71
Ersu B, Yuzugullu B, Yazici AR, Canay S (2009) Surface roughness and bond strengths of glass-infiltrated alumina-ceramics prepared using various surface treatments. J Dent 37:848–856
Rosentritt M, Behr M, Kolbeck C, Handel G (2007) Marginal integrity of CAD/CAM fixed partial dentures. Eur J Dent 1(1):25–30
Obeidi A, Ghasemi A, Azima A, Ansari G (2005) Effects of pulsed Nd:YAG laser on microleakage of composite restorations in Class V cavities. Photomed Laser Surg 23(1):56–59
Siso HS, Kustarci A, Göktolga EG (2009) Microleakage in resin composite restorations after antimicrobial pre-treatments: effect of KTP laser, chlorhexidine gluconate and Clearfil Protect Bond. Oper Dent 34(3):321–327
Jacobsen NL, Mitchell DL, Johnson DL, Holt RA (1997) Lased and sandblasted denture base surface preparations affecting resilient liner bonding. J Prosthet Dent 78:153–158
Arhun N, Arman A, Cehreli SB, Arikan S, Karabulut E, Gulsahi K (2006) Microleakage beneath ceramic and metal brackets bonded with a conventional and an antibacterial adhesive system. Angle Orthod 76:1028–1034
Gokce B, Ozpinar B, Dundar M, Comlekoglu E, Sen BH, Gungor MA (2007) Bond strengths of all-ceramics: Acid vs laser etching. Oper Dent 32(2):173–178
Watanabe I, McBride M, Newton P, Kurtz KS (2009) Laser surface treatment to improve mechanical properties of cast titanium. Dent Mater 25(5):629–633
Kim JT, Cho SA (2009) The effects of laser etching on shear bond strength at the titanium ceramic interface. J Prosthet Dent 101(2):101–106
Gaggl A, Schultes G, Müller WD, Kärcher H (2000) Scanning electron microscopical analysis of laser-treated titanium implant surfaces–a comparative study. Biomaterials 21:1067–1073
Cho SA, Jung SK (2003) A removal torque of the laser-treated titanium implants in rabbit tibia. Biomaterials 24:4859–4863
Korkmaz Y, Ozel E, Attar N, Bicer CO, Firatli E (2010) Microleakage and scanning electron microscopy evaluation of all-in-one self-etch adhesives and their respective nanocomposites prepared by erbium:yttrium-aluminum-garnet laser and bur. Lasers Med Sci 25(4):493–502
Chousterman M, Heysselaer D, Dridi SM, Bayet F, Misset B, Lamard L, Peremans A, Nyssen-Behets C, Nammour S (2010) Effect of acid etching duration on tensile bond strength of composite resin bonded to erbium:yttrium–aluminium–garnet laser-prepared dentine. Preliminary study. Lasers Med Sci 25(6):855–859
Gurgan S, Kiremitci A, Cakir FY, Yazici E, Gorucu J, Gutknecht N (2009) Shear bond strength of composite bonded to erbium:yttrium-aluminum-garnet laser-prepared dentin. Lasers Med Sci 24:117–122
de Oliveira Ortolan AS, Torres CP, Gomes-Silva JM, de Menezes-Oliveira MA, Pécora JD, Palma-Dibb RG, Borsatto MC (2009) Effect of erbium-doped yttrium aluminium garnet laser parameters on ablation capacity and morphology of primary dentin. Photomed Laser Surg 27(6):885–890
Cavalcanti AN, Pilecki P, Foxton RM, Watson TF, Oliveira MT, Gianinni M, Marchi GM (2009) Evaluation of the surface roughness and morphologic features of Y-TZP ceramics after different surface treatments. Photomed Laser Surg 27(3):473–479
Navarro RS, Gouw-Soares S, Cassoni A, Haypek P, Zezell DM, Eduardo CP (2010) The influence of erbium:yttrium-aluminum-garnet laser ablation with variable pulse width on morphology and microleakage of composite restorations. Lasers Med Sci 25(6):881–889
Aranha AC, Turbino ML, Powell GL, CdeP E (2005) Assessing microleakage of class V resin composite restorations after Er:YAG laser and bur preparation. Lasers Surg Med 37(2):172–177
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Akin, H., Tugut, F., Emine Akin, G. et al. Effect of Er:YAG laser application on the shear bond strength and microleakage between resin cements and Y-TZP ceramics. Lasers Med Sci 27, 333–338 (2012). https://doi.org/10.1007/s10103-011-0883-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-011-0883-4