Abstract
Heat generation during the removal of dental restorative materials may lead to a temperature increase and cause painful sensations or damage dental tissues. The aim of this study was to assess heat generation in dental restoration materials following laser ablation using an ultrashort pulse laser (USPL) system. A total of 225 specimens of phosphate cement (PC), ceramic (CE), and composite (C) were used, evaluating a thickness of 1 to 5 mm each. Ablation was performed with an Nd:YVO4 laser at 1,064 nm, a pulse length of 8 ps, and a repetition rate of 500 kHz with a power of 6 W. Employing a scanner system, rectangular cavities of 1.5-mm edge length were generated. A temperature sensor was placed at the back of the specimens to record the temperature during the ablation process. All measurements were made employing a heat-conductive paste without any additional cooling or spray. Heat generation during laser ablation depended on the thickness of the restoration material (p < 0.05) with the highest values in the composite group (p < 0.05), showing an increase of up to 17 K. A time delay for temperature increase during the ablation process depending on the material thickness was observed in the PC and C group (p < 0.05) with highest values for cement (p < 0.05). Employing the USPL system for removal of restorative materials, heat generation has to be considered. Especially during laser ablation next to pulpal tissues, painful sensations might occur.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
After establishing the theoretic foundations for the ‘laser’ and the ‘maser’ via a re-derivation of Max Planck’s law of radiation [1], the first theoretical description of the laser in 1958 [2] and the following experimental realization in 1960 [3], the fields of application for coherent light sources have grown rapidly. Laser technique is used in the oral cavity for a variety of dental treatment procedures. Surgical applications include excision of benign and malignant lesions [4], incision of soft tissues, biopsy, gingivectomy [5], frenectomy [6], and other soft-tissue periodontal procedures [7]. Application of laser irradiation to dental hard tissues has been described for the treatment of dental caries [8] and as an alternative for formocresol in pulpotomy of deciduous teeth [9]. Laser ablation also allows effective cleaning of the tooth surface from various dental materials [10]. Moreover, laser applications are considered to be alternative methods for a variety of dental treatment procedures as there is no mechanical vibration, causing less painful sensations [11].
In recent years, ultrashort pulsed lasers (USPL) were introduced into laser research [12]. In dentistry, the focus of this technology is to ablate oral hard and soft tissues with minimal collateral damage and high precision at sufficient ablation rates [13]. Comparing nanosecond and picosecond laser ablation in enamel, advantages toward the use of ultrashort laser pulses in dentistry are suggested [14]. Even laser energy concentration in femtosecond pulses has been evaluated and microcavities in enamel with very precise edges could be observed [15].
The present technology is based on laser systems in the range of 1-μm wavelength and pulse durations of femtosecond to picosecond [16]. The laser–tissue interaction is referred to as plasma-induced ablation or, in a more general way, photodisruption [17, 18]. Typical energy settings are in the range of up to 100 μJ, 500 kHz at a focus diameter of about 30 μm coupled with a scanner system. Unpublished preliminary studies indicate that the USPL technology might be an effective tool for the ablation of oral hard and soft tissues. Accurate preparation outlines and the lack of thermal damages around the prepared cavities suggest the use of USPL technology in dentistry. Moreover, also dental restorative materials can be removed effectively. These preliminary observations make the technology a promising tool for a variety of dental applications such as tooth cavity preparation, caries therapy, removal of restoration materials, periodontal treatment or also endodontic and implant therapy. Unfortunately, there is only low evidence for the use of USPL systems in dentistry, as systematically performed and statistically analyzed studies are missing.
One important aspect for the use of any technology in dentistry is that all tooth preparation procedures may potentially have a hazardous impact on the dental pulp. Regardless of the treatment equipment used, heat generation during the procedure can damage the tissue irreparably if uncontrolled [19, 20]. In vivo examination of dental pulps exposed to heat revealed that an elevation in temperature to 39–42°C resulted in an increase in circulation (hyperemia) [21]. If temperatures of 46–50°C were maintained for several seconds, thrombosis and a standstill of circulation occurred. An in vivo study correlated the rise in temperature on the surface of the tooth with an internal rise in temperature [20]. They found that an increase in pulpal temperature to 42.2°C led to pulpal necrosis in some cases, and a further rise in temperature caused necrosis in more than half of the teeth in their animal model. As a consequence, for any new tooth preparation technology, the possible heat generation capacity should be evaluated to avoid unwanted side-effects. Among the most studied laser systems, namely the ruby, CO2, and Nd:YAG (neodymium: yttrium-aluminum-garnet) lasers, heat generation above the pulpal tolerance is described when used on mineralized tissues [22, 23]. Preparations made with an Er:YAG (erbium: yttrium-aluminum-garnet) laser and a conventional high-speed handpiece generated similar temperature increases under water cooling [24]. The biological aspect of heat generation is one of the most important issues to be evaluated before introducing a novel technology into daily treatment concepts. The same aspect has to be regarded with respect to the removal of restoration materials from dental cavities.
At present, studies conducted so far did not evaluate thermal changes caused by ablation of restorative materials with an ultrashort pulse laser system. Thus, the aim of the study was to perform an intra-experimental comparison of heat generation during the ablation process of different dental restoration materials, testing the hypothesis of thermal changes being dependent on both the kind and the thickness of the material under study.
Materials and methods
A total of 225 specimens of phosphate cement (PC, n = 75), ceramic (CE, n = 75) and composite (C, n = 75) were used, evaluating a thickness of 1 to 5 mm at intervals of 1 mm. Consequently, all groups included 15 samples each.
Phosphate cement samples
Silicone moulds (Silflex Pink, Elephant Dental, Hoorn, Netherlands) were filled with zinc phosphate cement (Hoffmann Dental Manufaktur, Berlin, Germany) to produce samples of 6-mm length, 3-mm width, and 5-mm height using a mixing ratio of 2 g powder to 1 ml of fluid. The exact amount of both powder and fluid was verified with a high-precision gauge (SBC 53, Scaltec Instruments, Goettingen, Germany). Cement setting took place under constant pressure of 2 bar (S-U-Acrylmat No. 11105, Schuler Dental, Ulm, Germany) to avoid air bubble generation during the setting time. Thereafter, the zinc phosphate cement sample was reduced to heights of 1 to 5 mm employing a water-cooled diamond saw (Exakt 300 CP Band System, Exakt Apparatebau, Norderstedt, Germany).
Ceramic samples
The sample size of the ceramic specimens was determined by the pre-fabricated ceramic blanks used (Cerec S5-M, Sirona Dental Systems, Bensheim, Germany) of 12.5-mm length and 10.6-mm width. The ceramic blanks were reduced to heights of 1 to 5 mm employing the Exakt 300 CP water-cooled diamond saw.
Composite samples
A PVC tube with an inner diameter of 22.6 mm was used as a mould for the composite samples (Amaris O3, Voco, Cuxhaven, Germany). The tube was filled with the light-curing composite material in layers of 4 mm and polymerized employing a precision adhesive press (Exakt 402 Type 42/839, Exakt Apparatebau, Norderstedt, Germany) with a polymerization time of 30 min for each layer. After removal of the PVC tube, the composite sample was reduced to heights of 1 to 5 mm employing the Exact 300 CP water-cooled diamond saw.
Laser irradiation
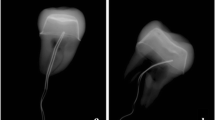
Laser irradiation was performed with an Nd:YVO4 (neodymium: yttrium-vanadate) laser at 1,064 nm (modified Super Rapid, Lumera Laser, Kaiserslautern, Germany), a pulse length of 8 ps, and a repetition rate of 500 kHz. The output power of the laser device was set to 6 W for all measurements. As a consequence, the laser irradiation time was 0.719 s with a delivered total energy of 4.314 J. Employing a scanner system (Scan Cube 7, Scanlab, Puchheim, Germany), rectangular cavities of 1.5-mm edge length were generated. Prior to temperature measurements, a preliminary survey was performed to assess the ablation of the different dental restoration materials under study. Employing an optical surface measuring system (MicroSpy, Fries Research and Technology, Bergisch Gladbach, Germany), the ablation depth of 12 specimens of each material was evaluated. Additionally, all samples were photographed employing a light microscope (Wild M8, Leica Mikrosysteme, Wetzlar, Germany).
Temperature measurements
A temperature sensor with an outer diameter of 0.5 mm was placed at the back of the specimens that recorded the temperature during the ablation process (TDA 3000, Jumbo, Fulda, Germany). For all measurements, the tip of the temperature sensor was aligned to the optical path of the laser beam using a translation stage (xyz-table LWRE3, SKF Linearsysteme, Schweinfurt, Germany) with a 0.02-mm precision of adjustment. Thereafter, the sample under study was aligned to the focal laser spot employing another translation stage (xyz-table VT-80, Micos, Eschbach, Germany) with a 0.001-mm precision of adjustment (Fig. 1). The temperature sensor was placed in contact behind the sample preserving the optical path of the laser beam. All measurements were performed employing a heat-conductive paste (P12, Wacker Silicones, Drawin Vertriebs GmbH, Ottobrunn/Riemerling, Germany) without any additional cooling or spray. Temperature measurements started 1 s before starting the ablation process to assess the baseline value. Further temperature values were measured at intervals of 1 s until the maximum temperature reading decreased. Thus, both maximum temperature value and time delay for the temperature increase could be evaluated. All measurements were performed in a room where a constant temperature of 21°C was observed by an air conditioning system.
Statistical analysis
A power analysis was performed prior to the study. Therefore, the effect size was set to 0.8 according to Cohen [25]. For an alpha-error of 0.05 and a power of 0.8, a sample size of 15 specimens in each group was calculated. For each cement, composite and ceramic sample, three temperature measurements were performed to minimize the impact of any individual structural conditions. Subsequently, the mean value of these three measurements was used for further statistical calculations, so that one sample could be considered as one statistical unit. For statistical analysis, normal distribution of the values was assessed with the Shapiro–Wilk test. Since not all data were normally distributed, values between and within a group were analyzed with a non-parametric test (Kruskal–Wallis) and Mann–Whitney pairwise comparisons. Differences were considered as statistically significant at p < 0.05. Box plot diagrams show the median, first and third quartiles, minimum and maximum values (whiskers). Values of more than 1.5 to three times the inter-quartile range are specified as outliers and marked as data points. Values more than three times the inter-quartile range are specified as far outliers and marked as asterisks.
Results
Ablation depth
Profilometry showed a median ablation depth of 3 μm (min: 0, max: 9, inter-quartile range: 4) in ceramic, 131 μm (min: 100, max: 144, inter-quartile range: 8) in composite and 17 μm (min: 9, max: 23, inter-quartile range: 3) in cement. All ablation depths were statistically significant different (p < 0.05, Mann–Whitney). A representative composite sample after laser ablation is shown in a light microscope picture and the corresponding profilometry (Fig. 2).
Maximum temperature increase
Heat generation could be observed during ablation of all dental restorative materials under study. However, temperature increase depended on the thickness of the restoration material (p < 0.05) (Fig. 3). Lowest delta temperature values could be observed in the 5 mm thickness group for both ceramic (median delta value: 1.0 K, min: 0.8, max: 1.2), composite (median delta value: 0.7 K, min: 0.6, max: 0.9) and cement (median delta value: 0.7 K, min: 0.6, max: 1.0). Highest delta temperature values could be observed in the 1 mm thickness group for all materials (ceramic: 12.4 K, min: 10.5, max: 14.7; composite: 12.2 K, min: 9.3, max: 16.7; cement: 12.4 K, min: 9.7, max: 14.7). Compared to the other materials under study, ceramic specimens showed statistically significant highest temperature values in the 2 to 5 mm groups (p < 0.05).
Temperature increase delay
A time delay for the maximum temperature after starting laser ablation could be observed in all groups (Fig. 4). Without consideration of the material thickness, lowest overall values could be measured for ceramic (median value: 2.7 s, min: 2, max: 4.3) with a statistically significant difference to composite (median value: 4.0 s, min: 2.3, max: 17.0) and cement (median value: 8.0 s, min: 3.0, max: 15.7) (p < 0.05 for all comparisons). No difference could be evaluated in the ceramic group with respect to the thickness of the samples (p > 0.05). However, a time delay for temperature increase during the ablation process became evident for PC and C with respect to the material thickness in these two groups (p < 0.05). The highest values could be observed for cement in all five thickness groups under study (p < 0.05).
Time delay measured for the maximum temperature after starting laser ablation of the different dental restoration materials. Highest latencies occurred in the cement group (p < 0.05). An increase of material thickness resulted in higher latencies of the maximum temperature in the cement and composite group (p < 0.05)
Discussion
The present study showed that heat generation during ablation of dental restorative materials with an ultrashort pulse laser system depends on the type and the thickness of the material. The amount of heat generation was not different in cement and composite layers of 1 to 5 mm but showed a higher temperature increase in thin specimens. Ceramic samples of 2 to 5 mm showed a statistically significant higher temperature increase than the other two materials under study. This difference may be caused by a threshold nature of the ablation process, which is described for nickel employing picosecond laser ablation [26]. Moreover, a threshold caused higher temperature increase in the ceramic group would be in accordance with the results of the preliminary survey. It could be shown that the ablation depth in ceramic specimens was statistically significant lower than in the other groups.
Employing a 12-ps Nd:YVO4 laser, it could be shown that USPL technology can be applied to remove dental restoration materials [27]. The authors assessed the ablation rates of different composite resin materials and observed similar rates for materials of three manufacturers. Unfortunately, they did not compare their results to other materials like ceramic or cement. Thus, it is not possible to perform an inter-experimental comparison to the results of the preliminary survey of the present study. Another study used a μs Nd:YAG laser system to remove dental restorative materials [10]. Compared to dental hard tissues, the authors found a lower ablation threshold value for all materials under study including two different composite resins, ceramics, and metal alloy. Unfortunately, there is no information given on the absolute values for temperature increase. Instead, the authors say that dental tissues were insignificantly heated when they used a laser fluence lower than the threshold values for dentine or enamel.
In the present study, in vitro laser ablation represents an exact temporally defined and reproducible stimulus. In vivo treatment times depend on the amount of the dental restorative material to be removed. Thus, different laser activation times have to be considered, resulting in different amounts of total laser energy emitted. The present study did not assess temperature changes during the removal of a restoration material with a given thickness. These data have to be evaluated in further studies to assess a possible cumulative temperature effect exceeding the pulpal threshold of heat tolerance. However, longer laser activation periods do not necessarily lead to a continuous temperature increase. For the removal of composite resin fillings using an Er:YAG laser with different pulse repetition rates it could be shown that a temperature increase did not exceed more than 5.6 K in all groups [28]. As no data are available for the removal of composite resin fillings with an USPL system, further studies have to evaluate the effect of long-lasting treatment procedures employing the novel laser device. Assessing temperature changes in the pulp chamber during halogen lamp exposure for a tooth-whitening procedure, a cumulative effect could be observed [29]. Thus, a similar effect, with temperature constant even when the energy source is turned off, has to be evaluated for USPL ablation.
In vivo studies of dental pulp tissue exposed to heat showed that hyperemia was produced in the rat incisor pulp by thermal irritation of 39–42°C [21]. Temperatures at and above 44°C caused red blood cell aggregation. If temperatures of 46–50°C were maintained for 30 s, thrombosis and a standstill of circulation occurred. An in vivo study correlated the rise in temperature on the surface of the tooth with an internal rise in temperature [20]. They found that an increase in pulpal temperature to 42.2°C caused pulpal necrosis in 15%, and a rise in temperature to 47.7°C caused necrosis in 60% of the teeth in their Macaca Rhesus monkey model. It was concluded that a temperature increase higher than 5.5 K would irreversibly damage the pulp tissue. In the present study, a temperature increase of up to 17 K could be observed. However, this must not necessarily be the amount of heat energy that reaches the pulp tissue. A study assessing composite resin materials showed that there was a quantifiable amount of heat generated in resin-containing material during light curing [30]. However, dentine sections were good thermal insulators that significantly reduced temperature rises associated with resin composite photocuring. Transferring the results of the present in vitro study to the in vivo situation, another important aspect has to be taken into account. The pulp microcirculation might affect the temperature increase. A study evaluated the rise in intrachamber temperature induced by application of various light curing units under conditions of continuous water flow inside the pulp chamber simulating pulpmicrocirculation [31]. When the simulated pulp microcirculation was absent, the temperature increases produced by all curing units except the conventional halogen lamp were large enough to be potentially harmful to the pulp. On the contrary, with the cooling effect of water flow inside the pulp chamber, all units proved to be safe for use. Thus, the importance of the cooling effect of simulated pulp microcirculation in the thermal behavior of the dentine was established. A further study could demonstrate that the thickness of tooth tissue influenced pulp temperature rise significantly [32].
Previous studies evaluated morphological and thermal aspects with respect to Nd:YAG picosecond laser ablation both in dentine and enamel [33, 34]. Assessing primary teeth, it could be shown that this technology is a safe tool for ablation of primary teeth in a broad range of operational parameters where temperature changes do not exceed 5.5 K [34].
Heat generation could be shown to depend on the thickness of the material under study. This result coincides with the findings of pulp chamber temperature increase during composite light activation with respect to dentine thickness [35]. The authors could show a significant temperature increase with the reduction in dentine thickness evaluating dentine discs of 0.5 to 2 mm. This observation is similar to the findings of the present study assessing dental restorative materials. It can be explained by the thicker material samples that might lead to a different thermal diffusivity with respect to the individual thermal properties.
The present study aimed to perform an intra-experimental comparison of heat generation during the ablation process of different dental restoration materials. The hypothesis of temperature increase being dependent on both the kind and the thickness of the material under study could be proven. Thus, heat generation has to be considered during laser ablation. Painful sensations might occur, especially during laser ablation next to pulpal tissues. As heat may cause irreversible damage to the dentine pulp complex, further studies have to evaluate the clinical impact of the in vitro measured temperature increase with respect to dental tissues, the pulp microcirculation, and intra-pulp chamber temperature changes. Possibly, a cooling procedure has to be used for ablation of dental restorative materials next to pulpal tissues.
References
Einstein A (1916) Zur Quantentheorie der Strahlung. Mitt Phys Ges Zur 18:121–128
Schawlow AL, Townes CH (1958) Infrared and optical masers. Phys Rev 112:1940–1949
Maiman TH (1960) Stimulated optical radiation in ruby. Nature 187:493–494
Vescovi P, Corcione L, Meleti M, Merigo E, Fornaini C, Manfredi M, Bonanini M, Govoni P, Rocca JP, Nammour S (2010) Nd:YAG laser versus traditional scalpel. A preliminary histological analysis of specimens from the human oral mucosa. Lasers Med Sci 25:685–691
Soares FM, Tarver EJ, Bimstein E, Shaddox LM, Bhattacharyya I (2009) Gingival overgrowth in a child with arthrogryposis treated with a Er,Cr:YSGG laser: a case report. Pediatr Dent 31:8–13
Haytac MC, Ozcelik O (2006) Evaluation of patient perceptions after frenectomy operations: a comparison of carbon dioxide laser and scalpel techniques. J Periodontol 77:1815–1819
Russo J (1997) Periodontal laser surgery. Dent Today 16:80–81
Ricketts DN, Pitts NB (2009) Novel operative treatment options. Monogr Oral Sci 21:174–187
Toomarian L, Fekrazad R, Sharifi D, Baghaei M, Rahimi H, Eslami B (2008) Histopathological evaluation of pulpotomy with Er,Cr:YSGG laser vs formocresol. Lasers Med Sci 23:443–450
Siniaeva ML, Siniavsky MN, Pashinin VP, Mamedov AA, Konov VI, Kononenko VV (2009) Laser ablation of dental materials using a microsecond Nd:YAG laser. Laser Phys 19:1056–1060
Braun A, Jepsen S, Deimling D, Ratka-Krueger P (2010) Subjective intensity of pain during supportive periodontal treatment using a sonic scaler or Er:YAG laser. J Clin Periodontol 37:340–345
Vogel A, Venugopalan V (2003) Mechanisms of pulsed laser ablation of biological tissues. Chem Rev 103:577–644
Altshuler GB, Belashenkov NR, Karasev VB, Skripnik AV, Solunin AA (1993) Application of ultrashort laser pulses in dentistry. Proc SPIE 2080:77–86
Lizarelli RF, Kurachi C, Misoguti L, Bagnato VS (2000) A comparative study of nanosecond and picosecond laser ablation in enamel: morphological aspects. J Clin Laser Med Surg 18:151–157
Lizarelli RF, Costa MM, Carvalho-Filho E, Nunes FD, Bagnato VS (2008) Selective ablation of dental enamel and dentin using femtosecond laser pulses. Laser Phys Lett 5:63–69
Konorov SO, Mitrokhin VP, Fedotov AB, Sidorov-Biryukov DA, Beloglazov VI, Skibina NB, Shcherbakov AV, Wintner E, Scalora M, Zheltikov AM (2004) Laser ablation of dental tissues with picosecond pulses of 1.06-micron radiation transmitted through a hollow-core photonic-crystal fiber. Appl Opt 43:2251–2256
Niemz MH (1994) Investigation and spectral analysis of the plasma-induced ablation mechanism of dental hydroxyapatite. Appl Phys B 58:273–281
Niemz MH (1998) Laser-tissue-interactions: fundamentals and applications. Springer, Berlin Heidelberg New York
Cavalcanti BN, Otani C, Rode SM (2002) High-speed cavity preparation techniques with different water flows. J Prosthet Dent 87:158–161
Zach L, Cohen G (1965) Pulp response to externally applied heat. Oral Surg Oral Med Oral Pathol 19:515–530
Pohto M, Scheinin A (1958) Microscopic observations on living dental pulp, Part 2. The effect of thermal irritants on the circulation of the pulp in the lower rat incisor. Acta Odontol Scand 16:315–327
Anic I, Vidovic D, Luic M, Tudja M (1992) Laser induced molar tooth pulp chamber temperature changes. Caries Res 26:165–169
Gow AM, McDonald AV, Pearson GJ, Setchell DJ (1999) An in vitro investigation of the temperature rises produced in dentine by Nd:YAG laser light with and without water-cooling. Eur J Prosthodont Restor Dent 7:71–77
Cavalcanti BN, Lage-Marques JL, Rode SM (2003) Pulpal temperature increases with Er:YAG laser and high-speed handpieces. J Prosthet Dent 90:447–451
Cohen J (1988) Statistical power analysis for the behavioral sciences, 2nd edn. Lawrence Erlbaum Associates, Hillsdale
Willis DA, Xu X (2002) Heat transfer and phase change during picosecond laser ablation of nickel. Int J Heat Mass Transfer 45:3911–3918
Wieger V, Strassl M, Wintner E (2006) Pico- and microsecond laser ablation of dental restorative materials. Laser Part Beams 24:41–45
Correa-Afonso AM, Pécora JD, Palma-Dibb RG (2008) Influence of pulse repetition rate on temperature rise and working time during composite filling removal with the Er:YAG laser. Photomed Laser Surg 26:221–225
Coutinho DS, Silveira L Jr, Nicolau RA, Zanin F, Brugnera A Jr (2009) Comparison of temperature increase in in vitro human tooth pulp by different light sources in the dental whitening process. Lasers Med Sci 24:179–185
Al-Qudah AA, Mitchell CA, Biagioni PA, Hussey DL (2005) Thermographic investigation of contemporary resin-containing dental materials. J Dent 33:593–602
Kodonas K, Gogos C, Tziafa C (2009) Effect of simulated pulpal microcirculation on intrachamber temperature changes following application of various curing units on tooth surface. J Dent 37:485–490
Kodonas K, Gogos C, Tziafa C (2009) Effect of simulated pulpal microcirculation on intrapulpal temperature changes following application of heat on tooth surfaces. Int Endod J 42:247–252
Lizarelli RF, Kurachi C, Misoguti L, Bagnato VS (1999) Characterization of enamel and dentin response to Nd:YAG picosecond laser ablation. J Clin Laser Med Surg 17:127–131
Lizarelli RF, Moriyama LT, Bagnato VS (2006) Temperature response in the pulpal chamber of primary human teeth exposed to Nd:YAG laser using a picosecond pulsed regime. Photomed Laser Surg 24:610–615
da Silva EM, Penelas AG, Simão MS, Filho JD, Poskus LT, Guimarães JG (2010) Influence of the degree of dentine mineralization on pulp chamber temperature increase during resin-based composite (RBC) light-activation. J Dent 38:336–342
Acknowledgements
This investigation was supported by the Federal Ministry of Education and Research, Germany. We acknowledge Voco for providing the composite material.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Braun, A., Wehry, R.J., Brede, O. et al. Heat generation caused by ablation of restorative materials with an ultrashort pulse laser (USPL) system. Lasers Med Sci 27, 297–303 (2012). https://doi.org/10.1007/s10103-010-0875-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-010-0875-9