Abstract
The formation of a superficial layer of tiny flakes has been observed on teeth prepared by Erbium lasers. It has been suggested that removing this layer (mechanically or chemically) may increase the bond strength of the resin composite. The purpose of this study is to evaluate the effect of various etching times on bond strength of resin composite to enamel and dentin prepared by Er,Cr:YSGG laser. Sixty previously flattened human molars were irradiated for 10 s by an Er,Cr:YSGG laser. Enamel (E) specimens were etched with 37% H3PO4 for 20, 40 or 60 s and dentin (D) specimens were etched for 15 or 30 s. All specimens were prepared for a standard shear bond strength (SBS) test (1 mm/min). Data were analyzed [ANOVA, Tukey post-hoc, a < 0.05)] and the failure mode was studied under SEM. Mean SBS±sd (MPa) for each group was 16.97 ± 7.77 (E20s), 21.34 ± 3.55 (E40s), 14.08 ± 4.77 (E60s), 13.62 ± 7.28 (D15s) and 13.15 ± 6.25 (D30s). SBS for E40s was significantly higher than E60s (p = 0.023). No difference was noted between the dentin groups. SEM evaluation showed predominantly cohesive failure. Within the limits of this study, etching time significantly influenced the SBS of composite resin to laser-prepared enamel. SEM showed subsurface cracks, fissures, and deformities leading to predominantly cohesive failure in both enamel and dentin.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Erbium (Er.) lasers were introduced into dentistry specifically as an alternative to traditional mechanical instrumentation for the preparation of tooth structure [1]. These lasers emit energy in the wavelength range of 2.6 and 3 µm. This range coincides with the strongest absorption peak of water, an important component of dental hard tissues [2]. The sudden evaporation of bound water (2–4% by weight in enamel) causes micro-explosions that blast away tiny particles of the tooth [2]. In addition to the selective removal of carious enamel and dentin, the advantages of using lasers for hard tissue preparation include bactericidal effects and less noise, vibration, and discomfort for the patient than a rotary handpiece [3, 4].
A member of the Er laser family, the Er,Cr:YSGG pulsed laser used with an air-water spray may be used to prepare enamel, dentin, cementum, and bone efficiently and cleanly without leaving a smear layer [5, 6].
Despite its efficiency, reported bond strengths of composite resin to tooth substrate prepared by erbium laser are often confusing and contradictory. Some studies have reported higher bond strengths to laser-prepared than to acid-etched dentin [7, 8]. Others have reported significantly lower bond strengths [9–12] and others have reported no significant differences [13, 14].
Since its introduction by Buonocore in 1955 [15], the acid-etch technique has been the subject of many investigations. Major topics of concern among these studies have been the type and concentration of acids [16], etching interval [17], the influence of air drying [18], and the effect of enamel contamination [19].
Early observations of enamel and dentin surfaces prepared by erbium lasers demonstrated a similarity to acid-etched tooth structure [8, 14]. These findings motivated clinicians to use a laser as an alternative to chemical etching [7, 14]. Later investigations showed patterns of micro-irregularities, often accompanied by micro-fissure propagation, fusion, or re-crystallization areas and absence of smear layer [1]. Hibst demonstrated the formation of a superficial layer of tiny flakes with laser tooth preparation. These flakes can easily break and reduce bond strength. Hibst suggested that this layer should be removed before any application of the filling material [1]. To overcome this problem, mechanical or chemical removing of this layer has been suggested. Gutknecht et al. and Carvalho et al. suggested acid-etching the laser-prepared cavity [20, 21].
Morphological changes to tooth structure resulting from laser irradiation may affect the performance of dental restorative materials, especially adhesive systems. Since many bonding systems now recommend an etching step prior to adhesive placement, the aim of the current study is to investigate the effect of different etching time on the shear bond strength of composite resin bonded to enamel and dentin using a current-generation bonding system.
Materials and methods
Sixty freshly extracted caries and restoration-free permanent human molars stored in sodium azide solution (0.4%) were selected after scaling to remove residual tissues and calculus. The samples were embedded in an acrylic resin with the occlusal surface of the crown exposed and parallel to the base of the resin block. Specimens were randomly divided into two groups, enamel (E, n = 36) and dentin (D, n = 24).
Sample preparation
Samples were wet-ground with 320-grit and polished with 600-grit to obtain a flat enamel or dentin surface. Surfaces were evaluated under a laboratory magnification lens to confirm that no dentin was exposed in enamel group and no enamel remained in the dentin group (except at the periphery). The specimens were stored in distilled water at 37°C and 100% humidity in a controlled incubator.
Laser exposure
An Er,Cr:YSGG laser (Waterlase, BioLase Technology Inc, San Clemente, CA, USA) operating at a wavelength of 2,780 nm, fixed repetition rate of 20 Hz and 140-μs pulse duration coupled with an adjustable air-water spray was used. Parameters for enamel specimens were 4.5 W (225 mJ/Pulse) 60% air, 80% water and 3 W (150 mJ/pulse) 60% air, 70% water for dentin samples. The laser energy was delivered through a fiber-optic system to a sapphire tip terminal 600 μm in diameter (G6, BioLase Technology Inc, San Clemente, CA, USA).
Samples were lased for 10 s in the non-contact mode perpendicular to the flat specimen surface with a 1-mm fixed distance from the laser tip. A sweeping motion was used to achieve an even coverage of the surface by overlapping the laser impacts. A surface area of approximately 4 × 3 mm was prepared in this manner. The energy density delivered to the enamel surface was 80 J/cm2 and 53 J/cm2 for the dentin samples. To ensure consistent energy density, spot size, distance, and handpiece angle, the laser hand piece was attached to a modified surveyor.
Etching procedure
Enamel samples were randomly divided into three subgroups (E20s, E40s, and E60s) and dentin specimens into two subgroups (D15s and D30s) with equal number of samples per group (n = 12). Prior to acid etching, the samples were gently air dried to remove the excess water and then 37% phosphoric acid (Patterson Brand LOT# 060278) was applied to group E20s for 20 s, E40s for 40 s, E60s for 60 s, D15s for 15 s and D30s for 30 s. Samples were rinsed with water spray for 30 s.
Bonding procedure
Specimens were blotted to remove excess water using a cotton pellet to obtain a glistening surface without water pooling. Bonding procedures recommended by the manufacturer were strictly followed. Two consecutive coats of the adhesive system (Adper Single bond plus, 3 M-ESPE, MN, USA LOT # 7LE) were immediately applied to the exposed etched surface for 15 s with gentle agitation using a fully saturated applicator. The surface was gently air-dried for 5 s to evaporate bonding solvents, and light cured (LED 5, Ultradent, UT, USA) for 10 s.
A transparent plastic tube of 1.5 mm inner diameter was filled with 3 mm of composite (Filtek Supreme Plus 3 M-ESPE, MN, USA LOT#5BR A3 Body Shade) and placed on the treated surface. The tube was exposed to the curing light for 40 s (20 s from each side). Light intensity of the curing light device was measured between every ten samples and was determined to be 663 ± 60 mW/cm2 by a laser power meter (Field Mate, Coherent Inc., OR, USA).
Subsequently, any excess material was removed with a sharp surgical blade. Samples were left in distilled water at 37°C for 48 h. Laboratory conditions during the specimen preparation were monitored (temperature: 24 ± 2°C, humidity: 36 ± 2%) and the samples were kept moist to avoid drying and cracking.
Shear bond strength (SBS) testing
Prior to loading, the tube mold was carefully removed with a sharp blade. The specimens were then placed in a custom-made fixture mounted on a Universal Testing Machine (INSTRON Model 5565, MA, USA) and were loaded to failure under compression using a knife-edge loading head at a cross-head speed of 1 mm/min. The investigator performed the load testing without knowledge of the group treatment. Maximum load to failure was recorded for each sample and the SBS was expressed in megapascals (MPa), which is derived by dividing the imposed force (Newtons) by the bond area (mm2)
SEM study
To evaluate the failure mode, the composite cylinders were mounted on aluminum stubs; sputter-coated with gold-palladium and examined under a scanning electron microscope (SEM) (ISI SX-30 Cambridge, MA, USA). The failure mode was classified as adhesive (adhesive failure); cohesive enamel, dentin, or composite substrate failure, or mixed (adhesive and cohesive failure).
Statistical analysis
Means and standard deviation of SBS were calculated and differences between groups were analyzed using one-way analysis of variance (ANOVA) and Tukey-Kramer post-hoc testing (α = .05).
Results
Shear bond strength (SBS)
Mean SBS±sd (MPa) for each group was 16.97 ± 7.77 (E20s), 21.34 ± 3.55 (E40s), 14.08 ± 4.77 (E60s), 13.62 ± 7.28 (D15s) and 13.15 ± 6.25 (D30s) (Fig. 1). The maximum SBS observed enamel was in group E20s (32.85 MPa) and the minimum was in group E60s (8.61 MPa), the maximum SBS observed in dentin group was in group D30s (25.49 MPa) and the minimum was in group D15s (4.19 MPa).
Some samples were dislodged and debonded during the preparation for the shear test, thus the uneven sample distribution. ANOVA showed a significant difference between enamel groups (P = 0.024). Further analysis using the Tukey-Kramer test indicated that mean SBS for E40s (21.34 ± 3.55 MPa) was significantly higher than E60s (14.08 ± 4.77 MPa) (P = 0.022). No difference was noted between E20s and E40s or E20s and E60s. There was no difference between the dentin groups (Tables 1 and 2).
Failure mode
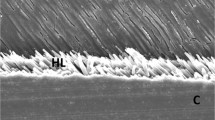
The failure mode of each specimen is presented in Table 3. SEM evaluation showed that the enamel samples tend to fail more cohesively in enamel. Only one sample in group E40s failed adhesively, the rest of the specimens had some amount of cohesive failure; 50% in group E20s, 37% in group E40s, and 80% in group E60s failed cohesively in enamel.
The remaining samples had a mixture of adhesive and cohesive failures. In the latter, cohesive failure surface was predominant except in one sample (group E20s), which showed bigger surface area of adhesive failure. It is noteworthy that dentin cohesive failure was seen in only a few of the samples of group E60s. The dentin samples also showed predominantly cohesive failure. In a few cases, a mixture failure was seen but the remainder failed cohesively in dentin (Figs. 2 and 3).
SEM photograph (45x) of fractured enamel–adhesive interface in the composite bar side. a A representative of group E20s, cohesive fracture mode. As seen in the picture, the sample interface is totally covered by a thin layer of enamel (CC Composite cylinder). b A representative of group E40s; despite a round cross section of the composite bar, the fracture interface observed was irregularly shaped in most cases (EC Exposed composite)
Discussion
The bond strength of adhesive systems is one of the major factors to be considered when placing a restoration [4]. This restoration parameter can be accurately measured by the bonding test. Bonding of resin composite material to tooth structure prepared with different type of lasers has been reported [3, 8, 12, 22–24]. These investigations have reported variable results comparing bond strengths of laser-prepared and bur-prepared enamel and dentin [4, 8, 14, 25]. They suggested that acid etching after laser preparation is recommended and may improve the bond strength [3, 20, 21, 26]. However, there are few data demonstrating the effect of etching time on the bonding performance of laser-prepared enamel and dentin.
Data from this investigation demonstrated that higher shear bond strength in enamel was observed when the etching time was increased to 40 s, but the differences were not statistically significant (p > 0.237). The results showed that increasing the time to 60 s had a detrimental effect. Shear bond strength values to 20 s for acid-etched enamel (16.97 ± 7.77 MPa) and 15 s for etched dentin (13.62 ± 7.28 MPa) in this study were similar to those reported previously [4, 10].
Conventional burs create smooth surfaces in the dentin coated by a smear layer. Treatment with phosphoric acid produces a repeating surface pattern, with cracks and fissures no deeper than 12 μm that are readily filled with resin [27, 28]. In contrast to bur preparation, the erbium laser creates rough surfaces free of smear layer, extensive surface fissuring, and less homogeneous and regular surface patterns [2].
As described by Perdigao et al., it seems that the bonding mechanism of resin to acid-etched dentin is well understood to be micromechanical, but little is known about the mechanism of resin adhesion to laser-etched dentin. The formation of an inter-diffusion zone similar to that described for acid-etched dentin seems to be unlikely [29].
It has been hypothesized that because the surface layer of laser-prepared cavities is severely fissured and probably denatured, micromechanical retention is likely to be inadequate with bond strength developing solely from penetration of resin tags into dentinal tubules [8, 12, 30].
Jassem et al. has shown that resin tags are responsible for only a small fraction of bond strength of composite to etched dentin [31], which may explain the reduced bond strength with laser-prepared tooth structures.
On the other hand, commercial dental laser manufacturers claim that enamel and dentin can be successfully etched at lower power settings with the erbium lasers [26]. Despite this common suggestion, this protocol was not used to etch the enamel or dentin surfaces because sub-ablative energies are prone to cause more cracks with subsequently lower restoration quality.
Apel et al. investigated the ablation threshold of Er:YAG and Er:YSGG lasers used when preparing tooth structures and noted that there is a possibility of micro-cracks developing in enamel below the ablation threshold. These cracks act as starting points for fracture and failure, which may reduce or eliminate the possible positive effect of erbium laser irradiation [32]. Various other effects were observed in their study, such as slight smoke evolution and opaque, chalky, or brownish discoloration within the enamel that occurred with radiation below the ablation threshold [32].
Another reason not to use lower power as a laser-etching procedure was the reports of lower bond strength when using this technique compare to acid etching [3, 10, 11, 26]. Irradiated enamel and dentin respond differently to acid etching than to surfaces obtained with a conventional high-speed bur. The peritubular dentin seems to be more resistant to acid etching; intertubular dentin became weakened and highly demineralized after etching and if not completely impregnated by monomers, it creates a hybrid layer more susceptible to hydrolysis [33].
Although adjunctive use of phosphoric acid following water-rinsing appeared to have eliminated the surface laser-modified layer, the thermomechanical effects produced by laser irradiation probably extend into the subsurface dentin, undermining the integrity of the resin-dentin interface [13]. Kataumi et al. observed resin-dentin interfaces and found micro-cracks below the hybrid layer, indicating that subsurface damage was caused by the Er:YAG irradiation [13]. These findings confirm our SEM observations that demonstrate enamel and dentin cohesive fractures. By means of transmission electron microscope (TEM) study of laser-irradiated dentin they reported 3–4 μm of severely altered subsurface dentin, in which collagen fibrils appeared to have lost cross-banding and were fused together, eliminating interfibrillar spaces [13]. This in particular could explain the cohesive fractures of enamel and dentin frequently observed in this and other studies. It is noteworthy to mention that the final pattern of fracture may not only demonstrate the resistance values but can also be determined by stress that occurs during the test, the material structure, the crack propagation, and the properties and dynamics of the fracture itself [34].
When comparing the SBS of the same bonding system (Adper Single bond, 3 M ESPE) to conventional bur-prepared enamel and dentin as reported by other investigators [10, 35], it is revealed that the bond strength value of E40s is relatively close to the bond strength of bur-prepared enamel [10], but this is not the case when comparing the bond strength of laser-prepared dentin (both D15s and D30s) and bur-prepared dentin [35]. Laser-prepared dentin showed lower values and significantly weaker bond strength than conventional bur-prepared dentin [10, 35]. The results of this investigation suggest that chemical etching be employed for 40 s to enamel prepared by a laser to obtain higher bond strengths. Further work is required to improve bond strength of laser-prepared dentin, perhaps by enhancement in the strength of dentinal structure or increased resin penetration into micro-porosities.
In this investigation, only one bonding system was tested. Other bonding systems used in dentistry may yield different results. From the laser perspective, we chose safe and effective laser parameters within the range of the manufacturer’s recommendations. Different parameters could vary shear bond strengths values. Further work is required to determine whether the present findings apply equally to other bonding systems, different bonding procedures, and different laser parameters, before the laser can be established as a reliable operative technique in dentistry.
Conclusions
Within the limits of this in vitro study, it is concluded that etching time can significantly influence the bonding of composite resin to enamel prepared by an Er,Cr:YSGG laser. In this regard, it is recommended to increase etching time to 40 s to obtain better bond strength, but not to 60 s, which may degrade the shear bond strength of the composite resin to the enamel. There were no differences observed in shear bond strength when lased dentin was etched for 15 or 30 s. Cohesive failure was the predominant failure mode in both enamel and dentin. SEM revealed subsurface cracks, fissures, and deformities which may affect the integrity of the lased enamel and dentin.
References
Hibst R (2004) Laser for caries removal and cavity preparation: state of the art and future directions. J Oral Laser Appl 2:203–212
Hibst R, Keller U (1989) Experimental studies of the application of the Er:YAG laser on dental hard substances: I. Measurement of the ablation rate. Lasers Surg Med 9:338–344. doi:10.1002/lsm.1900090405
Dunn WJ, Davis JT, Bush AC (2005) Shear bond strength and SEM evaluation of composite bonded to Er:YAG laser-prepared dentin and enamel. Dent Mater 21:616–624. doi:10.1016/j.dental.2004.11.003
Oliveira DC, Manhaes LA, Marques MM, Matos AB (2005) Microtensile bond strength analysis of different adhesive systems and dentin prepared with high-speed and Er:YAG laser: a comparative study. Photomed Laser Surg 23:219–224. doi:10.1089/pho.2005.23.219
Eversole LR, Rizoiu IM (1995) Preliminary investigations on the utility of an erbium, chromium YSGG laser. J Calif Dent Assoc 23:41–47
Eversole LR, Rizoiu I, Kimmel AI (1997) Pulpal response to cavity preparation by an erbium, chromium:YSGG laser-powered hydrokinetic system. J Am Dent Assoc 128:1099–1106
Carrieri TC, Freitas PM, Navarro RS, Eduardo CP, Mori M (2007) Adhesion of composite luting cement to Er:YAG-laser-treated dentin. Lasers Med Sci 22:165–170. doi:10.1007/s10103-006-0433-7
Visuri SR, Gilbert JL, Wright DD, Wigdor HA, Walsh JT Jr (1996) Shear strength of composite bonded to Er:YAG laser-prepared dentin. J Dent Res 75:599–605
Armengol V, Jean A, Weiss P, Hamel H (1999) Comparative in vitro study of the bond strength of composite to enamel and dentin obtained with laser irradiation or acid-etch. Lasers Med Sci 14:207–215. doi:10.1007/s101030050086
Botta SB, da Ana PA, Zezell DM, Powers JM, Matos AB (2007) Adhesion after erbium, chromium:yttrium-scandium-gallium-garnet laser application at three different irradiation conditions. Lasers Med Sci.. doi:10.1007/s10103-007-0521-3
Gurgan S, Kiremitci A, Cakir FY, Yazici E, Gorucu J, Gutknecht N (2007) Shear bond strength of composite bonded to erbium:yttrium-aluminum-garnet laser-prepared dentin. Lasers Med Sci.. doi:10.1007/s10103-007-0532-0
Martinez-Insua A, Da Silva DL, Rivera FG, Santana-Penin UA (2000) Differences in bonding to acid-etched or Er:YAG-laser-treated enamel and dentin surfaces. J Prosthet Dent 84:280–288. doi:10.1067/mpr.2000.108600
Kataumi M, Nakajima M, Yamada T, Tagami J (1998) Tensile bond strength and SEM evaluation of Er:YAG laser irradiated dentin using dentin adhesive. Dent Mater 17:125–138
Lin S, Caputo AA, Eversole LR, Rizoiu I (1999) Topographical characteristics and shear bond strength of tooth surfaces cut with a laser-powered hydrokinetic system. J Prosthet Dent 82:451–455. doi:10.1016/S0022-3913(99)70033-8
Buonocore MG (1955) A simple method of increasing the adhesion of acrylic filling materials to enamel surfaces. J Dent Res 34:849–853
Wang WN, Yeh CL, Fang BD, Sun KT, Arvystas MG (1994) Effect of H3PO4 concentration on bond strength. Angle Orthod 64:377–382
Holtan JR, Nystrom GP, Phelps RA, Anderson TB, Becker WS (1995) Influence of different etchants and etching times on shear bond strength. Oper Dent 20:94–99
Ichiki K, Fukushima T, Yoshida Y, Horibe T (1990) Correlation between air-drying duration and bond strength of composite resins to teeth. J Prosthet Dent 63:525–529. doi:10.1016/0022-3913(90)90069-O
Xie J, Powers JM, McGuckin RS (1993) In vitro bond strength of two adhesives to enamel and dentin under normal and contaminated conditions. Dent Mater 9:295–299. doi:10.1016/0109-5641(93)90046-S
Carvalho RC, Freitas PM, Otsuki M, Eduardo CP, Tagami J (2008) Micro-shear bond strength of Er:YAG-laser-treated dentin. Lasers Med Sci 23:117–124. doi:10.1007/s10103-006-0434-6
Gutknecht N, Apel C, Schafer C, Lampert F (2001) Microleakage of composite fillings in Er,Cr:YSGG laser-prepared class II cavities. Lasers Surg Med 28:371–374. doi:10.1002/lsm.1064
Drummond JL, Wigdor HA, Walsh JT Jr, Fadavi S, Punwani I (2000) Sealant bond strengths of CO(2) laser-etched versus acid-etched bovine enamel. Lasers Surg Med 27:111–118, doi:10.1002/1096-9101(2000)27:2<111::AID-LSM2>3.0.CO;2-L
Rolla JN, Mota EG, Oshima HM, Burnett LH Jr, Spohr AN (2006) Nd:YAG laser influence on microtensile bond strength of different adhesive system for human dentin. Photomed Laser Surg 24:730–734. doi:10.1089/pho.2006.24.730
Walsh LJ, Abood D, Brockhurst PJ (1994) Bonding of resin composite to carbon dioxide laser-modified human enamel. Dent Mater 10:162–166. doi:10.1016/0109-5641(94)90026-4
Corpas-Pastor L, Villalba MJ, Lopez-Gonzalez Garrido D, Pedraza M, Moore K, Elias A (1997) Comparing the tensile strength of brackets adhered to laser-etched enamel vs. acid-etched enamel. J Am Dent Assoc 128:732–737
Munck J, Van Meerbeek B, Yudhira R, Lambrechts P, Vanherle G (2002) Micro-tensile bond strength of two adhesives to erbium:YAG-lased vs. bur-cut enamel and dentin. Eur J Oral Sci 110:322–329. doi:10.1034/j.1600-0722.2002.21281.x
Rux W, Cooley RL, Hicks JL (1991) Evaluation of a phosphonate BIS-GMA resin as a bracket adhesive. Quintessence Int 22:57–60
Van Meerbeek B, Inokoshi S, Braem M, Lambrechts P, Vanherle G (1992) Morphological aspects of the resin-dentin interdiffusion zone with different dentin adhesive systems. J Dent Res 71:1530–1540
Perdigao J, Swift EJ Jr, Denehy GE, Wefel JS, Donly KJ (1994) In vitro bond strengths and SEM evaluation of dentin bonding systems to different dentin substrates. J Dent Res 73:44–55
Aoki A, Ishikawa I, Yamada T, Otsuki M, Watanabe H, Tagami J, Ando Y, Yamamoto H (1998) Comparison between Er:YAG laser and conventional technique for root caries treatment in vitro. J Dent Res 77:1404–1414
Jassem HA, Retief DH, Jamison HC (1981) Tensile and shear strengths of bonded and rebonded orthodontic attachments. Am J Orthod 79:661–668. doi:10.1016/0002-9416(81)90358-4
Apel C, Meister J, Ioana RS, Franzen R, Hering P, Gutknecht N (2002) The ablation threshold of Er:YAG and Er:YSGG laser radiation in dental enamel. Lasers Med Sci 17:246–252. doi:10.1007/s101030200036
Tay FR, Carvalho RM, Yiu CK, King NM, Zhang Y, Agee K, Bouillaguet S, Pashley DH (2000) Mechanical disruption of dentin collagen fibrils during resin-dentin bond testing. J Adhes Dent 2:175–192
Armstrong SR, Keller JC, Boyer DB (2001) Mode of failure in the dentin-adhesive resin-resin composite bonded joint as determined by strength-based (muTBS) and fracture-based (CNSB) mechanical testing. Dent Mater 17:201–210. doi:10.1016/S0109-5641(00)00070-1
Kim SY, Lee IB, Cho BH, Son HH, Um CM (2006) Curing effectiveness of a light emitting diode on dentin bonding agents. J Biomed Mater Res B Appl Biomater 77:164–170. doi:10.1002/jbm.b.30426
Acknowledgements
The authors would like to thank Dr. Jorg Miester, Ms. Carla Flemming, and Mr. Reid Marshal for their help and support. This study was supported by the Department of Comprehensive Dentistry and the Department of Prosthodontics and Biomaterials, School of Dentistry, University of Alabama at Birmingham.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was supported by the Department of Comprehensive Dentistry and the Department of Prosthodontics and Biomaterials, School of Dentistry, from the University of Alabama at Birmingham.
Rights and permissions
About this article
Cite this article
Obeidi, A., Liu, PR., Ramp, L.C. et al. Acid-etch interval and shear bond strength of Er,Cr:YSGG laser-prepared enamel and dentin. Lasers Med Sci 25, 363–369 (2010). https://doi.org/10.1007/s10103-009-0652-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-009-0652-9