Abstract
This study tested if dentin adhesion is affected by Er:YAG laser. Ninety dentin disks were divided in groups (n = 10): G1, control; G2, Er:YAG laser 150 mJ, 90° contact, 38.8 J/cm2; G3, Er:YAG laser 70 mJ, 90° contact, 18.1 J/cm2; G4, Er:YAG laser 150 mJ, 90° non-contact, 1.44 J/cm2; G5, Er:YAG laser 70 mJ, 90° non-contact, 0.67 J/cm2; G6, Er:YAG laser 150 mJ, 45° contact, 37.5 J/cm2; G7, Er:YAG laser 70 mJ, 45° contact, 17.5 J/cm2; G8, Er:YAG laser 150 mJ, 45° non-contact, 1.55 J/cm2; and G9, Er:YAG laser 70 mJ, 45° non-contact, 0.72 J/cm2. Bonding procedures were carried out and the micro-shear-bond strength (MSBS) test was performed. The adhesive surfaces were analyzed under SEM. Two-way ANOVA and multiple comparison tests revealed that MSBS was significantly influenced by the laser irradiation (p < 0.05). Mean values (MPa) of the MSBS test were: G1 (44.97 ± 6.36), G2 (23.83 ± 2.46), G3 (30.26 ± 2.57), G4 (35.29 ± 3.74), G5 (41.90 ± 4.95), G6 (27.48 ± 2.11), G7 (34.61 ± 2.91), G8 (37.16 ± 1.96), and G9 (41.74 ± 1.60). It was concluded that the Er:YAG laser can constitute an alternative tool for dentin treatment before bonding procedures.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Roughness and free surface energy play an important role on the bonding procedure and can increase the adhesion of composite materials to dentin. The increase on adhesion strength depends on the adhesive ability to spread on dentin surface, which is referred to as wettability. To improve wettability and bonding, the free surface energy of dentin must be increased by the use of conditioners and primers [1, 2].
It is well known that acid-etching leads to physicochemical changes on dentin surface, beneficial to micro-mechanical and chemical attachment of resin to the dentin. The most effective approach appears to be the formation of a dentin–resin inter-diffusion zone or hybrid layer [1]. The use of self-etching primers has been extensively reported in the literature and results support that there is an increase in dentin bonding, even with a thick hybrid layer formation [3, 4]. Although these simplified systems are convenient to use, a perfect bond to dentin still remains as one of the most important and challenging features to be considered when choosing adhesive materials.
Some authors [1, 5] reported that the surface topography also interferes on bonding procedures; the degree of surface roughness seems to indicate the degree of mechanical anchorage in bonding process.
Laser has been introduced in clinical dentistry for removal of dental hard tissues before the application of restorative materials [6]. One believes that the effects of laser irradiation on tooth structure are dependent on wavelength specificity, energy density, contact or non-contact mode of irradiation, and incidence angles. Er:YAG lasers emit a wavelength of 2.94 μm and can ablate dental hard tissues more effectively than other lasers [7, 8] due to its high coefficient of absorption in both water and hydroxyapatite and because it only minimally increases temperature in the surrounding tissues, especially when constant cooling is achieved with continuous water spray [9].
As the laser energy absorbed by dental tissue produces surface modifications, it has been suggested that laser could be used for the pretreatment of dentin and for enhancing the bonding of adhesive restorative materials [10, 11]. Several characteristics of lased dentin have previously been considered as advantageous for resin bonding. They include the formation of a microscopically rough surface without demineralization and open dentinal tubules without smear layer production [10–16].
To obtain a higher bond strength of resin to dentin, this study aimed to evaluate the effect of different parameters of the Er:YAG laser irradiation on dentin micro-shear bond strength (MSBS). In addition, the treated dentin surfaces were evaluated morphologically under SEM. The null hypothesis tested was that there is no difference in the MSBS of the dentin irradiated with different parameters of the Er:YAG laser and the non-irradiated surface, when followed by the application of a self-etching primer.
Understanding how laser treatment contributes to the adhesion of resin to dentin may help the professional in selecting the best parameter of irradiation for a specific clinical application. This understanding is the key for clinical success, where excellence in esthetics should parallel oral health maintenance.
Materials and methods
Preparation of the specimens
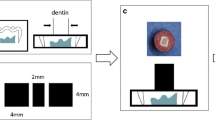
Forty-five non-carious freshly extracted human third molars were cleaned with a rotary brush with pumice and stored in physiological serum at 4°C until its use. The teeth were fixed with cyanoacrylate adhesive (Zapit Base, Dental Ventures of America, Corona, USA) on a metal disk. To obtain samples of similar size, the teeth were sectioned at the cementum–enamel junction. Ninety dentin disks of approximately 2-mm thick were obtained from the lingual and buccal surfaces by slow-speed sectioning with a diamond saw (Isomet-Buehler Lake Buff, IL, USA). Each slice was ground with a 600-grit silicon carbide paper (Struers, Tokyo, Japan) under running water to provide uniform surfaces of superficial dentin. An area of 6 × 9 mm was delimited on the surface of each specimen on which the laser irradiation was performed. Figure 1 illustrates the experimental design.
a Third molars were collected and cleaned. b Dentin disks of 2 mm were obtained from the crowns. c An area of 6 × 9 mm was delimited on the dentin surface of each sample. d Laser irradiation was performed with different parameters (contact/non-contact mode of irradiation, beam angle, and energy). e A tygon tube was cut to obtain matrix of 0.8 mm diameter. f Bonding procedures were carried out. The self-etching adhesive system was applied and the matrix was placed. After the light curing, the composite resin was placed and then light-cured. g The micro-shear bond test was carried out
Laser device and irradiation
The dentin disks were randomly assigned in nine groups (n = 10), as shown in Table 1.
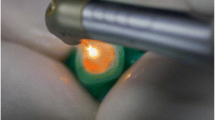
All groups, except the control (G1), were irradiated with dentin disks of approximately 2-mm thick were obtained. The Er:YAG laser (Osada, Tokyo, Japan) works with a wavelength of 2.94 μm. Regarding the handpiece used (HPER-S), the energy delivered at the end of the tip was 30% lower than that depicted on the equipment displayFootnote 1. Therefore, the groups irradiated with 150 and 70 mJ were, in fact, irradiated with 105 and 49 mJ, respectively. When using the handpiece at a non-contact mode, the laser beam was delivered at a work distance of 10 mm. The laser irradiation was performed on the dentin surface for 52 s, scanning the surface in both directions (vertical and horizontal) under water cooling (5.0 ml/mm). The irradiation was performed by hand, screening the dentin surface with a uniform motion. The handpiece was fixed on a metallic device for micrometric movements for which the angles of 1–180° were depicted.
Bonding procedures
The bonding and restorative procedures adhered strictly to the manufacturer’s instructions. The bonding system used was the Clearfil SE Bond System (Kuraray Co, Osaka, Japan), which includes a self-etching primer and a bonding agent. All dentin disks (G1–G9) were treated with Clearfil SE Bond primer for 20 s and dried. The Clearfil SE Bond was applied, air-thinned and light-cured for 20 s.
Before light-curing the bonding resin, an iris was mounted on the dentin surface to restrict the bonding area. This iris was cut from microbore Tygon tubing (R-3603, Norton Performance Plastic, Cleveland, USA) with an internal diameter and a height of approximately 0.8 and 0.5 mm, respectively. A hybrid restorative resin composite, A3 shade (Clearfil AP-X, Kuraray), was placed into the iris and a clear cellophane sheet was placed over the resin and pressed gently. The resin was then light-cured for 40 s. In this manner, very small cylinders of resin of approximately 0.8 mm in diameter and 0.5 mm in height were bonded to the surface [16].
The specimens were stored at room temperature (23°C) for 1 h before removing the Tygon tubing. Then, they were stored in water at 37°C for 24 h.
Micro-shear bond test
After 24 h, the dentin disks were adhered with a cyanoacrylate adhesive (Zapit Base, Dental Ventures of America) that, in turn, was placed in a universal testing machine (Ez-test, 500 N, Shimazu, Kioto, Japan) for micro-shear bond testing. A thin wire (diameter, 0.20 mm) was looped around the resin cylinder, making contact through half its circumference, and was gently held flush against the resin/dentin interface. A shear force was applied to each specimen at a crosshead speed of 1.0 mm/min until failure occurred.
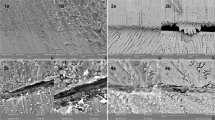
SEM evaluation
For the surface morphology analysis, 27 dentin disks (n = 3) were treated in the same manner as in the micro-shear bond test. After bonding procedures, all specimens were analyzed under scanning electron microscopy (SEM; JXA840, Jeol, Tokyo, Japan), so that the surface morphological changes could be identified.
After laser irradiation and bonding procedures, the dentin samples were given an additional 60-s acetone rinse for the removal of any crystals or other residue from the primer. Finally, the surface was sputter-coated with gold and observed under SEM.
Statistical analysis
The data from the MSBT were statistically analyzed using two-way ANOVA and multiple comparison test. The analyses were performed using the Stat View J-4.5 for Windows. Statistical significance was defined as p < 0.05.
Results
Micro-shear bond test
MSBS was significantly influenced by the treatment of the dentin surface (p < 0.05), as shown in Table 2. Multiple comparison tests revealed that the use of higher energies and the handpiece in contact with the dentin surface (higher energy densities) yielded MSBS values that were lower than those achieved with the handpiece at a non-contact mode and 70 mJ (lower energy densities), regardless of whether the latter was used at 45 or 90° incidence angles.
For all the experimental groups, the MSBS values obtained between resin and the laser-treated dentin were statistically lower than the control group. However, MSBS values from groups G5 (41.90 MPa) and G9 (41.74 MPa) were similar from that of G1—control group (44.97 MPa).
SEM evaluation
Representative SEM pictures of the morphological aspects of the control group and experimental groups are shown in Figs. 2 and 3, respectively. After the application of the self-etching primer, the samples from groups G2 (Fig. 3a) and G6 (Fig. 3e) exhibited a homogeneous surface with some occluded dentinal tubules. The collagen of the upper surface appeared to be packed and melted, with an appearance similar to that of glazing. In G3 (Fig. 3b) and G7 (Fig. 3f), it was possible to verify more exposed collagen. Tubules presented mineralized peritubular dentin matrix with cuff-like appearance.
Groups G4, G5, G8 and G9 showed opened tubules that appeared to be penetrated by adhesive resin. The smear layer was removed and the collagen exposed. It was observed a reticular aspect of dentinal collagen fibers in both the intertubular zone and at the first part of the peritubular dentin.
Discussion
The present study investigated how the incidence angle of the laser beam can influence the irradiation pattern and the adhesion to dentin by increasing the beam spot size and consequently, decreasing the energy density. Clinically, adhesion with self-etching primers can be compromised by laser parameters. Therefore, professionals should be aware of how laser works and which parameters select for different clinical applications.
A number of studies have been performed to evaluate the bonding ability of adhesives systems to dentin, including tensile and shear bond tests. However, there are still doubts about how laser-treated dentin can bond to adhesive systems. In the present study, bond strengths were assessed by means of a micro-shear bond test that can measure bonding to extremely small areas of substrate [17, 18].
Self-etching primers were used for the bonding procedures because it contains acidic adhesive monomers and water, so that it works as an etchant as well as a primer and thus offers simplification of the clinical procedure [19]. This adhesive system demineralizes and simultaneously infiltrates the dentin to form the hybrid layer [20] and was reported to create a dense and firm hybrid layer after polymerization of the bonding resin, enhancing adhesion to dentin [21].
Although some studies have reported that bond strength of Er:YAG laser-treated dentin was lower than that of non-irradiated dentin [13, 16, 22–24], the use of laser for cavity preparation or dentin conditioning before bonding procedures is expected to enlarge the adhesive area due to the typical flaky structure that dentin exhibits after the laser irradiation [8, 13, 15, 16, 25–27].
In the present study, the groups irradiated with the handpiece in contact with dentin surface (G2, 38.8 J/cm2; G3, 18.1 J/cm2; G6, 37.5 J/cm2; and G7, 17.5 J/cm2) presented a lower bonding quality, as reveled by the MSBS test. It is suggested that the irradiation with the handpiece in contact with the dentin surface and, consequently, with higher energies densities can led to changes on dentin that are not indicated for bonding procedures with the self-etching primers. After the laser irradiation and bonding procedures, the SEM evaluation revealed opened dentinal tubules lined by a slightly melted peritubular dentin, which may have contributed to the non-infiltration of the resin [16, 22, 27]. There was no open collagen matrix necessary for the interdiffusion of the adhesive. With dentinal tubules not fully impregnated by the bonding resin, it had possibly created a weak zone of bonding just below the interface, decreasing the MSBS values. The presence of peritubular dentin after acid etching can be due to the insufficient conditioning effect of the self-etching primer, which presents a weak acidity [28], or due to the possible increase in dentin acid resistance after the laser treatment [16, 29]. Corroborating with our study, Perdigão et al. (1996) [30] reported cuffs residual peritubular dentin matrix and suggested that the resin extension into the region of these tubules probably compromises the resin retention or tubule sealing.
The diffusion of the monomer from the tubule lumina into the surrounding dentin could only occur if the mineralized peritubular dentin matrix was removed by the etching [4]. Once there are no widened dentin tubules, the obstruction of the infiltration of the self-etching primer into the dentin might occur and the primer could not fulfill it’s function to superficial layer of the Er:YAG laser-treated dentin [25]. This possibly justifies the lowest MSBS values obtained in the groups treated with the handpiece at a contact mode and higher energy densities.
Other interesting aspect of the groups irradiated with the handpiece in contact with the surface was the characteristic of the intertubular dentin. It appeared packed and melted, with an aspect similar of that of glazing. Opened collagen matrix was not visible, and the collagen fibrils were not found forming a porous network responsible for the increased porosity of dentin. Some authors [14, 16, 31] have reported that the presence of this fused layer, which lacks interfibrillar spaces, can probably restrict resin diffusion into the subsurface intertubular dentin, resulting in lower shear bond strengths. One important variable responsible for the formation of resin-infiltrated demineralized intertubular dentin by resin is the permeability of the demineralized dentin matrix (i.e., maintenance of collagen fibril separation) [4]. These characteristics were not found for the contact-irradiated groups.
When the restorative procedures were conducted in the specimens prepared with the handpiece at a non-contact mode of irradiation and very low energy densities (G5, 0.67 J/cm2 and G9, 0.72 J/cm2), MSBS values were similar to those from the control group (non-irradiated dentin). Sealing of the tubules entrance was observed due to the penetration of monomers through the branching of dentinal tubules, which seems to be very important for the infiltration of the adhesive towards the deepest demineralized dentin zone [20].
Under SEM evaluation, it was observed that the dentin treated with the handpiece at a non-contact mode (G4, G5, G8, and G9) presented, after the self-etching primer application, dentinal tubules filled with resin suggesting the previous removal of the smear layer and exposed dentinal tubules by the laser irradiation. Regarding that these groups were irradiated with low energy densities (Table 1), it is suggested that the dentin was laser-conditioned and not submitted to a cavity preparation procedure, as revealed by the morphological analysis of the contact-irradiated groups. The collagen has a fibrilar and reticular aspect in both the intertubular and peritubular area. These aspects corroborate with the characteristics of diamond-prepared dentin etched with phosphoric acid [26, 27] and is possibly the one ideal for bonding procedures after laser irradiation.
Although dentin surface immediately after the laser irradiation was not considered in the current study, previous investigations have shown that the dentin irradiation with the handpiece at a contact or non-contact mode leads to different alterations on dentin morphology. For all experimental groups, the incidence angle did not greatly influence the MSBS results. The application of an acidic primer leads to the demineralization of both peritubular and intertubular dentin, resulting on the collagen matrix demineralization. The groups irradiated with 150 mJ also showed lower MSBS values when compared with the groups with the same parameters, but at 70 mJ. This can be attributed to physiochemical changes of the tissue due to the laser energy [16].
Regarding the energies densities evaluated, there was no evidence of charring or cracking of the dentin, emphasizing that minimal thermal damage of surrounding tissues can be expected when continuous water spray is used [9, 15].
Finally, one can conclude that different energy densities can adversely affect the bonding of composites to irradiated dentin. Both the contact/non-contact mode of irradiation and beam angle are directly related to the variation of the energy density. Despite the advances in adhesive dental materials and the achievement of greater bonding to dentin, professionals should be careful when using the Er:YAG laser for dentin irradiation and should not eliminate the etching step until further evidence-based studies report safe and effective parameters of erbium lasers for treating dentin surface.
Notes
The energy delivered at the end of the tip was measured with a power meter (FieldMaster, Coherent, USA) before the laser irradiation.
References
Pashley DH (1990) Interaction of dental materials with dentin. Trans Acad Dent Mat 3:55–73
Degrange M, Attal JP, Theimer K et al (1993) In vitro tests of dentin bonding systems. In: Vanherle G, Degrange M, Willems G (eds) State of the art on direct posterior filling materials and dentin bonding. Van der Poorten, Belgium, pp 205–225
Yoshiyama M, Carvalho R, Sano H, Horner JA, Brewer PD, Pashley DH (1996) Regional bond strengths of resins to human root dentin. J Dent 24:435–442
Prati C, Chersoni S, Mongiorgi R, Pashley DH (1998) Resin-infiltrated dentin layer formation of new bonding systems. Oper Dent 23:185–194
Buonocore MG (1995) A simple method of increasing the adhesion of acrylic filling materials to enamel surfaces. J Dent Res 34:849–853
Hibst R (2002) Lasers for caries removal and cavity preparation: state of the art and future directions. J Oral Laser Appl 2:203–212
Hibst R, Keller U (1989) Experimental studies of the application of the ER:YAG laser on the dental hard substances: I measurement of the ablation rate. Lasers Surg Med 9:338–344
Keller U, Hibst R (1989) Experimental studies of the application of the Er:YAG laser on the dental hard substances: II light microscopic and SEM investigations. Lasers Surg Med 9:345–351
Hossain M, Nakamura Y, Yamada Y, Kimura Y, Nakamura G, Matsumoto K (1999) Ablation depths and morphological changes in human enamel and dentin after Er:YAG laser irradiation with or without water mist. J Clin Laser Med Sur 17:105–109
Visuri SR, Gilbert JL, Wright DD, Wigdor HA, Walsh JT Jr (1996) Shear strength of composite bonded to Er:YAG laser-prepared dentin. J Dent Res 75:599–605
Niu W, Eto J, Kimura Y, Takeda FH, Matsumoto K (1998) A study on microleakage after resin filling of Class V cavities prepared by Er:YAG laser. J Clin Laser Med Sur 16:227–231
Wright GZ, McConnel RJ, Keller U (1993) Microleakage of Class V composite restorations prepared conventionally with those prepared with an Er:YAG laser: a pilot study. Pediatr Dent 15:425–426
Aoki A, Ishikawa I, Yamada T, Otsuki M, Watanabe H, Tagami J, Ando Y, Yamamoto H (1998) Comparison between Er:YAG laser and conventional technique for root caries treatment in vitro. J Dent Res 77:1404–1441
Ceballos L, Toledano M, Osorio R, Tay FR, Marshall GW (2002) Bonding to Er–YAG-laser-treated dentin. J Dent Res 8:119–122
Matsumoto K, Hossain M, Tsuzuki N, Yamada Y (2003) Morphological and compositional changes of human dentin after Er:YAG laser irradiation. J Oral Laser Appl 3:15–20
Giachetti L, Russo DS, Scarpelli F, Vitale M (2004) SEM analysis of dentin treated with the Er:YAG laser: a pilot study of the consequences resulting from laser use on adhesion mechanisms. J Clin Laser Med Sur 22:35–41
Shimada Y, Antonucci JM, Schumacher GE et al (1999) Effects of regional tooth structure and sectioning orientation on micro-shear bond strength. In: Tagami J, Toledano M, Prati C (eds) Advanced adhesive dentistry, International Kuraray Symposium, Tokyo, pp 91–103
Shimada Y, Kikushima D, Tagami J (2002) Micro-shear bond strength of resin-bonding systems to cervical enamel. Am J Dent 15:373–377
Toledano M, Osório R, Leonardi G, Rosales-Leal JI, Ceballos L, Cabrerizo-Vilchez MA (2001) Influence of self-etching primer on the resin adhesion to enamel and dentin. Am J Dent 14:205–210
Nakabayashi N, Pashley DH (2000) Hybridization of dental hard tissues, Quintessence, Tokyo
Nakabayashi N (1991) Dentinal bonding mechanisms. Quintessence Int 22:73–74
Kataumi M, Nakajima M, Yamada T, Tagami J (1998) Tensile bond strength and SEM evaluation of Er:YAG laser irradiated dentin using dentin adhesive. Dent Mat J 17:125–138
Armengol V, Jean A, Weiss P, Hamel H (1999) Comparative in vitro study of the bond strength of composite to enamel and dentin obtained with laser irradiation or acid etch. Lasers Med Sci 14:207–215
Martínez-Insua A, Dominguez LS, Rivera FG, Santana-Penin UA (2000) Differences on bonding to acid-etched or Er:YAG-laser-treated enamel and dentin surfaces. J Prosthet Dent 84:280–288
Eguro T, Maeda T, Otsuki M, Nishimura Y, Katsumi I, Tanaka H (2002) Adhesion of Er:YAG laser-irradiated dentin and composite resins: application of various treatments on irradiated surface. Lasers Surg Med 30:267–272
Benazzato P, Stefani A (2003) The effect of Er:YAG laser treatment on dentin collagen: an SEM investigation. J Oral Laser Appl 3:79–81
Schein MT, Bocangel JS, Nogueira GEC, Schein PAL (2003) SEM evaluation of the interaction pattern between dentin and resin after cavity preparation using Er:YAG laser. J Dent 31:127–135
Torii Y, Itou K, Nishitani Y, Ishikawa K, Suzuki K (2002) Effect of phosphoric acid etching prior to self-etching primer application on adhesion of resin composite to enamel and dentin. Am J Dent 15:305–308
Hossain M, Nakamura Y, Kimura Y, Yamada Y, Ito M, Matsumoto K (2000) Caries-preventive effect of Er:YAG laser irradiation with or without water mist. J Clin Laser Med Sur 18:61–65
Perdigão J, Lambrechts P, Van Meerbeek B, Tomé AR, Vanherle G, Lopes AB (1996) Morphological field emission–SEM study of the effect of six phosphoric acid etching agents on human dentin. Dent Mat 12:262–271
Ceballos L, Osorio R, Toledano M, Marshall GW (2001) Microleakage of composite restorations after acid or Er:YAG laser cavity treatments. Dent Mater 17:340–346
Acknowledgment
The authors would like to express their gratitude to the Tokyo Medical and Dental University and to the Committee of International Cooperation of the University of São Paulo (CCInt/USP) for making the present study feasible. In addition, we would like to thank the Kuraray (Japan), Kota (Brazil), and the State of São Paulo Research Foundation / FAPESP (São Paulo, Brazil).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
de Carvalho, R.C.R., de Freitas, P.M., Otsuki, M. et al. Micro-shear bond strength of Er:YAG-laser-treated dentin. Lasers Med Sci 23, 117–124 (2008). https://doi.org/10.1007/s10103-006-0434-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-006-0434-6