Abstract
Extended-spectrum cephalosporin-resistant Escherichia coli (ESCREC) are a growing threat. Leading ESCREC lineages include sequence type ST131, especially its (blaCTX-M-15-associated) H30Rx subclone and (blaCTX-M-27-associated) C1-M27 subset within the H30R1 subclone. The comparative activity against such strains of alternative antimicrobial agents, including the recently developed aminoglycoside plazomicin, is undefined, so was investigated here. We assessed plazomicin and 11 comparators for activity against 216 well-characterized ESCREC isolates (Minnesota, 2012–2017) and then compared broth microdilution MICs with phylogenetic and clonal background, beta-lactamase genotype (blaCTX-M; group 1 and 9 variants), and co-resistance. Percent susceptible was > 99% for plazomicin, meropenem, imipenem, and tigecycline; 96–98% for amikacin and ertapenem; and ≤ 75% for the remaining comparators. For most comparators, MICs varied significantly in relation to multiple bacterial characteristics, in agent-specific patterns. By contrast, for plazomicin, the only bacterial characteristic significantly associated with MICs was ST131 subclone: plazomicin MICs were lowest among O16 ST131 isolates and highest among ST131-H30R1 C1-M27 subclone isolates. Additionally, plazomicin MICs varied significantly in relation to resistance vs. susceptibility to comparator agents only for amikacin and levofloxacin. For most study agents, antimicrobial activity against ESCREC varied extensively in relation to multiple bacterial characteristics, including clonal background, whereas for plazomicin, it varied only by ST131 subclone (C1-M27 isolates least susceptible, O16 isolates most susceptible). These findings support plazomicin as a reliable alternative for treating ESCREC infections and urge continued attention to the C1-M27 ST131 subclone.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Extended-spectrum cephalosporin-resistant Escherichia coli (ESCREC) are a serious and growing threat [1], resulting in increasing use of carbapenems for empirical and definitive therapy [2]. Emerging carbapenem resistance in E. coli creates a need to identify suitable non-carbapenem treatment options for ESCREC [3].
Plazomicin (PLZ) is a novel aminoglycoside antibiotic that was approved recently by the US Food and Drug Administration (FDA) for treating complicated urinary tract infection and pyelonephritis [4,5,6,7]. It inhibits protein synthesis by binding to the 30S ribosomal subunit. Its Gram-negative spectrum includes extended-spectrum β-lactamase (ESBL)-producing Enterobacteriaceae, carbapenem-resistant Enterobacteriaceae (CRE), and organisms with aminoglycoside-modifying enzymes [8,9,10,11]. Thus, PLZ may be a carbapenem-sparing alternative for ESCREC. However, PLZ’s activity specifically against ESCREC has received limited study, especially in relation to clonal background and ESBL genotype.
Antimicrobial resistance in E. coli is highly clonal [12, 13]. The leading ESCREC clonal lineage currently is sequence type ST131 [14, 15], which has multiple distinctive clonal subsets, or subclones [16,17,18]. Of these, H30R, which likewise has multiple important subsets, overall is the most extensively antimicrobial resistant and epidemiologically successful [14].
All H30R members are densely fluoroquinolone resistant, due to four canonical amino acid replacement mutations in gyrA and parC [19]. H30R1 has two main sublineages, H30R1 and H30Rx. H30Rx was recognized first [20], due to its association with the (globally dominant) extended-spectrum beta-lactamase (ESBL)-encoding gene blaCTX-M-15. However, H30R1, the historically “less resistant” sister clade to H30Rx, now has an emerging subclone, C1-M27, that is closely associated with blaCTX-M-27 and blaCTX-M-14 [21]. Unlike blaCTX-M-15 (from blaCTX-M group 1), these two bla variants are from blaCTX-M group 9. Additionally, some non-H30R ST131 strains—especially within the O16-fimH41 subclone (or clade A)—have horizontally acquired ESBL-encoding genes [16,17,18, 22].
Here, we sought to clarify the activity of PLZ against recent ESCREC isolates in comparison with conventional agents, including carbapenems, and in relation to other bacterial characteristics. For that, we determined broth microdilution MICs to PLZ among 216 unique-by-episode ESCREC isolates from the Minneapolis Veterans Affairs Health Care System (MVAHCS) and then compared the MICs statistically with bacterial characteristics, including phylogenetic group, clonal background, blaCTX-M genotype, and susceptibility to 11 relevant comparators.
Methods
Study setting
The MVAHCS is a teaching hospital that provides a full range of patient care services. The MVAHCS clinical microbiology laboratory processes specimens from the Minneapolis campus and 14 outlying community clinics across MN and western WI. Patients are mostly older men, many with multiple chronic medical conditions.
Isolates
From May 2012 through December 2017, with approval from the Institutional Review Board (i.e., Ethics Committee), the research laboratory prospectively collected consecutive E. coli clinical isolates from the MVAHCS clinical microbiology laboratory. In the research laboratory, isolates were stored at −70 C in LB broth supplemented with 20% glycerol.
During the approximately 5.5-year study period, 6324 total E. coli isolates were collected. The clinical laboratory found 267 (4.2%) of these to be resistant or intermediate to ceftazidime and/or ceftriaxone, according to a VITEK-2 instrument (bioMérieux, Durham, NC) and then-current MIC breakpoints, so here were classified as ESCREC. Exclusion of repeat isolates from the same patient within 30 days after an initial isolate left 216 putative unique-by-episode ESCREC isolates as the study population.
By specimen type, the 216 ESCREC study isolates were from (no. of isolates, % of 216) urine (173, 80%); blood (21, 10%); wound (10, 5%); sputum (4, 1.9%); bone (3, 1.4%); fluid (2, 0.9%); and tissue, swab, and other (each: 1, 0.5%). They were derived from 138 unique source patients, with ages ranging from 24 to > 90 years (median, 68 years); 113 (82%) were male.
Susceptibility testing
Isolates underwent standardized broth microdilution MIC determinations with PLZ and, as reported elsewhere [23], 11 comparators, including ertapenem (ETP), imipenem (IPM), and meropenem (MEM), plus eight non-carbapenem agents, i.e., amikacin (AMK), ceftazidime (CAZ), colistin (CLS), gentamicin (GEN), levofloxacin (LVX), minocycline (MIN), tigecycline (TGC), and piperacillin/tazobactam (TZP). Test methods and reference strains were per the Clinical Laboratory Standards Institute (CLSI) [24]. The tazobactam concentration was fixed at 4 mg/L. Interpretive criteria were per CLSI (all agents except TGC and PLZ) or the FDA (TGC and PLZ). Note: the European Committee on Antimicrobial Susceptibility Testing (EUCAST) specifies different MIC breakpoints (mg/L) than does CLSI for GEN (EUCAST, ≥ 4 resistant, vs. CLSI, 8 intermediate) and AMK (EUCAST, ≥ 16 resistant, vs. CLSI, 32 intermediate). Here, isolates with intermediate MIC values were considered resistant.
Molecular typing
As reported elsewhere [23], established PCR-based assays were used to identify E. coli phylogroups A, B1, B2, C, D, E, and F [25]; selected STs associated with multidrug resistance, recent emergence, and/or extraintestinal infections generally [15, 26, 27]; ST131 subsets O16 (clade A), H30R, C1-M27, and H30Rx [27,28,29]; and blaCTX-M. Isolates with blaCTX-M (according to universal blaCTX-M primers [30]) were further characterized with group 1- and group 9-specific multiplex PCR analysis [30].
Fluoroquinolone-resistant ST131-H30 isolates were classified operationally as H30R; H30R isolates that tested negative for H30Rx were classified as H30R1 [27, 28]. All H30R1 isolates were tested for a C1-M27 subclone-specific prophage marker [29] and based on the result were classified operationally as (H30R1) C1-M27 or (non-C1-M27) H30R1.
Statistical methods
Statistical analysis was limited to variables present in ≥ 2 isolates (≥ 1.0 % of 216). Comparisons involving dichotomous variables were tested using chi-squared tests, including an “N-1” chi-squared test for two-group comparisons [31]. Comparisons involving MIC distributions were tested using the Mann-Whitney or Kruskal-Wallis test (two-tailed), due to the nonparametric distribution of the data. Off-scale high or low MICs were analyzed statistically as representing the dilution step above or below (as appropriate) the tested dilution range. For PLZ, MICs were analyzed in relation to susceptibility vs. resistance to each comparator agent that was represented by sufficient resistant (or susceptible) isolates to qualify for statistical analysis.
Summary statistics used for MIC values included the MICmin (lowest detected MIC), MIC50, MIC90, and MICmax (highest detected MIC). Additionally, for PLZ, GEN, and AMK, cumulative percent MIC distributions were tabulated. Throughout, the criterion for statistical significance was P < 0.05, without adjustment for multiple comparisons, given the study’s exploratory nature. For MIC comparisons that yielded a statistically significant difference despite similar or identical MIC summary statistics, mean MIC ranks (note: not mean MICs) were used to clarify the direction of the difference.
Results
Overall susceptibility
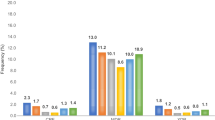
Of the 12 study agents, four (PLZ, IMP, MEM, and TGC) exhibited > 99% susceptibility (Table 1). These were followed, in descending order, by AMK (98%), ETP (96%), MIN (75%), GEN (64%), CAZ (36%), and LVX (12%). No isolate—by definition (per CLSI)—was susceptible to CL (Table 1). PLZ exhibited the lowest MIC50/MIC90 ratio (i.e., 4) of all study agents excepting LVX (MIC50 and MIC90 both > 8 mg/L; ratio uninterpretable).
Phylogroups
PLZ MICs did not vary significantly across phylogroups, by contrast with MICs for all but three comparators (IPM, GEN, AMK) Suppl. Table (1). The PLZ MIC50 was 1 mg/L for all phylogroups except phylogroup C (0.5 mg/L), and the PLZ MIC90 was consistently 2 mg/L. The cumulative percent MIC distribution for PLZ, GEN, and AMK likewise showed minor variation across phylogroup Suppl. Table (2).
STs
PLZ MICs also did not vary significantly across the four most prevalent STs and all other STs combined, by contrast with MICs all but four of the comparators (IPM, GEN, AMK, TGC) (Table 2). Within each ST category, the PLZ MIC50 was consistently 1 mg/L and the PLZ MIC90 consistently 2 mg/L. The cumulative percent MIC distribution for PLZ, GEN, and AMK showed minor variation across STs (Supplemental Table 3).
ST131 subclone
By contrast with phylogroup and ST, PLZ MICs did vary significantly by ST131 subclone status, albeit subtly, as reflected in mean MIC ranks (Table 2 footnote) and the cumulative percent MIC distribution (Supplemental Table 4), not the MIC50 or MIC90 (Table 2). Specifically, according to mean MIC ranks, PLZ MICs were lowest among the O16 (clade A) ST131 isolates; highest among the (H30R1) C1-M27 ST131 isolates; and intermediate among the non-ST131 isolates, the non-C1-M27 H30R1 isolates, and the H30Rx isolates. Likewise, MICs for all but three comparators (MEM, AMK, TGC) also varied significantly by ST131 subclone status, in agent-specific patterns.
CTX-M genotype
PLZ MICs did not vary significantly by CTX-M status or CTX-M group (Supplemental Table 5). By contrast, MICs did so vary for eight of the 11 comparators (i.e., all but MEM, GEN, and TGC). For these eight agents, MICs were usually higher among CTX-M-positive isolates, and/or CTX-M group 1-positive isolates. The cumulative percent MIC distribution for PLZ, GEN, and AMK illustrated with greater granularity this distinction between GEN (higher MICs among CTX-M and group 1-positive isolates) vs. PLZ and AMK (minimal variation in relation to resistance genotype) (Supplemental Table 6).
Resistance to comparators
PLZ MICs varied significantly with comparator-agent-resistance only for AMK or LVX, in both instances being higher among comparator-resistant isolates (Supplemental Table 7). With AMK, the fact that PLZ MICs were higher among resistant isolates was reflected in the twofold higher MIC50 (2 mg/L, vs. 1 mg/L). By contrast, with LVX, the direction of the difference was evident only from mean MIC ranks (88, LVX-susceptible isolates; vs. 111, LVX-resistant isolates: Supplemental Table 7 footnote).
Discussion
In this study of the activity PLZ and 11 comparators against 216 ESCREC clinical isolates from veterans in relation to bacterial characteristics, PLZ distinguished itself from most or all comparators in multiple respects. These included (i) a very high overall percent susceptible (99.5%); (ii) very similar MIC50 and MIC90 values (only a four-fold difference); (iii) minimal MIC variation in relation to phylogroup, ST, or beta-lactamase genotype; and (iv) subtle but statistically significant MIC variation in relation to ST131 subclone status (lowest among O16 isolates, highest among C1-M27 H30R1 isolates). PLZ MICs were also independent of resistance to comparator agents, except for AMK (possibly due to shared resistance mechanisms [32]) and LVX (possibly due to clonally or genetically linked resistance mechanisms [33]). These findings demonstrate the distinctiveness of PLZ and its preserved activity against even multidrug-resistant ESCREC isolates, and recommend it as a potential non-beta-lactam, carbapenem-sparing alternative for treating ESCREC infections.
The high percent susceptible for most agents obliged comparisons based on MICs rather than percent susceptible. In these analyses, multiple comparator agents—but rarely PLZ—exhibited MIC shifts in relation to each category of variable studied. The observed MIC differences within the susceptible range conceivably could be clinically significant, depending on the site and severity of infection [34,35,36,37], if drug levels at the site were limited by local or systemic factors, or with immune compromise.
The only phylogenetic entity to exhibit comparatively higher PLZ MICs was the recently recognized and emerging C1-M27 subset within ST131-H30R1, which is associated with blaCTX-M-27 and blaCTX-M-14 [21, 29, 38]. The basis for the higher PLZ MICs of C1-M27 isolates is unclear. Conceivably, the same plasmids that carry blaCTX-M-27 may carry genes that encode resistance mechanisms (e.g., ribosomal methyl-transferases or efflux pumps) that raise PLZ MICs, without conferring full resistance.
Study limitations include the single-institution source of the isolates (MVAHCS); the distinctiveness of the veteran population, which may constrain generalizability; the minimal data regarding the source patients and their clinical presentations; the lack of information regarding PLZ resistance mechanisms; and the uncertain therapeutic implications of the MIC data. Study strengths include the relatively large and recent sample, the extensive molecular and phenotypic characterization of the isolates, and the analysis of MICs in relation to multiple bacterial characteristics, including resistance to comparators.
In conclusion, we found that PLZ exhibited activity against recent ESCREC clinical isolates comparable to that of carbapenems and that most bacterial characteristics were unassociated with shifts in the PLZ MIC, by contrast with the extensive associations of these variables with MICs for most comparators. These findings support PLZ as a potential alternative to carbapenems for treating ESCREC infections, largely irrespective of phylogenetic/clonal background or ESBL genotype, and support further attention to PLZ susceptibility within the emerging C1-M27 ST131 subclone.
References
CDC (2019) Antibiotic resistance threats in the United States, 2019. In: U.S. Department of Health and Human Services C (ed)
Hawkey PM, Warren RE, Livermore DM, McNulty CAM, Enoch DA, Otter JA, Wilson PR (2018) Treatment of infections caused by multidrug-resistant Gram-negative bacteria: report of the British Society for Antimicrobial Chemotherapy/Healthcare Infection Society/British Infection Association Joint Working Party. J Antimicrob Chemother 73(suppl 3):iii2–iii78
Fournier D, Chirouze C, Leroy J, Cholley P, Talon D, Plésiat P, Bertrand X (2013) Alternatives to carbapenems in ESBL-producing Escherichia coli infections. Med Mal Infect 43:62–66
Eljaaly K, Alharbi A, Alshehri S, Ortwine JK, Pogue JM (2019) Plazomicin: a novel aminoglycoside for the treatment of resistant Gram-negative bacterial infections. Drugs 79:243–269
Shaeer KM, Zmarlicka MT, Chahine EB, Piccicacco N, Cho JC (2018) Plazomicin: a next-generation aminoglycoside. Pharmacotherapy 31:77–93
Saravolatz LD, Stein GE (2020) Plazomicin: a new aminoglycoside. Clin Infect Dis 70
Wagenlehner F, Cloutier D, Komirenko A, Cebrik D, Krause K, Keepers T, Connolly L, Miller L, Friedland I, Dwyer J, EPIC Study Group (2019) Once-daily plazomicin for complicated urinary tract infections. N Engl J Med 380:729–740
Zhanel G, Lawson C, Zelenitsky S, Findlay B, Schweizer F, Adam H, Walkty A, Rubinstein E, Gin A, Hoban DJ, Lynch J, Karlowsky JA (2012) Comparison of the next-generation aminoglycoside plazomicin to gentamicin, tobramycin and amikacin. Expert Rev Anti-Infect Ther 10:459–473
Walkty A, Baxter H, Denisuik A, Lagacé-Wiens P, Karlowsky J, Hoban D, Zhanel G (2014) In vitro activity of plazomicin against 5,015 Gram-negative and Gram-positive clinical isolates obtained from patients in Canadian hospitals as part of the CANWARD study, 2011–2012. Antimicrob Agents Chemother 58:2554–2563
Zhang Y, Kashikar A, Bush K (2017) In vitro activity of plazomicin against beta-lactamase-producing carbapenem-resistant Enterobacteriaceae (CRE). J Antimicrob Chemother 72:2792–2795
Clark JA, Kulengowski B, Burgess DS (2020) In vitro activity of plazomicin compared to other clinically relevant aminoglycosides in carbapenem-resistant Enterobacteriaceae. Diagn Microbiol Infect Dis 98:115117
Tchesnokova V, Billig M, Chattopadhyay S, Linardopoulou E, Aprikian P, Roberts PL, Skrivankova V, Johnston B, Gileva A, Igusheva I, Tolland A, Riddell R, Rogers P, Qin X, Butler-Wu S, Cookson BT, Fang FC, Kahl B, Price LB, Weissman SJ, Limaye A, Scholes D, Johnson JR, Sokurenko EV (2013) Predictive diagnostics for Escherichia coli infections based on the clonal association of antimicrobial resistance and clinical outcome. J Clin Microbiol 51:2991–2999
Tchesnokova V, Avagyan H, Billig M, Chattopadhyay S, Aprikian P, Chan D, Pseunova J, Rechkina E, Riddell K, Scholes D, Fang F, Johnson J, Sokurenko E (2016) A novel 7-single nucleotide polymorphism-based clonotyping test allows rapid prediction of antimicrobial susceptibility of extraintestinal Escherichia coli directly from urine specimens. Open Forum Infect Dis 3:fw002
Johnson J, Porter S, Thuras P, Castanheira M (2017) The pandemic H30 subclone of sequence type 131 (ST131) is the leading cause of multidrug-resistant Escherichia coli infections in the United States (2011-2012). Open Forum Infect Dis 4:ofx089
Johnson JR, Johnston BD, Porter SB, Clabots C, Bender TL, Thuras P, Trott DJ, Cobbold R, Mollinger J, Ferrieri P, Drawz S, Banerjee R (2019) Rapid emergence, subsidence, and molecular detection of Escherichia coli sequence type 1193-fimH64 (ST1193-H64), a new disseminated multidrug-resistant commensal and extraintestinal pathogen. J Clin Microbiol 57:e01664–e01618
Ben Zakour N, Alsheich-Hussain A, Ashcroft M, Nhu N, Roberts L, Stanton-Cook M, Schembri MA, Beatson SA (2016) Sequential acquisition of virulence and fluoroquinolone resistance has shaped the evolution of Escherichia coli ST131. mBio 7:e00347–e00316
Stoesser N, Sheppard AE, Pankhurst L, de Maio N, Moore C, Sebra R, Turner P, Anson L, Kasarkis A, Batty E, Kos V, Wilson D, Phetsouvanh R, Wyllie D, Sokurenko E, Manges A, Johnson TJ, Price LB, Peto T, Johnson J, Didelot X, Walker AS, Crook D The Modernizing Medical Microbiology Informatics Group (MMMIG) (2016) Evolutionary history of the global emergence of the Escherichia coli epidemic clone ST131. mBio 7:e02162–e02115
Price LB, Johnson JR, Aziz M, Clabots C, Johnston B, Tchesnokova V, Nordstrom L, Billig M, Chattopadhyay S, Stegger M, Andersen PS, Pearson T, Riddell K, Rogers P, Scholes D, Kahl B, Keim P, Sokurenko EV (2013) The epidemic of ESBL-producing Escherichiae coli ST131 is driven by a single highly virulent subclone, H30-Rx. mBio 6:e00377–e00313
Johnson JR, Tchesnokova V, Johnston B, Clabots C, Roberts PL, Billig M, Riddel K, Rogers P, Qin X, Butler-Wu S, Price LB, Aziz M, Nicolas-Chanoine M, Debroy C, Robicsek A, Hansen G, Urban C, Platell JL, Trott DJ, Zhanel G, Weissman SJ, Cookson B, Fang F, Limaye AP, Scholes D, Chattopadhyay S, Hooper DC, Sokurenko E (2013) Abrupt emergence of a single dominant multi-drug-resistant strain of Escherichia coli. J Infect Dis 207:919–928
Nicolas-Chanoine M-H, Blanco J, Leflon-Guibout V, Demarty R, Alonso MP, Caniça MM, Park Y-J, Lavigne J-P, Pitout J, Johnson JR (2008) Intercontinental emergence of Escherichia coli clone O25:H4-ST131 producing CTX-M-15. J Antimicrob Chemother 61(2):273–281
Matsumura Y, Johnson JR, Yamamoto M, Nagao M, Tanaka K, Takakura S, Ichiyama S, Kyoto-Shiga Clinical Microbiology Study Group (2015) CTX-M-27- and CTX-M-14-producing, ciprofloxacin-resistant Escherichia coli of the H30 subclonal group within ST131 drive a Japanese regional ESBL epidemic. J Antimicrob Chemother 70:1639–1649
McNally A, Oren Y, Kelly D, Pascoe B, Dunn S, Sreecharan T, Vehkala M, Välimäki N, Prentice M, Ashour A, Avram O, Pupko T, Dobrindt U, Literak I, Guenther S, Schaufler K, Wieler LH, Zhiyong Z, Sheppard SK, McInerney JO, Corander J (2016) Combined analysis of variation in core, accessory and regulatory genome regions provides a super-resolution view into the evolution of bacterial populations. PLoS Genet 12:e1006280
Johnston B, Thuras P, Porter S, Anacker M, VonBank B, Vagnone Snippes P, Witwer M, Castanheira M, Johnson J (2020) Activity of cefiderocol, ceftazidime-avibactam, and eravacycline against carbapenem-resistant Escherichia coli isolates from the United States and international sites in relation to clonal background, resistance genes, coresistance, and region. Antimicrob Agents Chemother 64:e00797–e00720
Clinical and Laboratory Standards Institute (2020) M100: Performance standards for antimicrobial susceptibility testing, 30th edn. CLSI, Wayne, PA
Clermont O, Christenson JK, Denamur E, Gordon DM (2012) The Clermont Escherichia coli phylo-typing method revisited: improvement of specificity and detection of new phylo-groups. Environ Microbiol Rep 5:58–65
Clermont O, Christenson JK, Daubie A, Gordon DM, Denamur E (2014) Development of an allele-specific PCR for Escherichia coli B2 sub-typing, a rapid and easy to perform substitute of multilocus sequence typing. J Microbiol Methods 101:24–27
Johnson JR, Porter S, Thuras P, Castanheira M (2017) Epidemic emergence in the United States of Escherichia coli sequence type 131-H30 (ST131-H30), 2000-2009. Antimicrob Agents Chemother 61pii:e00732–e00717
Johnson JR, Davis G, Clabots C, Johnston BD, Porter S, Debroy C, Pomputius W, Ender PT, Cooperstock M, Slater BS, Banerjee R, Miller S, Kisiela D, Sokurenko E, Aziz M, Price LB (2016) Household clustering of Escherichia coli sequence type 131 clinical and fecal isolates according to whole genome sequence analysis. Open Forum Infect Dis 3:ofw129
Birgy A, Bidet P, Levy C, Sobral E, Cohen R, Bonacorsi S (2017) CTX-M-27–producing Escherichia coli of sequence type 131 and clade C1-M27, France. Emerg Infect Dis 23:885
Saladin M, Cao VT, Lambert T, Donay JL, Herrmann JL, Ould-Hocine Z, Verdet C, Delisle F, Philippon A, Arlet G (2002) Diversity of CTX-M beta-lactamases and their promoter regions from Enterobacteriaceae isolated in three Parisian hospitals. FEMS Microbiol Lett 209:161–168
Campbell I (2007) Chi-squared and Fisher-Irwin tests of two-by-two tables with small sample recommendations. Stat Med 26:3661–3675
Livermore D, Mushtaq S, Warner M, Zhang J-C, Maharjan S, Doumith M, Woodford N (2011) Activity of aminoglycosides, including ACHN-490, against carbapenem-resistant Enterobacteriaceae isolates. J Antimicrob Chemother 66:48–53
Doi Y, Wachino J, Arakawa Y (2016) Aminoglycoside resistance: the emergence of acquired 16S ribosomal RNA methyltransferases. Infect Dis Clin N Am 30:523–537
Nau R, Sörgel F, Eiffert H (2010) Penetration of drugs through the blood-cerebrospinal fluid/blood-brain barrier for treatment of central nervous system Infections. Clin Microbiol Rev 23:858–883
Luaces-Rodríguez A, González-Barcia M, José Blanco-Teijeiro M, Gil-Martínez M, Gonzalez F, Gómez-Ulla F, Lamas M-J, Otero-Espinar F-J, Fernández-Ferreiro A (2018) Review of intraocular pharmacokinetics of anti-infectives commonly used in the treatment of infectious endophthalmitis. Pharmaceutics 10:66
Lipsky B, Berendt A, Cornia P, Pile J, Peters E, Armstrong D, Deery H, Embil J, Joseph W, Karchmer A, Pinzur M, Senneville E (2012) 2012 Infectious Diseases Society of America clinical practice guideline for the diagnosis and treatment of diabetic foot infections. Clin Infect Dis 54:132–173
Charalabopoulos K, Karachalios G, Baltogiannis D, Charalabopoulos A, Giannakopoulos X, Sofikitis N (2003) Penetration of antimicrobial agents into the prostate. Chemother 49:269–279
Matsumura Y, Pitout J, Gommi R, Matsuda T, Noguchi T, Yamamoto M, Peirano G, DeVinney R, Bradfor PA, Motyl M, Tanaka M, Nagao M, Takakura S, Ichiyama S (2016) Global Escherichia coli sequence type 131 clade with blaCTX-M-27 gene. Emerg Infect Dis 22:1900–1907
Acknowledgements
The MVAMC Clinical Microbiology Laboratory provided the study isolates.
Availability of data and material
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
Funding
This work was supported by an investigator-initiated grant from Cipla/Achaogen. This work was also supported by Office of Research and Development, Department of Veterans Affairs and the National Institute of Allergy and Infectious Diseases of the NIH (Antibacterial Resistance Leadership Group, award number UM1AI104681) (JRJ). The sponsors had no role in study design, data collection, data analysis, writing the manuscript, or the decision to publish.
Author information
Authors and Affiliations
Contributions
1. Brian Johnston: Data collection and validation, laboratory procedures, data analysis, construction of tables, and manuscript writing and editing
2. Paul Thuras: Statistical analysis
3. Stephen B. Porter: Isolate collection, data collection, and manuscript editing
4. Connie Clabots: Isolate collection, data collection, and manuscript editing
5. James R. Johnson: Concept, funding, project oversight, and manuscript drafting and editing
Corresponding author
Ethics declarations
Ethics approval (include appropriate approvals or waivers): The study was approved by the MVAMC Institutional Review Board.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
James R. Johnson has had grants and/or consultancies with Allergan/Actavis, Cipla/Achaogen, Janssen/Crucell, Melinta/The Medicines Company, Merck, Shionogi, Syntiron, and Tetraphase. The other authors report no financial conflicts of interest.
Disclaimer
The opinions expressed here are strictly those of the authors and do not necessarily represent those of the Department of Veteran Affairs or the authors' institutions.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Johnston, B.D., Thuras, P., Porter, S.B. et al. Comparative activity of plazomicin against extended-spectrum cephalosporin-resistant Escherichia coli clinical isolates (2012–2017) in relation to phylogenetic background, sequence type 131 subclones, blaCTX-M genotype, and resistance to comparator agents. Eur J Clin Microbiol Infect Dis 40, 2069–2075 (2021). https://doi.org/10.1007/s10096-021-04256-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-021-04256-9