Abstract
Antimicrobial resistance among Enterobacteriaceae has been increasing globally especially due to extended-spectrum-β-lactamases (ESBLs), which typically necessitate the use of carbapenems for treatment of serious infections. Emerging carbapenem-resistant Enterobacteriaceae further complicate therapy. As part of the Study for Monitoring Antimicrobial Resistance Trends (SMART), this analysis examined the recent activity of a key carbapenem (ertapenem) and other important therapeutic options against Enterobacteriaceae. From 2012 to 2016, 224 hospitals in 57 countries collected up to 100 consecutive gram-negative bacilli from intra-abdominal (IAI) and 50 from urinary tract infections (UTI) per year, totaling 106,300 Enterobacteriaceae isolates. Susceptibility was determined using CLSI broth microdilution and breakpoints. Although statistically significant decreasing trends in ertapenem activity against Enterobacteriaceae were found in all regions except Middle East, the actual size of the decreases was < 3 percentage points, and susceptibility in 2015–2016 remained ca. 90% or higher, ranging from 89.5% in Asia to 97.3% in US/Canada. Of the comparators, only amikacin exceeded these results. Ertapenem was active against > 90% of isolates with ESBL phenotype from Latin America, Middle East, South Pacific, and US/Canada, and against > 80% of MDR isolates in all regions except Africa (72.9%), Asia (75.1%), and Europe (78.0%). Only imipenem, amikacin, and colistin exceeded these rates. Ertapenem, which is popular among clinicians due to its convenient once-daily dosing schedule and favorable safety and tolerability profile, remains highly active against Enterobacteriaceae from IAI and UTI, even as ESBLs and other resistance mechanisms limit therapeutic options, but continued susceptibility testing for surveillance and individual patients is important.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The emergence and spread of extended-spectrum β-lactamases (ESBL) and carbapenemases, as well as a multitude of other evolving antibiotic resistance mechanisms, such as drug efflux and changes in membrane permeability, have led to an increase in antimicrobial resistance, which the World Health Organization (WHO) has identified as a problem so serious that it “threatens the achievements of modern medicine” [1]. Correspondingly, multi-drug resistance (MDR) has been increasing, drastically limiting treatment options for these strains. This is a critical problem for empirical therapy, as multi-drug resistance greatly increases the risk that the antibiotic used will be ineffective, resulting in increased mortality, length of hospital stay, and cost in patients with serious infections [2]. For these reasons, knowledge of current resistance patterns including MDR rates is important in order to reduce the risk of using ineffective antibiotics as well as avoid the over-use of newer last-resort agents.
Ertapenem is a group 1 carbapenem that was launched in 2002 and was described in two reviews from 2005 as having excellent efficacy for the treatment of a variety of community-acquired infections in hospitalized patients as well as for outpatient parenteral antimicrobial therapy, especially for those infections with ESBL-positive Enterobacteriaceae [3, 4]. The global Study for Monitoring Antimicrobial Resistance Trends (SMART) has monitored the in vitro susceptibility to ertapenem and comparators of gram-negative organisms from intra-abdominal infections (IAI) since 2002 and from urinary tract infections (UTI) since 2009 [5]. In this report, we use Enterobacteriaceae isolates collected as part of the SMART surveillance program to examine trends in the susceptibility to ertapenem and comparators over the past 5 years and to assess whether its activity has been maintained against a large, global collection of recent isolates, including ESBL-positive and MDR strains. Because antimicrobial activity varies greatly across global regions and is higher in certain patient settings, we examine the susceptibility patterns for each of seven global regions, as well as for subsets of isolates from hospital-associated infections and from ICU patients.
Materials and methods
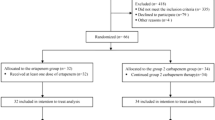
For the SMART program, participating hospital laboratories each collected up to 100 consecutive aerobic or facultatively anaerobic gram-negative isolates from intra-abdominal infections (IAI) and up to 50 isolates from urinary tract infections (UTI) per year. Only one isolate per patient per species was accepted. After species identification using local site procedures, all isolates except those from China and India were sent to one of two central laboratories (International Health Management Associates, Inc. [IHMA], Schaumburg, IL, USA, and IHMA Europe Sàrl, Epalinges, Switzerland), where their identities were confirmed using MALDI-TOF spectrometry (Bruker Daltonics, Billerica, MA, USA). From 2012 to 2016, 224 hospital laboratories from 57 countries collected 121,892 isolates of gram-negative bacilli from IAI (n = 76,474) and UTI (n = 45,418). Enterobacteriaceae accounted for 106,300 isolates (85.2% of all IAI isolates [65,163/76,474] and 90.6% of all UTI isolates [41,137/45,418]). Online Resource 1 shows the number of Enterobacteriaceae isolates collected from the participating countries in each region.
Antimicrobial susceptibility testing was performed at the IHMA labs using the Clinical and Laboratory Standards Institute (CLSI) broth microdilution method [6, 7] with custom dehydrated panels manufactured by MicroScan (Beckman Coulter, Inc., West Sacramento, CA) in 2012 to 2014 and by Trek Diagnostic Systems (Thermo Scientific, Independence, OH) in 2015 and 2016. Because of export restrictions, isolates from China and India were tested in a central laboratory in the respective countries using the identical protocol for susceptibility testing. MICs were interpreted as susceptible, intermediate, or resistant using CLSI breakpoints, except colistin, for which EUCAST breakpoints were used [7, 8]. Escherichia coli, Klebsiella pneumoniae, K. oxytoca, and Proteus mirabilis were screened for an ESBL phenotype (ceftazidime or cefotaxime MIC of > 1 μg/ml) and confirmed as ESBL producers using combination clavulanic acid based testing according to the CLSI method (broth microdilution until 2015 and disk diffusion in 2016) [7]. ESBL phenotype determination was not available for 26% of isolates from China (888/3371) and for 41% of isolates from India (386/950); consequently, all isolates from these two countries were excluded from ESBL rate calculations and from the analysis of susceptibility of ESBL-positive isolates (but were included in all other analyses). Multidrug-resistance was defined as non-susceptibility (intermediate or resistant) to any three or more agents of eight sentinel drugs (amikacin, aztreonam, cefepime, ceftazidime, ciprofloxacin, colistin, imipenem, piperacillin-tazobactam). Infections were defined as hospital- and community-associated if cultured ≥ 48- and < 48-h post-admission, respectively.
Susceptibility trends between 2012 and 2016 were analyzed using only isolates from hospital sites that participated in all 5 years. A total of 21,299 isolates from 82 hospital sites were excluded. The Cochran-Armitage test was used to assess linear trends in percent susceptible if 10 or more isolates were available in each year. A two-tailed p value < 0.05 was considered statistically significant.
Data availability
The data generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Results
To assess changes in activity of ertapenem over the past 5 years, trend analyses were performed using only the 142 sites that participated every year of the study. A total of 85,001 Enterobacteriaceae isolates were included in the analysis. The distribution of species changed over this time period with a statistically significant decrease in the proportion of E. coli (from 58.4% in 2012 to 54.4% in 2016, p < 0.0001) and a corresponding increase in proportion of K. pneumoniae (from 18.0 to 19.9%, p < 0.0001), K. oxytoca (from 2.5 to 3.0%, p = 0.006), and Morganella morganii (from 1.6 to 2.0%, p = 0.009) (Fig. 1). To avoid confounding due to these changes in composition of Enterobacteriaceae, trend analyses were performed for the two most common species (E. coli and K. pneumoniae) individually, in addition to the analysis of all Enterobacteriaceae combined (Table 1). Small but statistically significant decreases in susceptibility to ertapenem were found for Enterobacteriaceae overall in all regions except the Middle East. Susceptibility remained ≥ 94% in 2016 in all regions except Asia (88.2% susceptible). Similarly, the susceptibility of E. coli showed a significantly decreasing trend in all regions except Africa, but remained ≥ 92% in all regions and ≥ 98% in five of the seven regions. Among K. pneumoniae, susceptibility to ertapenem decreased significantly in Africa (by 6 percentage points), Europe (by 8%), and US/Canada (by 2.5%). In 2016, susceptibility of K. pneumoniae was still > 90% in US/Canada and in the South Pacific region and was ≥ 80% in the other five regions.
For clinicians, knowledge of the current activity of ertapenem and comparator antibiotics is especially important. Therefore, we wanted to examine in more detail the most recent isolates, including analysis of the five most commonly collected species individually, as well as of subsets of isolates, such as those from hospital- and community-associated infections. To make these detailed analyses possible at a regional level, we maximized sample sizes by using isolates from all participating sites and by combining isolates from 2015 and 2016.
Figure 2 shows the regional species distribution among this collection of recent Enterobacteriaceae isolates. E. coli was the most common species in all regions, with the proportion ranging from 49.1% in US/Canada to 59.2% in Middle East, and K. pneumoniae was the second most common species in all regions, ranging from 16.7% in Europe to 23.6% in Asia. Table 2 shows the susceptibility to ertapenem and comparators of all Enterobacteriaceae combined and of the five most common species. Overall, susceptibility rates for ertapenem were > 90% in all regions except Asia, where it was only slightly lower (89.5%). Of the comparator agents, only amikacin exceeded these results. The cephalosporins and aztreonam showed values < 85% in most regions, ciprofloxacin values < 80% in most regions, and piperacillin-tazobactam values < 90% in all regions except US/Canada. Against E. coli, the carbapenems, amikacin, and colistin showed susceptibility rates > 95% in all regions (except ertapenem in Asia, 92.5%), whereas it was < 90% in each region for all other comparators except piperacillin-tazobactam (> 90% in four regions). Susceptibility of K. pneumoniae was < 90% in the majority of regions for all agents except amikacin and colistin. Ertapenem activity was high in US/Canada and South Pacific (≥ 95%) and ranged from 76.3% in Africa to 88.5% in the Middle East for the remaining regions. Susceptibility of P. mirabilis to ertapenem was ≥ 97% or higher in each region; of the comparators, only piperacillin-tazobactam and amikacin exceeded 90% susceptibility in each region. Activity of ertapenem was lower against E. cloacae (ranging from 75.5% susceptibility in Asia to 94.7% in the Middle East) with imipenem, amikacin, and colistin showing activity > 90% in most or all regions. Susceptibility of K. oxytoca was > 90% in all or most regions to the carbapenems, cefepime, ceftazidime, ciprofloxacin, amikacin, and colistin.
MIC50 values for ertapenem against Enterobacteriaceae were ≤ 0.06 μg/ml in all regions. MIC90 values were ≤ 0.06 μg/ml in US/Canada; 0.12 μg/ml in Europe, Middle East, and South Pacific; 0.25 μg/ml in Latin America; 0.5 μg/ml in Africa; and 1 μg/ml in Asia. Results for the comparator agents can be seen in Online Resource 2. Typically, MIC90 values for ertapenem were between 2 and 8 dilutions lower than for the comparators.
Using the collection of recent isolates, susceptibility rates were also assessed for subsets of isolates from community- and hospital-associated infections as well as ESBL-positive and MDR strains (Table 3). Ertapenem showed strong activity > 90% in all regions against Enterobacteriaceae from community-associated infections. Of the comparators, only amikacin exceeded these rates. Against Enterobacteriaceae from hospital-associated infection, susceptibility to ertapenem was > 90% in five regions, with activity ≥ 88% in the remaining two regions. Again, only amikacin exceeded these rates. Susceptibility was also analyzed among E. coli, K. oxytoca, K. pneumoniae, and P. mirabilis with ESBL phenotype. The rate of ESBL-positive isolates among these species varied widely by region: 9.9% (470/4752) in US/Canada, 12.7% (262/2062) in South Pacific, 17.5% (1783/10205) in Europe, 26.0% (1135/4372) in Asia (without China and India), 28.9% (657/2270) in Africa, 29.4% (1681/5710) in Latin America, and 38.2% (642/1681) in Middle East. Ertapenem was active against > 90% of ESBL-positive isolates in all regions except Africa (83.6%) and Europe (85.5%). Only imipenem, amikacin, and colistin exceeded these susceptibility levels.
The proportion of MDR Enterobacteriaceae among all collected isolates also varied widely by region: 12.4% (751/6074) in US/Canada, 14.6% (383/2627) in South Pacific, 18.4% (2284/12412) in Europe, 29.1% (757/2600) in Africa, 30.9% (2069/6686) in Latin America, 34.3% (653/1904) in Middle East, and 38.9% (3973/10202) in Asia. Susceptibility rates against MDR Enterobacteriaceae were generally ≤ 30% for the cephalosporins, aztreonam, and ciprofloxacin. Ertapenem and imipenem were active against ≥ 80% of isolates in most regions. Only amikacin reached susceptibility levels ca. 90% or higher in most regions, as well as colistin in Africa, Middle East, and South Pacific. Table 4 shows the ten most common MDR phenotypes found globally. Ertapenem was active against > 97% of isolates from four phenotypes, including one phenotype that was non-susceptible to imipenem (mostly Proteeae); showed activity against 54 to 83% of isolates from four phenotypes; and showed no or very poor activity against two phenotypes that were also non-susceptible to imipenem.
Discussion
According to a recent WHO report, antimicrobial resistance threatens the effective treatment of an ever-increasing range of infections [1]. A recent review of the global epidemiology of CTX-M β-lactamases describes increases in ESBL prevalence over time in all WHO geographical regions, especially in the community [9]. Carbapenems are considered the antimicrobial agents of choice for infections with ESBL-positive organisms; however, the prevalence of carbapenemases has also been increasing [10]. Furthermore, ESBL production combined with structural mutations can render organisms resistant to carbapenems. This makes antimicrobial surveillance, especially of carbapenems, crucial for the selection of appropriate agents for empiric therapy. The WHO report points out that significant gaps exist in antimicrobial surveillance with a lack of standards for methodology and with gaps in global coverage. Global surveillance programs like SMART can at least partially fill these gaps, as it monitors the antimicrobial activity of a consistent set of agents using standardized methodology in central laboratories. However, limitations remain, such as small numbers of participating sites per country as well as sites not participating every year. In an effort to address these limitations, country data were combined into larger regions in the current study, and for the trend analyses, only sites that participated in all 5 years were included.
These trend analyses revealed statistically significant decreases in susceptibility of Enterobacteriaceae to ertapenem in most regions. The actual size of the decreases, however, was small (between 0.9 and 2.5 percentage points), and susceptibility remained > 90% in all regions except Asia. The significant statistical test results are in part due to the large sample sizes for Enterobacteriaceae overall and for E. coli, as well as the fact that the proportion of susceptible isolates is close to 100%. These two factors give the statistical test increased power to find significant trends.
The analysis of only the more recent isolates (using all available participating sites) confirmed that ertapenem has maintained high antimicrobial activity in 2015–2016. Against Enterobacteriaceae overall, susceptibility rates were ca. 90% or higher in each region, ranging from 89.5% in Asia to 97.3% in US/Canada. Activity against E. coli, the most common species, was 92.5% in Asia and > 96% in all other regions. Activity was ≥ 93% in all regions against Enterobacteriaceae from community-associated infections, despite reports of increasing resistance in the community [10,11,12]. This is important as ertapenem is typically regarded as an important treatment option for patients with serious community-acquired infections [3, 4]. Even against Enterobacteriaceae from hospital-associated infections, ertapenem maintained susceptibility levels > 90% in most regions, rates consistently exceeded only by amikacin. This finding is especially noteworthy in light of reports identifying health care as a risk factors for acquisition of carbapenem-resistant strains [13], and studies reporting higher resistance levels in isolates from hospital- than from community-associated infections [14,15,16]. The latter were SMART studies that described antimicrobial resistance among E. coli and K. pneumoniae isolates from IAI collected in Europe in 2008 [14], E. coli from IAI collected in the USA 2009–2013 [15], and E. coli from UTI collected in Canada and the USA in 2010–2014 [16].
Ertapenem also showed strong activity against the subset of phenotypically ESBL-positive isolates, with susceptibility rates of > 90% in all regions, except Africa (83.6%) and Europe (85.5%). It should be noted that for this analysis, Asia did not include isolates from China and India, two countries for which high resistance rates, including high rates of carbapenemase-producing organisms, have been reported [17,18,19,20], and the susceptibility level of 93.6% to ertapenem is therefore presumably an overestimate. In fact, a separate analysis of the isolates from China and India for which ESBL determination was available showed ertapenem susceptibility rates among the ESBL-positive isolates of 88.0% in China (1317/1496) and 84.9% in India (141/166) (data not shown), which as expected were lower than for the rest of the region. However, because the ESBL phenotype was not available for 26 and 41% of isolates, respectively, these results must be interpreted with caution. Analysis of MDR isolates showed low MDR rates in US/Canada and South Pacific and high rates in Asia, Africa, Middle East, and Latin America. This regional pattern corresponds closely with the ESBL rates determined in this study, which is not surprising as ESBL production is typically associated with unrelated resistance determinants for fluoroquinolones, aminoglycosides, and tetracyclines [18]. Others have also described high MDR rates in these four regions [21] as well as high rates of ESBL and/or carbapenemase producers [17,18,19,20]. Regardless of region, ertapenem demonstrated good activity against MDR isolates with susceptibility rates of 73% in Africa, 75% in Asia, 78% in Europe, and > 80% in all other regions, levels that were generally > 50 percentage points higher than the susceptibility rates for cephalosporins, aztreonam, and ciprofloxacin and > 20 percentage points higher than for piperacillin-tazobactam. Only imipenem, amikacin, and colistin exceeded the activity of ertapenem. Compared to these agents, ertapenem has a once-daily administration schedule and is generally well-tolerated as opposed to the significant morbidities associated with aminoglycosides and polymyxins including nephro-, neuro-, and oto-toxicity.
Recent susceptibility rates for ertapenem are not readily available from sources other than SMART studies, of which the most recent ones focused exclusively on ESKAPE pathogens from Latin American and Asia/Pacific countries (without China and India) collected in 2013–2015 [22, 23]. One recently published non-SMART study showed high percent susceptible to ertapenem among Enterobacteriaceae (94.5%), E. coli (98.7%), and K. pneumoniae (87.4%), albeit for isolates from 2012 and 2013 [24]. Other recent publications demonstrated that ertapenem still remained very effective, including two clinical trials of bloodstream and urinary tract infections due to ESBL-producing Enterobacteriaceae [25, 26], for which ertapenem has been considered the treatment of choice [27]. Furthermore, ertapenem has been successfully and safely used as de-escalation therapy for patients who had received group 2 carbapenems for infections with ESBL-producing Enterobacteriaceae [28]. Outpatient therapy with ertapenem may therefore be a feasible option for clinically stable patients, reducing length of hospital stay and costs. Ertapenem also showed rapid bactericidal activity against MDR ESBL-producing E. coli isolates that were intermediately resistant to ertapenem (MIC of 1 μg/ml) when simulating free drug after 2-g intravenous once-daily dosing [27].
Fifteen years after the launch of ertapenem, despite the worrisome spread of antimicrobial resistance, this agent, which is popular among clinicians due to its convenient once-daily dosing schedule and favorable safety and tolerability profile, remains active in all regions of the world against 89.5 to 97.3% of consecutively collected Enterobacteriaceae from intra-abdominal and urinary tract infections. Nevertheless, continued monitoring of antimicrobial resistance for surveillance purposes as well as susceptibility testing for individual patients is important.
References
World Health Organization (2014) Antimicrobial resistance global report on Surveillance. http://www.who.int/drugresistance/documents/surveillancereport/en/
Giske CG, Monnet DL, Cars O, Carmeli Y, Resistance oboR-AoA (2008) Clinical and economic impact of common multidrug-resistant gram-negative bacilli. Antimicrob Agents Chemother 52(3):813–821. https://doi.org/10.1128/aac.01169-07
Zhanel GG, Johanson C, Embil JM, Noreddin A, Gin A, Vercaigne L, Hoban DJ (2005) Ertapenem: review of a new carbapenem. Expert Rev Anti-Infect Ther 3(1):23–39. https://doi.org/10.1586/14787210.3.1.23
Keating GM, Perry CM (2005) Ertapenem: a review of its use in the treatment of bacterial infections. 65
Morrissey I, Hackel M, Badal R, Bouchillon S, Hawser S, Biedenbach D (2013) A review of ten years of the study for monitoring antimicrobial resistance trends (SMART) from 2002 to 2011. Pharmaceuticals (Basel) 6(11):1335–1346. https://doi.org/10.3390/ph6111335
Clinical and Laboratory Standards Institute (2015) Methods for dilution antimicrobial susceptibility tests for Bacteria that grow aerobically ninth edition: approved standard M7-A10. Clinical and Laboratory Standards Institute, Wayne
Clinical and Laboratory Standards Institute (2017) Performance standards for antimicrobial susceptibility testing: twenty-seventh edition CLSI supplement M100-S27. Clinical and Laboratory Standards Institute, Wayne
European Committee on Antimicrobial Susceptibility Testing (2017) Breakpoint tables for interpretation of MICs and zone diameters, version 7.1. http://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Breakpoint_tables/v_7.1_Breakpoint_Tables.pdf. Accessed 15 Jan 2018
Bevan ER, Jones AM, Hawkey PM (2017) Global epidemiology of CTX-M β-lactamases: temporal and geographical shifts in genotype. J Antimicrob Chemother 72(8):2145–2155. https://doi.org/10.1093/jac/dkx146
Logan LK, Weinstein RA (2017) The epidemiology of Carbapenem-resistant Enterobacteriaceae: the impact and evolution of a global menace. J Infect Dis 215(suppl_1):S28–S36. https://doi.org/10.1093/infdis/jiw282
Pitout JD, Nordmann P, Laupland KB, Poirel L (2005) Emergence of Enterobacteriaceae producing extended-spectrum beta-lactamases (ESBLs) in the community. J Antimicrob Chemother 56(1):52–59. https://doi.org/10.1093/jac/dki166
Pitout JDD (2013) Enterobacteriaceae that produce extended-spectrum β -lactamases and AmpC β -lactamases in the community: the tip of the iceberg? Curr Pharm Des 19(2):257–263. https://doi.org/10.2174/1381612811306020257
Schwaber MJ, Klarfeld-Lidji S, Navon-Venezia S, Schwartz D, Leavitt A, Carmeli Y (2008) Predictors of Carbapenem-resistant Klebsiella pneumoniae acquisition among hospitalized adults and effect of acquisition on mortality. Antimicrob Agents Chemother 52(3):1028–1033. https://doi.org/10.1128/aac.01020-07
Hawser SP, Bouchillon SK, Hoban DJ, Badal RE, Canton R, Baquero F (2010) Incidence and antimicrobial susceptibility of Escherichia coli and Klebsiella pneumoniae with extended-spectrum beta-lactamases in community- and hospital-associated intra-abdominal infections in Europe: results of the 2008 study for monitoring antimicrobial resistance trends (SMART). Antimicrob Agents Chemother 54(7):3043–3046. https://doi.org/10.1128/AAC.00265-10
Lob SH, Kazmierczak KM, Badal RE, Hackel MA, Bouchillon SK, Biedenbach DJ, Sahm DF (2015) Trends in susceptibility of Escherichia coli from intra-abdominal infections to Ertapenem and comparators in the United States according to data from the SMART program, 2009 to 2013. Antimicrob Agents Chemother 59(6):3606–3610. https://doi.org/10.1128/aac.05186-14
Lob SH, Nicolle LE, Hoban DJ, Kazmierczak KM, Badal RE, Sahm DF (2016) Susceptibility patterns and ESBL rates of Escherichia coli from urinary tract infections in Canada and the United States, SMART 2010–2014. Diagn Microbiol Infect Dis 85(4):459–465. https://doi.org/10.1016/j.diagmicrobio.2016.04.022
Livermore DM (2012) Current epidemiology and growing resistance of gram-negative pathogens. Korean J Intern Med 27(2):128–142. https://doi.org/10.3904/kjim.2012.27.2.128
Theuretzbacher U (2013) Global antibacterial resistance: the never-ending story. J Glob Antimicrob Resist 1(2):63–69. https://doi.org/10.1016/j.jgar.2013.03.010
Nordmann P, Poirel L (2014) The difficult-to-control spread of carbapenemase producers among Enterobacteriaceae worldwide. Clin Microbiol Infect 20(9):821–830. https://doi.org/10.1111/1469-0691.12719
Mathers AJ, Peirano G, Pitout JD (2015) The role of epidemic resistance plasmids and international high-risk clones in the spread of multidrug-resistant Enterobacteriaceae. Clin Microbiol Rev 28(3):565–591. https://doi.org/10.1128/CMR.00116-14
Giammanco A, Calà C, Fasciana T, Dowzicky MJ (2017) Global assessment of the activity of tigecycline against multidrug-resistant gram-negative pathogens between 2004 and 2014 as part of the tigecycline evaluation and surveillance trial. mSphere 2(1):e00310–e00316
Karlowsky JA, Hoban DJ, Hackel MA, Lob SH, Sahm DF (2017) Resistance among gram-negative ESKAPE pathogens isolated from hospitalized patients with intra-abdominal and urinary tract infections in Latin American countries: SMART 2013–2015. Braz J Infect Dis 21(3):343–348. https://doi.org/10.1016/j.bjid.2017.03.006
Karlowsky JA, Hoban DJ, Hackel MA, Lob SH, Sahm DF (2017) Antimicrobial susceptibility of gram-negative ESKAPE pathogens isolated from hospitalized patients with intra-abdominal and urinary tract infections in Asia–Pacific countries: SMART 2013–2015. J Med Microbiol 66(1):61–69. https://doi.org/10.1099/jmm.0.000421
Karlowsky JA, Biedenbach DJ, Kazmierczak KM, Stone GG, Sahm DF (2016) Activity of ceftazidime-avibactam against extended-Spectrum- and AmpC beta-lactamase-producing Enterobacteriaceae collected in the INFORM global surveillance study from 2012 to 2014. Antimicrob Agents Chemother 60(5):2849–2857. https://doi.org/10.1128/aac.02286-15
Gutiérrez-Gutiérrez B, Bonomo RA, Carmeli Y, Paterson DL, Almirante B, Martínez-Martínez L, Oliver A, Calbo E, Peña C, Akova M, Pitout J, Origüen J, Pintado V, García-Vázquez E, Gasch O, Hamprecht A, Prim N, Tumbarello M, Bou G, Viale P, Tacconelli E, Almela M, Pérez F, Giamarellou H, Cisneros JM, Schwaber MJ, Venditti M, Lowman W, Bermejo J, Hsueh P-R, Mora-Rillo M, Gracia-Ahulfinger I, Pascual A, Rodríguez-Baño J, Gálvez J, de Cueto M, Salamanca E, Falcone M, Russo A, Daikos G, Karaiskos I, Trecarichi EM, Losito AR, Paterson DL, Hernández A, Gómez J, Roilides E, Iosifidis E, Doi Y, Tuon FF, Navarro F, Mirelis B, Juan RS, Fernández-Ruiz M, Larrosa N, Puig M, Molina J, González V, Rucci V, de Gopegui ER, Marinescu CI, Fariñas MC, Cano ME, Gozalo M, Paño-Pardo JR, Francisco CN-S, Gómez-Zorrilla S, Tubau F, Pournaras S, Tsakris A, Zarkotou O, Azap ÖK, Souli M, Antoniadou A, Poulakou G, Virmani D, Machuca I, Pérez-Nadales E, Torre-Cisneros J, Helvaci Ö, Sahin AO, Cantón R, Ruiz P, Bartoletti M, Giannella M, Riemenschneider F, Badia C, Xercavins M, Fontanals D, Jové E (2016) Ertapenem for the treatment of bloodstream infections due to ESBL-producing Enterobacteriaceae: a multinational pre-registered cohort study. J Antimicrob Chemother 71(6):1672–1680. https://doi.org/10.1093/jac/dkv502
Seo YB, Lee J, Kim YK, Lee SS, J-a L, Kim HY, Uh Y, Kim H-S, Song W (2017) Randomized controlled trial of piperacillin-tazobactam, cefepime and ertapenem for the treatment of urinary tract infection caused by extended-spectrum beta-lactamase-producing Escherichia coli. BMC Infect Dis 17:404. https://doi.org/10.1186/s12879-017-2502-x
Zhanel GG, Denisuik A, Vashisht S, Yachison C, Adam HJ, Hoban DJ (2014) Pharmacodynamic activity of ertapenem versus genotypically characterized extended-spectrum beta-lactamase (ESBL)-, KPC- or NDM-producing Escherichia coli with reduced susceptibility or resistance to ertapenem using an in vitro model. J Antimicrob Chemother 69(9):2448–2452. https://doi.org/10.1093/jac/dku149
Rattanaumpawan P, Werarak P, Jitmuang A, Kiratisin P, Thamlikitkul V (2017) Efficacy and safety of de-escalation therapy to ertapenem for treatment of infections caused by extended-spectrum-β-lactamase-producing Enterobacteriaceae: an open-label randomized controlled trial. BMC Infect Dis 17:183. https://doi.org/10.1186/s12879-017-2284-1
Acknowledgements
The authors thank all SMART participants for their contributions to the program.
Funding
Funding for this research was provided by Merck & Co., Inc., Kenilworth, NJ, which also included compensation fees for services in relation to preparing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Transparency declaration
SHL, MAH, DJH, and DFS work for International Health Management Associates, Inc. (IHMA), which receives funding from Merck & Co., Inc. for the SMART surveillance program. KY and MRM are employees of Merck & Co., Inc. The IHMA authors do not have personal financial interests in the sponsor of this paper (Merck & Co., Inc.).
Ethical approval
For this type of study, ethical approval is not required.
Electronic supplementary material
ESM 1
(PDF 236 kb)
Rights and permissions
About this article
Cite this article
Lob, S.H., Hackel, M.A., Hoban, D.J. et al. Activity of Ertapenem against Enterobacteriaceae in seven global regions—SMART 2012–2016. Eur J Clin Microbiol Infect Dis 37, 1481–1489 (2018). https://doi.org/10.1007/s10096-018-3274-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-018-3274-y