Abstract
Helicobacter pylori (H. pylori) resides in the stomach, colonizes gastric epithelium, and causes several digestive system diseases. Several diagnostic methods utilizing invasive or non-invasive techniques with varying levels of sensitivity and specificity are developed to detect H. pylori infection. Selection of one or more diagnostic tests will depend on the clinical conditions, the experience of the clinician, cost, sensitivity, and specificity. Invasive methods require endoscopy with biopsies of gastric tissues for the histology, culture, and rapid urease test. Among non-invasive tests, urea breath test and fecal antigen tests are a quick diagnostic procedure with comparable accuracy to biopsy-based techniques and are methods of choice in the test and treatment setting. Other techniques such as serological methods to detect immunoglobulin G antibodies to H. pylori can show high accuracy as other non-invasive and invasive biopsies, but do not differentiate between current or past H. pylori infections. Polymerase chain reaction (PCR) is an emerging option that can be categorized as invasive and non-invasive tests. PCR method is beneficial to detect H. pylori from gastric biopsies without the need for the cultures. There is no other chronic gastrointestinal infection such as H. pylori with a set of comparable diagnostic methodologies. Despite the availability of multiple diagnostic methods, it remains unclear on the choice of any one method as the gold standard for detecting H. pylori infection, especially in epidemiological studies. In this work, we review the principal diagnostic methods used to detect H. pylori infection and their advantages and disadvantages, and applications in clinical practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Helicobacter pylori (H. pylori) is a gram-negative bacterium that colonizes in gastric epithelium [1,2,3,4,5]. First, this bacterium was misrecognized as Pseudomonas spp. even though [6], during a clinical research project, Barry Marshall and Robin Warren discovered [7] it as Campylobacter pyloridis, which was later changed to H. pylori [8, 9].
H. pylori represent one of the most common bacterial infection in humans, which infected about half of the world’s population [10, 11]. Often, H. pylori infection occurs in childhood and continue throughout life when proper treatment is not provided [11]. In this regard, some studies suggested that the infected mothers are the major source of this infection of their kids, through contact with the contaminated stomach juice from the mother’s mouth [12].
Research indicates that H. pylori spread from East Africa about 58,000 years ago and subsequently developed into many strains with varying degrees of pathogenicity [13]. Generally, the prevalence of the bacterium infection varies according to age, region, race, and socioeconomic statuses. The prevalence of H. pylori infection in the developing countries is 50.8%, whereas the prevalence is 34.7% in the developed countries [14]. Many documents show that humans are the primary reservoir of H. pylori. The bacterium can also survive in dental plaques and saliva of a human [15]. The bacterial transmission can be through oral-oral, feco-oral, and gastro-oral routes [9, 16]. This bacterium has been found in water, as it is proven that the infection is transmitted through the water [17]. It is also reported that these bacteria can survive in the stomach of animals such as sheep and cats and milk of some others [18].
Effective treatment of the H. pylori infection is possible through antimicrobial therapy, prescribed to the susceptible patients. In order to treat the disease appropriately, suitable diagnostic procedures are necessary. Therefore, in this review, we aim to study the invasive and non-invasive diagnostic tests for H. pylori infection.
Pathogenicity of H. pylori
H. pylori is a gram-negative, helical bacillus, flagellated, slow-growing, microaerophilic, and fastidious bacterium [9, 19,20,21]. The bacterium isolated from the gastric mucosa is often seen as a spiral and curved in the culture medium [22].
H. pylori can survive in the gastric tissue, due to the presence of urease, its mobility, and ability to connect to the gastric epithelium [23, 24]. Some of the factors that provide an advantage for the successful bacterial colonization in the gastric epithelium include the shape of this bacterium, polar-sheathed flagella, mobility, chemotaxis, adherence, and persistence. Pathogenic factors such as cytotoxin-associated gene A (CagA), vacuolating cytotoxin A (VacA), outer inflammatory protein A (OipA), duodenal ulcer promoting gene a (dupA), sialic acid–binding adhesin (SabA), and blood group antigen–binding adhesin (BabA) are associated with increased virulence of H pylori [25,26,27,28]. This bacterium, with the help of the urease enzyme, breaks down urea to carbon dioxide and ammonia [29], through which it can neutralize the gastric acid, penetrate, and colonize in the gastric epithelium [30].
Immunopathogenesis of H. pylori–induced infection in gastric mucosa
The immune response towards pathogenic agents can be divided into innate and adaptive responses. H. pylori is an activator of both the innate and adaptive immune responses. The colonization of H. pylori in gastric mucosa triggers innate host defense mechanisms, including NOD1, TLR2, TLR4, TLR5, and TLR9, thus stimulating the expression of pro-inflammatory and antimicrobial peptides including defensins and cathelicidins by gastric epithelial cells as well as dendritic cells (DCs), neutrophils, and macrophages [31]. DCs and macrophages are activated and produce cytokines, including IL-6, IL-10, IL-12, IL-18, and IL-8 in inflamed mucosa of H. pylori–infected individuals [32].
The Th1/Th2 cell paradigm is an important concept to understand mucosal adaptive immunity and inflammation induced by H. pylori. Cytokine profiles indicate a Th1-predominant host immune response in the gastric mucosa, illustrated by IFN-γ production, which is associated with IL-12, IL-18, and TNF-α pro-inflammatory cytokines expression by DCs and macrophages [33]. Many studies support the involvement of Th17 cells in H. pylori infection by production of IL-17. IL-17 induces expression of IL-8, as a chemokine with the strong neutrophil chemoattractive property [34]. H. pylori can also elicit a strong specific systemic and mucosal IgG and IgA antibody responses. However, the humoral immune response is not protective in this infection. Many reports show that H. pylori induces regulatory T cell (Treg) responses to avoid both innate and adaptive immune defenses and maintain prolonged colonization of the gastric mucosa (Fig. 1).
Immunopathogenesis of H. pylori in gastric mucosa. H. pylori colonizes in gastric epithelium using urease. Binding and entering of H. pylori to epithelial cells results in the production of IL-8 and activation of the innate and adaptive immune systems as well as apoptosis of epithelial cells. Dendritic cells capture, process, and present bacterial antigens to the T cells in immunogenic or tolerogenic forms. Immunogenic DCs induce Th1/Th17 differentiation by producing IL-12, IL-6, and IL-23. IL-17 produced by Th17 cells targets innate immune cells and epithelial cells, to produce IL-8 (CXCL8), which results in neutrophil production and recruitment. Tolerogenic DCs provide a high level of IL-18 as well as TGF-훽/IL-10 for Treg differentiation. Macrophages are important activators of immune response to H. pylori, along with immunogenic DCs, by producing IL-12. IL-12 stimulates Th1 cells, resulting in production of IFN-γ, a key cytokine for activation of macrophages. H. pylori induces enhanced expression of indoleamine 2,3-dioxygenase (IDO) which results in diminished IFN-훾 production by Th1 cells and differentiation of Th2 cells. Colonization of H. pylori elicits the production of IgA and IgG antibodies, but it seems that antibodies are not essential for protection
Diseases and clinical manifestation
H. pylori is the cause of some gastric disorders (peptic ulcer disease (PUD), gastric adenocarcinoma, and gastric mucosa-associated lymphoid tissue (MALT) lymphoma [7, 35, 36]), which are the results of an interaction between bacterial virulence factors, host, and environmental factors. Several extra-gastric manifestations have been reported to be linked to H. pylori infection such as neurological, dermatological, hematologic, ocular, cardiovascular, metabolic, and allergic diseases [19]. Most of H. pylori infections usually are without clinical manifestation [37]. However, signs and symptoms associated with the disease are primarily due to gastric or peptic ulcer illness or duodenal inflammation. Furthermore, other symptoms such as abdominal pain, nausea, and vomiting may be attributed to other gastrointestinal diseases [38].
Peptic ulcer disease
Peptic ulcers are usually found in the stomach or proximal duodenum but can also be found in the esophagus or Meckel’s diverticulum. Peptic ulcer refers to the acid peptic injury of the digestive tract, resulting in mucosal break reaching the submucosa [39]. The lifetime prevalence of this disease in the general population has been estimated to be about 5–10% and incidence 0.1–0.3% per year. Over the past two centuries, PUD has been a major threat to the world’s population [39]. Some studies showed that PUD is at least fourfold higher in H. pylori–infected individuals than in non-infected individuals [40]. H. pylori along with non-steroidal anti-inflammatory drugs (NSAIDs) such as aspirin is the main cause of gastric and duodenal ulcers (imbalance of aggressive gastric luminescence and pepsin and protective mucosal barrier function) [41].
Gastric adenocarcinoma
Worldwide, gastric cancer (GC) is the fifth most commonly diagnosed malignancy and the fourth leading cause of cancer-related deaths per year [41, 42]. On the other hand H. pylori has been implicated as the strongest risk factor in the pathogenesis of gastric adenocarcinoma [40, 43]; thus, it has been classified as a class I carcinogen by the World Health Organization (WHO) [44]. GC is triggered by a multifactorial process, beginning with H. pylori–induced chronic gastritis, which results in atrophic gastritis, intestinal metaplasia, dysplasia, and eventually gastric cancer [45, 46].
Mucosa-associated lymphoid tissue lymphoma
The molecular pathogenesis of MALT lymphoma is incompletely understood, but it seems to include strain-specific H. pylori factors as well as host genetic factors, such as polymorphisms in inflammatory cytokine promoters such as TNF and IL-1β [47]. The mentioned lymphoma is an indolent extranodal marginal zone B cell lymphoma, originating in acquiring MALT that is induced in mucosal barriers as part of a normal adaptive immune response to a chronic immunoinflammatory stimulus, most notably chronic infections by H. pylori [48]. In addition to the disease caused by this bacterium, it should also be noted that the treatment of H. pylori infection has improved considerably since the early experiments in 1987. Currently, three or four drug regimens used for 7 to 14 days lead to the cure of the infection in 85 to 95% of the patients [49].
Evidence shows that the eradication of H. pylori or vaccination (vaccines were composed of different antigens and adjuvants applied by different routes and delivery systems) [50] may reduce the risk of ulcers and gastric cancer. Of course, in the case of vaccines, it should be reminded that some immunization strategies were tested in humans, but they almost never reached sterilizing immunity [51]. It should be noted that scientists argue that the co-evolution of H. pylori with the human population might have positive effects and protect children from diarrhea and asthma [52].
Diagnostic methods
Diagnostic methods have also been expanded with the evolution of H. pylori infection treatments. In spite of this, the standard methods applicable, especially in the population at risk, is still missing [11].
These methods should fulfill the common standards of clinical diagnostics like accuracy, sensitivity, and specificity. The methods should also be applicable in developing areas where hygiene standards and medical supports are poor [11].
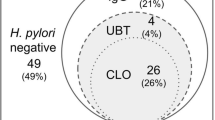
The diagnostic tests are separated into two divisions: invasive tests (endoscopy, histology, culture, and molecular methods) and non-invasive (urea breath test, fecal antigens, serological and molecular tests) for H. pylori infection (Table 1).
Non-invasive methods
These methods are based on the presence of bacterial enzymes, antigens, antibodies, or DNA sequences [53]. They include 13C or 14C urea breath test, stool antigen test (SAT), serology, and molecular methods [54].
Urea breath test
Urea breath test (UBT) is regarded as a gold standard non-invasive method for H. pylori diagnosis [55, 56]. This non-invasive test has high sensitivity, specificity, and accuracy [57, 58]. UBT has been used for about 30 years and is still the most popular, accurate, and common non-invasive test for the diagnosis of H. pylori infection [10].
This test can detect the infection indirectly by measuring the activity of bacterial urease produced by H. pylori in the stomach [11]. The test exploits the hydrolysis of orally administered urea by the H. pylori. An isotopically (13C or 14C) labeled urea is hydrolyzed into ammonia and carbon dioxide, which diffuses directly into the blood and excreted out through the lungs. The released carbon dioxide can be measured [10, 59, 60]. A 13C-labeled urea is preferred over 14C since 13C is stable and nonradioactive. An isotype ratio mass spectrometer is typically used to measure the release of 13C-enriched carbon dioxide from breath samples. However, this technique is expensive and requires a lot of skill. Recently, other less expensive methods like infrared spectroscopy and laser-assisted ratio analysis are developed as valid alternatives. The increase of 13C-labeled carbon dioxide in breath samples (taken before and about 30 min after drinking the test solution) indicates the bacterial urease activity. The intensity of the 13C signal in breath indicates the density of the microorganism colonization [54].
The 13C UBT has shown a variable level of accuracy in the pediatric population. Some meta-analyses confirmed that the 13C UBT is less accurate for the diagnosis of H. pylori infection in young children [60].
Several factors including the patient’s condition, bacterium, and the test itself can affect the results of the UBT [61]. Nonetheless, the urea breath test is widely available because breath samples are easy to collect for rapid testing [62]. UBT is useful for epidemiological studies and for assessing the effectiveness of eradication therapy [63]. This method has advantages such as non-invasive, safe, accurate, and with a sensitivity of 95.9% and a specificity of 95.7% [60, 64].
Factors can cause the false-negative test results; the patients have been received proton-pump inhibitors (PPIs) 2 weeks and antibiotic 4 weeks before this exam [65]. The bleeding also affects the diagnostic accuracy of UBT, and thus, UBT should be performed after recovery from bleeding [66]. Corpus-predominant gastritis can cause false-negative UBT results [67]. It should also be noted that although it is rarely true, the urease production of other pathogens in the stomach (such as H. heilmannii) which might lead to false-positive results [49].
It has been shown that UBT can detect an ongoing from past infections; hence, it can identify the eradication progress after treatment [68]. Also, according to various existing protocols, the accuracy of UBT test results depends on the amount of urea applied, sampling time, and the set point of the cutoff value [69].
Stool antigen test
In infected individuals, H. pylori sticks to the gastric epithelial wall and is excreted in the feces. This test is a direct test of initial infection that results in the superiority of serologic tests [70]. The test is based on the detection of H. pylori antigens in the stool. There are two types of SATs used for H. pylori detection: enzyme immunoassay (EIA)– and immunochromatography assay (ICA)–based methods, using either polyclonal antibodies or monoclonal antibodies [30, 49]. Monoclonal antibody–based tests show better results compared to polyclonal-based tests mainly because of the difficulty in obtaining polyclonal antibodies of consistent quality every time. EIA-based tests provide more accurate and reliable results than ICA-based tests although both tests can be performed with monoclonal antibodies [30, 71].
The systematic review and meta-analysis conducted by Leal et al. [72] established that stool enzyme-linked immunosorbent assay (ELISA) using monoclonal antibodies is an efficient non-invasive test for the diagnosis of H. pylori infection in children [62, 72, 73]. The sensitivity and specificity of this method are 94% and 97%, respectively [74]. Stool samples need to be refrigerated when stored before analysis; otherwise [75], the sensitivity of this test will be critically reduced [76].
The accuracy of this test can be influenced by some gastrointestinal problems, PPIs, antibiotics, and N-acetylcysteine (NAC) treatments, and bleeding ulcers [49].
Similar to the urea breath test, false-negative results occur when the bacterial load is relatively low and due to the use of the antibiotics, bismuth, and proton-pump inhibitors [77]. However, SAT may not require fasting and recently monoclonal antibodies unaffected by PPI are also developed. These advantages make SAT a better test compared to UBT. Many studies showed that SATs could distinguish actively infected from treated patients as well as to assess the effectiveness of H. pylori eradication [78]. However, to confirm the definitive eradication, it is advisable to wait until about 3 months after the end of the treatment [70]. SAT is a fast, simple, and inexpensive test [70, 79] and is also a useful tool for epidemiological studies and screening programs [80, 81].
The disadvantage of the SAT is the lack of enthusiasm for patients in the stool sample preparation. In addition, storage and handling of stool samples can also impact the assay results. For example, the stool should be frozen to keep the antigen intact when samples are not tested in a short period of time. The storage may become a problem in areas where freezing is not available. Selection of a cutoff point is an important factor for specificity and sensitivity of detection and may vary among the different population. Thus, a local validation of the test at a particular location is needed for better results [54].
Serology
In this method, antibodies against H. pylori are detected by ELISA, immunoblotting, and enzyme immunoassays (EIA) [30]. Although more tests for IgA, IgG, and IgM antibodies are performed, only the IgG antibody test is reliable. These tests involve the use of serum, saliva, or urine; however, the use of whole blood is still a controversial topic [82]. This method has a sensitivity and specificity of 76–84% and 79–90%, respectively [30].
Based on findings from many studies, such tests have a high negative predictive value (NPV). The ability of this test to detect active infections depends on the patient’s age, clinical conditions of infection, the choice of the antigen used for antibody preparation in ELISA kit, and the prevalence of infection [54, 83]. In patients treated with colloidal bismuth, antibiotics, and PPIs, if it is not possible to discontinue the mentioned medications, the IgG serologic tests may be beneficial since serological methods are less likely confounded by suppression of H. pylori by these treatments [83]. Therefore, in particular, in clinical scenarios such as gastrointestinal bleeding, gastric carcinoma, MALT lymphoma, and atrophic gastritis, the serological method is the efficient diagnostic method. Serological methods offer other advantages such as cost-effectiveness, wider availability, simplicity, and thus are commonly used in most studies of H. pylori epidemiological studies [84, 85]. Besides, a serological test for the evaluation of H. pylori infection in children is also found to be very helpful [85]. Another benefit of the serology test is that the accuracy of them is not affected by ulcer bleeding and gastric atrophy, which cause false-negative results in other invasive or non-invasive experiments [10]. However, if UBT and SAT are available, it will not be used for initial diagnosis because it only represents the previous exposure [54].
A urine-based ELISA is also found to be inexpensive, convenient serological method to detect anti-H. pylori antibodies in adults. Serological test from urine samples is much easier than serum samples because it does not require skills in sample collection and does not need preparation steps like centrifugation. However, the urine-based ELISA method is found to be unacceptable for children due to its low specificity (76.4%). The low specificity may be due to low concentrations of anti-H. pylori antibodies in the urine.
The major disadvantage of the serological approach is its inability to distinguish between the current infection and the previous exposure leading to misinterpretation. The IgG antibodies can be found even for the months after treatment and thus provide a positive result, even after the bacterial clearance [83, 84]. Therefore, it is usually not useful in confirming cure after antimicrobial therapy, but it is useful for epidemiological examinations [86]. False negatives can also result during early infection since the antibody levels are not sufficiently elevated during the early infection.
Invasive methods
These methods include endoscopy and gastric biopsy followed by either rapid urease test (RUT) or histology or culture, or molecular methods on biopsy samples. Each individual invasive test offers a specific clinical advantage. Rapid urease test (RUT) is the quickest test the provides an opportunity to start the treatment immediately. The histological examination provides a comprehensive assessment of gastric mucosa and thus help in short-term and long-term management strategies. Cultures have the highest specificity and are particularly useful in antibiotic susceptibility testing prior to choosing an appropriate eradication therapy. PCR is an emerging option to detect the bacterium without needing for cultures. The specific details and methodology of each technique are described below.
Endoscopy
A typical endoscopy exam is performed to detect H. pylori–related diseases. Endoscopy is the method for obtaining biopsies from the gastric mucosa that can be used in further studies on other invasive methods [87, 88]. Also, the endoscopy offers the precise and clear image of gastric mucosa, but it may not have better results than other diagnostic tests [89]. The major disadvantages of this procedure include the time-consuming process and require a lot of skill and experience [83].
Rapid urease test
Rapid urease test (RUT) is the popular invasive and cost-effective test for the detection of H. pylori infection [90]. If the biopsy is done, then the rapid urease test from gastric biopsies is the first choice [91]. This test is based on the production of urease enzyme by H. pylori bacteria and the presence of this enzyme in the gastric mucosa [92]. After the biopsy, the specimen is transferred to the solution comprising urea and a pH indicator [91, 93]. If H. pylori exists, urease will convert the urea into ammonia and CO2, which leads to change in color of the indicator due to an increase in pH [30]. In order to get the best results, biopsy specimens are taken from the gastric antrum and corpus [92].
The RUT is a very fast, inexpensive, reliable, and simple technique that provides the results in a few hours. An accurate detection would depend on the bacterial density in the biopsy samples [92, 94, 95]. It is worth noting that the sensitivity and specificity of this method are more than 90% [30, 91].
False-positive results of this test are possible in certain conditions [92, 96]. Several organisms such as Klebsiella pneumoniae, Staphylococcus aureus, Proteus mirabilis, Enterobacter cloacae, and Citrobacter freundii, isolated from the oral cavity and/ or stomach, also present urease activity and give false-positive results. Treatment with proton-pump inhibitors, antibiotics, and bismuth compounds [93] may cause false-negative results. As these agents can prevent the production of urease by H. pylori [92]. Also, we find similar findings in the cases with achlorhydria [95]. Besides, the sensitivity and specificity of the test are significantly lower in the cases of gastric ulcer bleeding and also in patients with intestinal metaplasia [54, 92, 96]. Therefore, in these cases where the RUT result is negative, a confirmation is needed by using appropriate alternate tests.
Histology
Histology is reviewed and considered as the gold standard in the direct diagnosis of H. pylori in mucus [83, 88]. This method is faster and, of course, more expensive than RUT and give essential data about the different types of gastritis (especially chronic form), atrophy, dysplasia, metaplasia, and malignant neoplasms [30]. The accuracy of the histopathological diagnosis of H. pylori is dependent on the number and location of the collected biopsy materials [97]. The diagnosis of H. pylori by this method can be made with only one biopsy sample taken from a suitable location, but multiple biopsies are recommended for high diagnostic accuracy and sensitivity [98, 99]. Due to the various distributions of these bacteria in the mucus layers, tissue samples should be taken from several areas of the stomach [100]. For this reason, the biopsy is better to be collected from both antrum and corpus [90, 101, 102]. Usually, two different stain methods are used for tissue samples from biopsy; hematoxylin and eosin (H&E) for assessment of inflammatory cells, and Giemsa for discernment of pathogen. Giemsa stain is commonly used in medical diagnostic laboratories [30, 54]. But when the results are unclear, other diagnostic techniques like toluidine blue, acridine orange, genta, the Romanowski, and the McMullen are beneficial [103, 104]. However, many of these methods are purely research-related. Some studies showed that histology had the higher sensitivity and specificity than the UBT and the RUT for the H. pylori diagnosis [105] so that the mentioned sensitivity and specificity were 80–95% and 99–100%, respectively [30].
Many factors affect the diagnostic accuracy of histological examination, like pathologist and gastroenterologist potentials and experiences, respectively, and in sampling and observation of biopsy specimens, staining techniques; the used medications are PPIs, antibiotics, and peptic ulcers bleeding [54, 83]. Also, the presence of other bacterial species, but with structural similarity to Helicobacter, can have adverse and dramatic effects on the results of this test [97, 98].
Based on the abovementioned, the several biggest weaknesses of this test are the observer dependency, the relative-to-the-long-time-to-get results, the need for specialized skills for relatively high performance, and the high cost [106].
Culture
The culture of H. pylori is performed on the gastric biopsy samples to confirm the H. pylori infection and is performed only in specialized laboratories [107]. Culturing of gastric biopsy samples to detect H. pylori is not a routine method for detecting H. pylori [108, 109]. Bacterial culture is carried out mainly for scientific research and when the prior treatments have failed to detect an appropriate bacterium. It is recommended that the mentioned test should be performed before the next treatment line to determine the microbial susceptibility [110, 111].
Although the culture is an expensive, complicated, and time-consuming test for H. pylori detection, an antibiotic susceptibility test of H. pylori by culture is a useful clinical practice for accurate detection. Besides, culture allows the isolation of H. pylori for phenotypic and genotypic studies [10, 84].
H. pylori needs selective media and microaerobic conditions (80–90% N2, 5–12% CO2, 5–10% O2) for growth [112, 113] and requires an incubation for 5–7 days at 37 °C [30, 114]. Several types of media can be used for H. pylori culture, including selective and non-selective agars (H. pylori agar, the Wang media, the Wilkins-Chalgren, brain-heart infusion (BHI), trypticase agar bases, Columbia and blood agar) [113, 114]. Antibiotics are used in the culture media to prevent the growth of other types of bacteria [11].
H. pylori should be cultured quickly after the biopsy [112]. A biopsy can be preserved in the transport medium (Portagerm pylori or Stuart) for up to 24 h at 4 °C and also isolates of H. pylori can be stored frozen at − 80 °C [113, 114]. GESA transport medium is a new medium that can store gastric biopsy specimens at 4 °C for up to10 days and provide a quantifiable recovery rate of H. pylori [115]. This method has a sensitivity and specificity of 70–80% and 100%, respectively [30, 116].
The culture’s results are affected by the skill and experience of the microbiologist, sample quality, exposure to the aerobic environment, and the use of the transport medium [113]. Also, other factors may affect the diagnostic accuracy of culture examination, like the decreased density of these pathogens in atrophic gastritis, alcohol drinking, bleeding, and the use of antibiotics, H2 receptor antagonists, and PPIs [117, 118].
Polymerase chain reaction
Over the past few decades, molecular detection has dramatically changed the clinical management of many infectious diseases [119]. Polymerase chain reaction (PCR) is one of the best molecular methods used in a wide range of clinical applications including broad-spectrum infection detection, evaluation of emerging infections, genotypic bacterial identification, antibiotic resistance, and in epidemiological studies [120, 121]. PCR-based detection of H. pylori could be classified as both invasive and non-invasive [119]. Samples are frequently used in this method including gastric juice and biopsy, saliva, and feces [120, 122, 123].
This method has high sensitivity and specificity (˃ 95%) [122, 124, 125]. PCR offers a simple, accurate, fast, automatic, and high efficiency of the H. pylori detection [120, 123]. In comparison to other common tests, PCR is more accurate to detect H. pylori in patients with bleeding [122, 125]. An accurate primer design and a proper gene selection are critical for a successful PCR reaction [11]. H. pylori genes such as vacA, cagA, UreA, GlmM, HSP60, 16SrRNA, 23SrRNA, and ureC can be used to amplify the H. pylori genome [30, 116]. Two or more target genes are amplified to increase the specificity of H. pylori diagnosis and to reduce the false-positive rates (particularly in specimens other than gastric biopsy samples) [122, 123, 125].
Bacterial resistance to antibiotics has become an increasingly difficult challenge for the health care community [126]. This problem is considered an essential challenge in medicine and microbiology. Alarmingly, the World Health Organization (WHO) recently issued the following statement: “the world is heading towards a post-antibiotic era in which common infections will once again start to kill” [127]. Molecular techniques like PCR is an appropriate methodology for pathogen detection can detect antibiotic resistance mutations and would help us in choosing an appropriate treatment strategy [128].
PCR can also be used to identify H. pylori in environmental samples for epidemiological researches. The relatively high prevalence of this pathogen in drinking water has been confirmed by PCR [129]. Moreover, the higher detection rate of H. pylori in unwashed vegetables suggests that the hygienic consumption of vegetables and complete washing of such foods is beneficial in reducing the infection with H. pylori [130]. The major disadvantages of PCR are that the technique is expensive and requires a lot of skill and experience. Also, false-positive results can be found in PCR due to its detection of DNA fragments from the killed bacteria [120, 121, 131].
Conclusion
H. pylori is a common bacterial infection of stomach epithelial tissue that causes severe anomalies, including chronic gastritis and gastric cancer. An accurate diagnosis of H. pylori infection is a critical first step in the successful treatment of this infection. Several methodologies are developed for H. pylori diagnosis and the choice of a particular depends on several factors such as clinical situations, availability of the appropriate technology to run the method at a clinical setting, and the accuracy, sensitivity, and specificity of the test. In this regard, our view is that we must continue our efforts to achieve more appropriate and reliable diagnostic tests.
References
Sgouras DN, Trang TTH, Yamaoka Y (2015) Pathogenesis of helicobacter pylori infection. Helicobacter 20:8–16
Ebrahimpour S, Esmaeili H, Ghadimi R (2017) Food bioactive componts, a possible adjuvant for H. pylori eradication. Caspian J Intern Med 8(2):131–132
Karkhah A, Ebrahimpour S, Rostamtabar M, Koppolu V, Darvish S, Krishna Rekha Vasigala V, Validi M, Nouri HR (2018) Helicobacter pylori evasion strategies of the host innate and adaptive immune responses to survive and develop gastrointestinal disease. Microbiol Res 218:49–57
Nourollahpour Shiadeh M, Riahi SM, Adam I, Saber V, Behboodi Moghadam Z, Armon B, Spotin A, Nazari Kangavari H, Rostami A (2017) Helicobacter pylori infection and risk of preeclampsia: a systematic review and meta-analysis. J Matern Fetal Neonatal Med 1–8
Shiadeh MN, Moghadam ZB, Adam I, Saber V, Bagheri M, Rostami A (2017) Human infectious diseases and risk of preeclampsia: an updated review of the literature. Infection 45(5):589–600
Fennerty M (1994) Helicobacter pylori. Arch Intern Med 154:721–727
O’connor A, Gisbert JP, O’morain C, Ladas S (2015) Treatment of helicobacter pylori infection 2015. Helicobacter 20:54–61
Perry S, De La Luz Sanchez M, Yang S, Haggerty TD, Hurst P, Perez-Perez G, Parsonnet J (2006) Gastroenteritis and transmission of Helicobacter pylori infection in households. Emerg Infect Dis 12(11):1701
Bui D, Brown H, Harris R, Oren E (2016) Serologic evidence for fecal-oral transmission of Helicobacter pylori. Am J Trop Med Hyg 94:82–88
Wang Y-K, Kuo F-C, Liu C-J, Wu M-C, Shih H-Y, Wang SS, Wu J-Y, Kuo C-H, Huang Y-K, Wu D-C (2015) Diagnosis of Helicobacter pylori infection: current options and developments. World J Gastroenterol: WJG 21(40):11221
Kalali B, Formichella L, Gerhard M (2015) Diagnosis of Helicobacter pylori: changes towards the future. Diseases 3(3):122–135
Veres G, Pehlivanoglu E (2007) Helicobacter pylori infection in pediatrics. Helicobacter 12:38–44
Linz B, Balloux F, Moodley Y, Manica A, Liu H, Roumangnac P, Falush D, Stamer C, Prugnolle F, Svd M, Yamaoka Y, Gragam D, Perez-Trallero E, Wadstorm T, Suerbaum S, Achtman M (2007) An African origin for the intimate association between humans and Helicobacter pylori. Nature 915–918:915–918
Zamani M, Ebrahimtabar F, Zamani V, Miller W, Alizadeh-Navaei R, Shokri-Shirvani J, Derakhshan M (2018) Systematic review with meta-analysis: the worldwide prevalence of Helicobacter pylori infection. Aliment Pharmacol Ther 47(7):868–876
Ogunbodede E, Lawal O, Lamikanra A, Okeke I, Rotimi O, Rasheed A (2002) Helicobacter pylori in the dental plaque and gastric mucosa of dyspeptic Nigerian patients. Trop Gastroenterol 23(3):127–133
Megraud F (1995) Transmission of Helicobacter pylori: faecal-oral versus oral-oral route. Aliment Pharmacol Ther 9:85–91
Brown LM (2000) Helicobacter pylori: epidemiology and routes of transmission. Epidemiol Rev 22(2):283–297
Quaglia N, Dambrosio A, Normanno G, Parisi A, Patrono R, Ranieri G, Rella A, Celano G (2008) High occurrence of Helicobacter pylori in raw goat, sheep and cow milk inferred by glmM gene: a risk of food-borne infection? Int J Food Microbiol 124(1):43–47
Gravina AG, Zagari RM, De Musis C, Romano L, Loguercio C, Romano M (2018) Helicobacter pylori and extragastric diseases: a review. World J Gastroenterol 24(29):3204–3221
Ahmed MA, Hassan NG, Omer ME, Rostami A, Rayis DA, Adam I (2018) Helicobacter pylori and Chlamydia trachomatis in Sudanese women with preeclampsia. J Matern Fetal Neonatal Med (just-accepted) 1–11
Xu Z, Li J, Wang H, Xu G (2017) Helicobacter pylori infection and atherosclerosis: is there a causal relationship? Eur J Clin Microbiol Infect Dis 36(12):2293–2301
Archer JR, Romero S, Ritchie A, Hamacher M, Steiner B, Bryner J, Schell R (1988) Characterization of an unclassified microaerophilic bacterium associated with gastroenteritis. J Clin Microbiol 26(1):101–105
Mobley HL (1996) Defining Helicobacter pylori as a pathogen: strain heterogeneity and virulence. Am J Med 100:2S–11S
Logan R (1996) Adherence of Helicobacter pylori. Aliment Pharmacol Ther 10(Sup1):3–15
Huang JQ, Zheng GF, Sumanac K, Irvine EJ, Hunt RH (2003) Meta-analysis of the relationship between cagA seropositivity and gastric cancer. Gastroenterology 125(6):1636–1644
Nejati S, Karkhah A, Darvish H, Validi M, Ebarhimpour S, Nouri HR (2018) Influence of Helicobacter pylori virulence factors CagA and VacA on pathogenesis of gastrointestinal disorders. Microb Pathog 117:43–48
Yamaoka Y (2010) Mechanisms of disease: Helicobacter pylori virulence factors. Nat Rev Gastroenterol Hepatol 7(11):629
Mishra S (2013) Is Helicobacter pylori good or bad? Eur J Clin Microbiol Infect Dis 32(3):301–304
Dasani BM, Sigal SH, Lieber CS (1998) Analysis of risk factors for chronic hepatic encephalopathy: the role of Helicobacter pylori infection. Am J Gastroenterol 93(5):726
Thaker Y, Moon A, Afzali A (2016) Helicobacter pylori: a review of epidemiology, treatment, and management. J Clin Gastroenterol Treat 2(19):1–5
Tran LS, Tran D, De Paoli A, D’Costa K, Creed SJ, Ng GZ, Le L, Sutton P, Silke J, Nachbur U, Ferrero RL (2018) NOD1 is required for Helicobacter pylori induction of IL-33 responses in gastric epithelial cells. Cell Microbiol 20(5):e12826
Bimczok D, Clements RH, Waites KB, Novak L, Eckhoff DE, Mannon PJ, Smith PD, Smythies LE (2010) Human primary gastric dendritic cells induce a Th1 response to H. pylori. Mucosal Immunol 3(3):260–269
Abdollahi H, Shams S, Zahedi MJ, Darvish Moghadam S, Hayatbakhsh MM, Jafarzadeh A (2011) IL-10, TNF-alpha and IFN-gamma levels in serum and stomach mucosa of Helicobacter pylori-infected patients. Iran J Allergy Asthma Immunol 10(4):267–271
Shamsdin SA, Alborzi A, Rasouli M, Hosseini MK, Bagheri Lankrani K, Kalani M (2015) Alterations in Th17 and the respective cytokine levels in Helicobacter pylori-induced stomach diseases. Helicobacter 20(6):460–475
Marshall B, Adams PC (2008) Helicobacter pylori: a nobel pursuit? Can J Gastroenterol 22(11):895–896
Masrour-Roudsari J, Ebrahimpour S (2017) Causal role of infectious agents in cancer: an overview. Caspian J Intern Med 8(3):153
Figueiredo C, Machado JC, Pharoah P, Seruca R, Sousa S, Carvalho R, Capelinha AF, Quint W, Caldas C, van Doorn L-J (2002) Helicobacter pylori and interleukin 1 genotyping: an opportunity to identify high-risk individuals for gastric carcinoma. J Natl Cancer Inst 94(22):1680–1687
Gold BD, Gilger MA, Czinn SJ (2014) New diagnostic strategies for detection of helicobacter pylori infection in pediatric patients. Gastroenterol Hepatol 10(12 Suppl 7):1
Malfertheiner P, Chan FK, McColl KE (2009) Peptic ulcer disease. Lancet 374(9699):1449–1461
Tham TC, Chen L, Dennison N, Johnston CF, Collins JS, Ardill J, Buchanan KD (1998) Effect of Helicobacter pylori eradication on antral somatostatin cell density in humans. Eur J Gastroenterol Hepatol 10(4):289–291
Zhang B-B, Li Y, Liu X-Q, Wang P-J, Yang B, Bian D-L (2014) Association between vacA genotypes and the risk of duodenal ulcer: a meta-analysis. Mol Biol Rep 41(11):7241–7254
Lordick F, Allum W, Carneiro F, Mitry E, Tabernero J, Tan P, Van Cutsem E, van de Velde C, Cervantes A (2014) Unmet needs and challenges in gastric cancer: the way forward. Cancer Treat Rev 40(6):692–700
Suerbaum S, Michetti P (2002) Helicobacter pylori infection. N Engl J Med 347(15):1175–1186
Houghton J, Wang TC (2005) Helicobacter pylori and gastric cancer: a new paradigm for inflammation-associated epithelial cancers. Gastroenterology 128(6):1567–1578
Valenzuela MA, Canales J, Corvalán AH, Quest AF (2015) Helicobacter pylori-induced inflammation and epigenetic changes during gastric carcinogenesis. World J Gastroenterol 21(45):12742
Weren RD, van der Post RS, Vogelaar IP, van Krieken JH, Spruijt L, Lubinski J, Jakubowska A, Teodorczyk U, Aalfs CM, van Hest LP (2018) Role of germline aberrations affecting CTNNA1, MAP3K6 and MYD88 in gastric cancer susceptibility. J Med Genet 55(10):669–674
Hussell T, Isaacson PG, Crabtree JE, Spencer J (1996) Helicobacter pylori-specific tumour-infiltrating T cells provide contact dependent help for the growth of malignant B cells in low-grade gastric lymphoma of mucosa-associated lymphoid tissue. J Pathol 178(2):122–127
Pereira M-I, Medeiros JA (2014) Role of Helicobacter pylori in gastric mucosa-associated lymphoid tissue lymphomas. World J Gastroenterol: WJG 20(3):684
Garza-González E, Perez-Perez GI, Maldonado-Garza HJ, Bosques-Padilla FJ (2014) A review of Helicobacter pylori diagnosis, treatment, and methods to detect eradication. World J Gastroenterol 20(6):1438
Sutton P, Chionh YT (2013) Why can’t we make an effective vaccine against Helicobacter pylori? Expert Review of Vaccines 12(4):433–441
Arnold IC, Lee JY, Amieva MR, Roers A, Flavell RA, Sparwasser T, Müller A (2011) Tolerance rather than immunity protects from Helicobacter pylori–induced gastric preneoplasia. Gastroenterology 140(1):199–209 e198
Chen Y, Blaser MJ (2007) Inverse associations of Helicobacter pylori with asthma and allergy. Arch Intern Med 167(8):821–827
Vaira D, Gatta L, Ricci C, Miglioli M (2002) Diagnosis of Helicobacter pylori infection. Aliment Pharmacol Ther 16:16–23
Braden B (2012) Diagnosis of Helicobacter pylori infection. BMJ 344:e828
Kosunen TU, Seppäla K, Sarna S, Sipponen P (1992) Diagnostic value of decreasing IgG, IgA, and IgM antibody titres after eradication of Helicobacter pylori. Lancet 339(8798):893–895
Goossens H, Glupczynski Y, Burette A, Van den Borre C, DePrez C, Bodenmann J, Keller A, Butzler J (1992) Evaluation of a commercially available complement fixation test for diagnosis of Helicobacter pylori infection and for follow-up after antimicrobial therapy. J Clin Microbiol 30(12):3230–3233
Braden B, Duan L, Caspary W, Lembcke B (1994) More convenient 13C-urea breath test modifications still meet the criteria for valid diagnosis of Helicobacter pylori infection. Z Gastroenterol 32(4):198–202
Epple H, Kirstein F, Bojarski C, Frege J, Fromm M, Riecken E, Schulzke J (1997) 13C-Urea breath test in helicobacter pylori diagnosis and eradication correlation to histology, origin of ‘false’ results, and influence of food intake. Scand J Gastroenterol 32(4):308–314
Best LM, Takwoingi Y, Siddique S, Selladurai A, Gandhi A, Low B, Yaghoobi M, Gurusamy KS (2018) Non†invasive diagnostic tests for Helicobacter pylori infection. Cochrane Database Syst Rev (3)
Leal YA, Flores LL, Fuentesâ Pananã EM, Cedilloâ Rivera R, Torres J (2011) 13C urea breath test for the diagnosis of Helicobacter pylori infection in children: a systematic review and meta analysis. Helicobacter 16(4):327–337
Ferwana M, Abdulmajeed I, Alhajiahmed A, Madani W, Firwana B, Hasan R, Altayar O, Limburg PJ, Murad MH, Knawy B (2015) Accuracy of urea breath test in Helicobacter pylori infection: meta-analysis. World J Gastroenterol 21(4):1305
Tonkic A, Tonkic M, Lehours P, Mégraud F (2012) Epidemiology and diagnosis of Helicobacter pylori infection. Helicobacter 17:1–8
Gong Y, Wei W, Yuan Y (2014) Association between abnormal gastric function risk and Helicobacter pylori infection assessed by ELISA and 14C-urea breath test. Diagn Microbiol Infect Dis 80(4):316–320
Guarner J, Kalach N, Elitsur Y, Koletzko S (2010) Helicobacter pylori diagnostic tests in children: review of the literature from 1999 to 2009. Eur J Pediatr 169(1):15–25
McColl KE (2010) Helicobacter pylori infection. N Engl J Med 362(17):1597–1604
Ontsira Ngoyi EN, Atipo Ibara BI, Moyen R, Ahoui Apendi PC, Ibara JR, Obengui O, Ossibi Ibara RB, Nguimbi E, Niama RF, Ouamba JM (2015) Molecular detection of Helicobacter pylori and its antimicrobial resistance in Brazzaville. Congo Helicobacter 20(4):316–320
Capurso G, Carnuccio A, Lahner E, Panzuto F, Baccini F, Fave G, Annibale B (2006) Corpus-predominant gastritis as a risk factor for false-negative 13C-urea breath test results. Aliment Pharmacol Ther 24(10):1453–1460
Gatta L, Vakil N, Ricci C, Osborn J, Tampieri A, Perna F, Miglioli M, Vaira D (2003) A rapid, low-dose, 13C-urea tablet for the detection of Helicobacter pylori infection before and after treatment. Aliment Pharmacol Ther 17(6):793–798
Gisbert J, Pajares J (2004) 13C-urea breath test in the diagnosis of Helicobacter pylori infection–a critical review. Aliment Pharmacol Ther 20(10):1001–1017
Koletzko S, Konstantopoulos N, Bosman D, Feydt-Schmidt A, Van der Ende A, Kalach N, Raymond J, Rüssmann H (2003) Evaluation of a novel monoclonal enzyme immunoassay for detection of Helicobacter pylori antigen in stool from children. Gut 52(6):804–806
Korkmaz H, Kesli R, Karabagli P, Terzi Y (2013) Comparison of the diagnostic accuracy of five different stool antigen tests for the diagnosis of Helicobacter pylori infection. Helicobacter 18(5):384–391
Leal YA, Cedillo-Rivera R, Simón JA, Velázquez JR, Flores LL, Torres J (2011) Utility of stool sample–based tests for the diagnosis of Helicobacter pylori infection in children. J Pediatr Gastroenterol Nutr 52(6):718–728
Zhou X, Su J, Xu G, Zhang G (2014) Accuracy of stool antigen test for the diagnosis of helicobacter pylori infection in children: a meta-analysis. Clin Res Hepatol Gastroenterol 38(5):629–638
Gisbert JP, De La Morena F, Abraira V (2006) Accuracy of monoclonal stool antigen test for the diagnosis of H. pylori infection: a systematic review and meta-analysis. Am J Gastroenterol 101(8):1921
Malfertheiner P, Megraud F, O’Morain C, Bazzoli F, El-Omar E, Graham D, Hunt R, Rokkas T, Vakil N, Kuipers EJ (2006) Current concepts in the management of Helicobacter pylori infection-the Maastricht III consensus report. Gut 56(6):772–781
Malfertheiner P, Megraud F, O’morain C, Bell D, Porro BG, Deltenre M, Forman D, Gasbarrini G, Jaup B, Misiewicz J (1997) Current European concepts in the management of Helicobacter pyloriinfection-the Maastricht Consensus Report. Eur J Gastroenterol Hepatol 9(1):1–2
Manes G, Balzano A, Iaquinto G, Ricci C, Piccirillo M, Giardullo N, Todisco A, Lioniello M, Vaira D (2001) Accuracy of the stool antigen test in the diagnosis of Helicobacter pylori infection before treatment and in patients on omeprazole therapy. Aliment Pharmacol Ther 15(1):73–79
Gisbert J, Cabrera MMM, Pajares J (2002) Stool antigen test for initial Helicobacter pylori diagnosis and for confirmation of eradication after therapy. Med Clin 118(11):401–404
Prell C, Osterrieder S, Lottspeich C, Schwarzer A, Rüssmann H, Ossiander G, Koletzko S (2009) Improved performance of a rapid office-based stool test for detection of Helicobacter pylori in children before and after therapy. J Clin Microbiol 47(12):3980–3984
Lee Y-C, Tseng P-H, Liou J-M, Chen M-J, Chen C-C, Tu C-H, Chiang T-H, Chiu H-M, Lai C-F, Ho J-C (2014) Performance of a one-step fecal sample-based test for diagnosis of Helicobacter pylori infection in primary care and mass screening settings. J Formos Med Assoc 113(12):899–907
Okuda M, Osaki T, Lin Y, Yonezawa H, Maekawa K, Kamiya S, Fukuda Y, Kikuchi S (2015) Low prevalence and incidence of Helicobacter pylori infection in children: a population-based study in J apan. Helicobacter 20(2):133–138
Vaira D, Holton J, Menegatti M, Ricci C, Landi F, Gatta L, Acciardi C, Farinelli S, Crosatti M, Berardi S (1999) New immunological assays for the diagnosis of Helicobacter pyloriinfection. Gut 45(suppl 1):I23–I27
Malfertheiner P, Megraud F, O’morain CA, Atherton J, Axon AT, Bazzoli F, Gensini GF, Gisbert JP, Graham DY, Rokkas T (2012) Management of Helicobacter pylori infection—the Maastricht IV/Florence consensus report. Gut 61(5):646–664
Jemilohun AC, Otegbayo JA (2016) Helicobacter pylori infection: past, present and future. Pan Afr Med J 23(1)
Ueda J, Okuda M, Nishiyama T, Lin Y, Fukuda Y, Kikuchi S (2014) Diagnostic accuracy of the E-plate serum antibody test kit in detecting Helicobacter pylori infection among Japanese children. J Epidemiol 24(1):47–51
Monteiro L, De Mascarel A, Sarrasqueta AM, Bergey B, Barberis C, Talby P, Roux D, Shouler L, Goldfain D, Lamouliatte H (2001) Diagnosis of Helicobacter pylori infection: noninvasive methods compared to invasive methods and evaluation of two new tests. Am J Gastroenterol 96(2):353
Lee JH, Park YS, Choi KS, Kim DH, Choi KD, Song HJ, Lee GH, Jang SJ, Jung HY, Kim JH (2012) Optimal biopsy site for Helicobacter pylori detection during endoscopic mucosectomy in patients with extensive gastric atrophy. Helicobacter 17(6):405–410
Lan H-C, Chen T-S, Li AF-Y, Chang F-Y, Lin H-C (2012) Additional corpus biopsy enhances the detection of Helicobacter pylori infection in a background of gastritis with atrophy. BMC Gastroenterol 12(1):182
Cho JH, Chang YW, Jang JY, Shim JJ, Lee CK, Dong SH, Kim HJ, Kim BH, Lee TH, Cho JY (2013) Close observation of gastric mucosal pattern by standard endoscopy can predict Helicobacter pylori infection status. J Gastroenterol Hepatol 28(2):279–284
Lash J, Genta R (2013) Adherence to the Sydney system guidelines increases the detection of Helicobacter gastritis and intestinal metaplasia in 400 738 sets of gastric biopsies. Aliment Pharmacol Ther 38(4):424–431
Vaira D, Vakil N, Gatta L, Ricci C, Perna F, Saracino I, Fiorini G, Holton J (2010) Accuracy of a new ultrafast rapid urease test to diagnose Helicobacter pylori infection in 1000 consecutive dyspeptic patients. Aliment Pharmacol Ther 31(2):331–338
Uotani T, Graham DY (2015) Diagnosis of Helicobacter pylori using the rapid urease test. Ann Transl Med 3(1)
Lewis JD, Kroser J, Bevan J, Furth EE, Metz DC (1997) Urease-based tests for Helicobacter pylori gastritis: accurate for diagnosis but poor correlation with disease severity. J Clin Gastroenterol 25(2):415–420
Choi YJ, Kim N, Lim J, Jo SY, Shin CM, Lee HS, Lee SH, Park YS, Hwang JH, Kim JW (2012) Accuracy of diagnostic tests for Helicobacter pylori in patients with peptic ulcer bleeding. Helicobacter 17(2):77–85
Moon SW, Kim TH, Kim HS, Ju J-H, Ahn YJ, Jang HJ, Shim SG, Kim HJ, Jung WT, Lee O-J (2012) United rapid urease test is superior than separate test in detecting Helicobacter pylori at the gastric antrum and body specimens. Clin endoscop 45(4):392
Lee J, Breslin N, Fallon C, O’morain C (2000) Rapid urease tests lack sensitivity in Helicobacter pylori diagnosis when peptic ulcer disease presents with bleeding. Am J Gastroenterol 95(5):1166
Patel SK, Pratap CB, Verma AK, Jain AK, Dixit VK, Nath G (2013) Pseudomonas fluorescens-like bacteria from the stomach: a microbiological and molecular study. World J Gastroenterol 19(7):1056
Patel SK, Pratap CB, Jain AK, Gulati AK, Nath G (2014) Diagnosis of Helicobacter pylori: what should be the gold standard? World J Gastroenterol 20(36):12847
El-Zimaity HM, Graham DY (1999) Evaluation of gastric mucosal biopsy site and number for identification of Helicobacter pylori or intestinal metaplasia: role of the Sydney System. Hum Pathol 30(1):72–77
Morgner A, Lehn N, Andersen LP, Thiede C, Bennedsen M, Trebesius K, Neubauer B, Neubauer A, Stolte M, Bayerdörffer E (2000) Helicobacter heilmannii–associated primary gastric low-grade MALT lymphoma: complete remission after curing the infection. Gastroenterology 118(5):821–828
Ola S, Yakubu A, Otegbayo J, Oluwasola A, Ogunbiyi J, Akang E, Summerton C (2006) The most appropriate site for endoscopic biopsy for the detection of H. pylori among Nigerians in Ibadan. West Afr J Med 25(4):269–272
Chey WD, Wong BC (2007) American College of Gastroenterology guideline on the management of Helicobacter pylori infection. Am J Gastroenterol 102(8):1808
Hartman DJ, Owens SR (2012) Are routine ancillary stains required to diagnose Helicobacter infection in gastric biopsy specimens? An institutional quality assurance review. Am J Clin Pathol 137(2):255–260
Batts KP, Ketover S, Kakar S, Krasinskas AM, Mitchell KA, Wilcox R, Westerhoff M, Rank J, Gibson J, Mattia AR (2013) Appropriate use of special stains for identifying Helicobacter pylori: recommendations from the Rodger C. Haggitt Gastrointestinal Pathology Society. Am J Surg Pathol 37(11):e12–e22
Tian X-Y, Zhu H, Zhao J, She Q, Zhang G-X (2012) Diagnostic performance of urea breath test, rapid urea test, and histology for Helicobacter pylori infection in patients with partial gastrectomy: a meta-analysis. J Clin Gastroenterol 46(4):285–292
Graham DY, Malaty HM, Evans DG, Evans DJ Jr, Klein PD, Adam E (1991) Epidemiology of Helicobacter pylori in an asymptomatic population in the United States: effect of age, race, and socioeconomic status. Gastroenterology 100(6):1495–1501
Grove DI, Koutsouridis G, Cummins AG (1998) Comparison of culture, histopathology and urease testing for the diagnosis of Helicobacter pylori gastritis and susceptibility to amoxycillin, clarithromycin, metronidazole and tetracycline. Pathology 30(2):183–187
Samuels AL, Windsor HM, Ho GY, Goodwin LD, Marshall BJ (2000) Culture of Helicobacter pylori from a gastric string may be an alternative to endoscopic biopsy. J Clin Microbiol 38(6):2438–2439
Jaup BH, Stenquist B, Brandberg ÃK (2000) Helicobacter pylori culture from a positive, liquid-based urease test for routine clinical use: a cost-effective approach. Helicobacter 5(1):22–23
Ogata SK, Godoy APO, da Silva Patricio FR, Kawakami E (2013) High Helicobacter pylori resistance to metronidazole and clarithromycin in Brazilian children and adolescents. J Pediatr Gastroenterol Nutr 56(6):645–648
Taj Y, Essa F, Kazmi S, Abdullah E (2003) Sensitivity and specificity of various diagnostic tests in the detection of helicobacter pylori. J Coll Physicians Surg Pak 13(2):90–93
Perez-Perez GI (2000) Accurate diagnosis of Helicobacter pylori: culture including transport. Gastroenterol Clin N Am 29(4):879–884
Ndip RN, MacKay WG, Farthing MJ, Weaver LT (2003) Culturing Helicobacter pylori from clinical specimens: review of microbiologic methods. J Pediatr Gastroenterol Nutr 36(5):616–622
Park SA, Ko A, Lee NG (2011) Stimulation of growth of the human gastric pathogen Helicobacter pylori by atmospheric level of oxygen under high carbon dioxide tension. BMC Microbiol 11(1):96
Cellini L, Di Campli E, Di Bartolomeo S, Bessa LJ, Baffoni M, Di Giulio M (2014) New transport medium for cultural recovery of Helicobacter pylori. J Clin Microbiol 52(12):4325–4329
Roth DE, VelapatiÃo B, Gilman RH, Su WW, Berg DE, Cabrera L, Garcia E, Group GPW (2001) A comparison of a string test-PCR assay and a stool antigen immunoassay (HpSA) for Helicobacter pylori screening in Peru. Trans R Soc Trop Med Hyg 95(4):398–399
Mégraud F, Lehours P (2007) Helicobacter pylori detection and antimicrobial susceptibility testing. Clin Microbiol Rev 20(2):280–322
Hutton ML, Kaparakis-Liaskos M, Ferrero RL (2012) The use of AlbuMAX II® as a blood or serum alternative for the culture of Helicobacter pylori. Helicobacter 17(1):68–76
Yang S, Rothman RE (2004) PCR-based diagnostics for infectious diseases: uses, limitations, and future applications in acute-care settings. Lancet Infect Dis 4(6):337–348
Rimbara E, Sasatsu M, Graham DY (2013) PCR detection of Helicobacter pylori in clinical samples PCR Detection of Microbial Pathogens. Methods Mol Biol 943:279–287
Duś I, Dobosz T, Manzin A, Loi G, Serra C, Radwan-Oczko M (2013) Role of PCR in Helicobacter pylori diagnostics and research--new approaches for study of coccoid and spiral forms of the bacteria. Postepy Hig Med Dosw (Online) 67(9):261–218
Saez J, Belda S, Santibáñez M, Rodríguez JC, Sola-Vera J, Galiana A, Ruiz-García M, Brotons A, López-Girona E, Girona E (2012) Real-time pcr for diagnosing Helicobacter pylori infection in patients with upper gastrointestinal bleeding. Comparison with other classical diagnostic methods. J Clin Microbiol 01205–01212
Lehours P, Mégraud F (2011) Helicobacter pylori molecular diagnosis. Expert Rev Mol Diagn 11(4):351–355
Gill P, Alvandi A-H, Abdul-Tehrani H, Sadeghizadeh M (2008) Colorimetric detection of Helicobacter pylori DNA using isothermal helicase-dependent amplification and gold nanoparticle probes. Diagn Microbiol Infect Dis 62(2):119–124
Momtaz H, Souod N, Dabiri H, Sarshar M (2012) Study of Helicobacter pylori genotype status in saliva, dental plaques, stool and gastric biopsy samples. World J Gastroenterol 18(17):2105
Schweizer HP (2012) Understanding efflux in Gram-negative bacteria: opportunities for drug discovery. Expert Opin Drug Discovery 7(7):633–642
Sabbagh P, Ebrahimzadeh-Namvar A, Ferdosi-Shahandashti E, Javanian M, Khafri S, Rajabnia M (2017) Molecular characterization of Staphylococcus aureus strains isolated among hospital staff nasal carriers of Babol, Iran. Caspian J Intern Med 8(4):311
Ramírez-Lázaro MJ, Lario S, Casalots A, Sanfeliu E, Boix L, García-Iglesias P, Sanchez-Delgado J, Montserrat A, Bella-Cueto MR, Gallach M (2011) Real-time PCR improves Helicobacter pylori detection in patients with peptic ulcer bleeding. PLoS One 6(5):e20009
Amirhooshang A, Ramin A, Ehsan A, Mansour R, Shahram B (2014) High frequency of Helicobacter pylori DNA in drinking water in Kermanshah, Iran, during June–November 2012. J Water Health 12(3):504–512
Atapoor S, Dehkordi FS, Rahimi E (2014) Detection of Helicobacter pylori in various types of vegetables and salads. Jundishapur J Microbiol 7 (5)
Whitmire JM, Merrell DS (2012) Successful culture techniques for Helicobacter species: verification of Helicobacter identity using 16S rRNA gene sequence analysis. Methods Mol Biol 921:37–40
Acknowledgements
The authors gratefully thank the Department of Infectious Diseases of Babol University of Medical Sciences, Iran.
Author information
Authors and Affiliations
Contributions
P.S and S.E conceived the study; M.M.A, M. J, A. B, V. K, V.K.R.V, H.R.N, and S.E collected all data; P.S and S.E drafted the manuscript; and all authors commented on the drafts of the manuscript and approved the final draft of the paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
This study received the approval from the Babol University of Medical Science, Ethical Committee.
Informed consent
There is no informed consent for this review article.
Rights and permissions
About this article
Cite this article
Sabbagh, P., Mohammadnia-Afrouzi, M., Javanian, M. et al. Diagnostic methods for Helicobacter pylori infection: ideals, options, and limitations. Eur J Clin Microbiol Infect Dis 38, 55–66 (2019). https://doi.org/10.1007/s10096-018-3414-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-018-3414-4