Abstract
Periprosthetic joint infection (PJI) is a catastrophic complication after total joint arthroplasty. It has always been difficult to diagnose PJI, which is characterised by existence of biofilm around the implants. The application of sonication has proven advantageous for pathogen detection. This meta-analysis of clinical trials was performed to evaluate the diagnostic value of sonication and to compare it with traditional bacterial culture. We assessed 16 studies that evaluated sonication fluid cultures (SFC) for the diagnosis of PJI. It was shown that sonication may be of great value in PJI diagnosis, with a pooled sensitivity of 0.79 (95 % confidence interval [CI] = 0.76–0.81), specificity of 0.95 (CI = 0.94–0.96), DOR of 71.20 (CI = 31.08–163.10), PLR of 15.25 (CI = 6.44–36.15), and NLR of 0.23 (CI = 0.18–0.30). The AUC value of the SROC was 0.90. The results of this meta-analysis showed that culture of fluid after sonication was of great value for PJI diagnosis. Sonication was more sensitive than traditional tissue culture with lower specificity, especially for patients previously taking antibiotics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total joint arthroplasty (TJA) is among the most effective and widely performed surgical operations, and this procedure significantly improves quality of life and relieves pain [1]. Given the considerable development and achievement of total joint replacements over the past several decades, the major focus has switched to minimizing surgical complications to further improve long-term outcomes and lower costs [2].
Periprosthetic joint infection (PJI) is the most catastrophic complication seen in TJA [3]. It is reported that the incidence of PJI varied from 1 to 12 % [4, 5]. Meanwhile, PJI requires additional surgeries, antimicrobial therapies, and prolonged hospitalization, with higher risk of disability [6]. According to conservative estimates, the treatment of PJI costs $50,000 [7, 8].
For effective management of PJI, receiving timely treatment is important [9]. The application of anti-bacterial agents has been regarded as playing an important role in treating PJI. The isolation and identification of the pathogen and susceptibility testing are pivotal for appropriate antimicrobial choice, yet this is challenging. Currently, cultures of synovial fluid and intraoperative periprosthetic tissue are considered to be the gold standard for diagnosing PJI. However, its sensitivity and specificity are imperfect, leaving considerable numbers of missed diagnoses [10]. Researchers hypothesized that the forming biofilm protects pathogens around the prosthesis from detection and elimination [11]. Neither specificity nor sensitivity is realised as a result of biofilm and contaminants from skin flora [12].
Several studies have assessed the diagnostic value of sonication techniques for diagnosing PJI, in which long-wave ultrasound was applied before culture to dislodge the bacteria growing within the biofilm and enhance bacterial growth [13]. It has been reported that some cases of aseptic failure are missed cases of PJI [14]. Even in patients receiving antimicrobial therapy within 14 days before surgery, the application of sonication cultures was more sensitive than tissue culture [10]. However, the sensitivities and specificities among studies were inconsistent, and the sample size of any single study was not sufficiently large [14]. There have been several new clinical studies since the last diagnostic meta-analysis [15]. In addition, we still did not know whether the sensitivity and specificity of sonication is better than tradition tissue culture. Therefore, the aim of our study was to perform an updated meta-analysis to evaluate the detection validity of sonication for PJI to provide further evidence for its clinical use, especially compared with traditional tissue culture.
Material and methods
This study was conducted according to the recommendations of the Cochrane Collaboration’s Diagnostic Test Accuracy Group [16]. Electronic and manual search of the literature was performed, and all clinical trials before 2016 related to application of sonication in PJI diagnosis were evaluated.
Eligibility criteria
Studies considered for inclusion met the following criteria: (1) the study reported the application of sonication in the diagnosis of PJI in comparison with traditional culture; (2) the diagnostic criteria were appropriate, such as visible purulence in the synovial fluid or surrounding the prosthesis, acute inflammation on histopathological examination of permanent tissue sections, a sinus tract communicating with the prosthesis, or positive detection in at least two tissue samples culture; (3) sufficient data of true-positive (TP), false-negative (FN), false-positive (FP), and true-negative (TN) values were reported.
Search strategy
Electronic database searches were conducted using Mesh and text keywords “sonication OR ultrasound”, “infection”, “joint” and a combination of these terms, in the title, abstract and keyword fields. Only clinical trials were chosen. The major medical databases were covered, which included MEDLINE, EBSCO, COCHRANE library, EMbase and OVID. No language restrictions were set. Chinese databases, CNKI and VIP, were also covered. References from these trials were scrutinized to reveal additional citations using a manual approach. Duplicated articles were deleted in Endnote software.
Quality assessment
Two reviewers independently screened the retrieved clinical studies for inclusion, extracted data from all included studies and conducted the quality assessment. The aggregate quality of the included studies was evaluated according to the modified version of the QUADAS-2 tool [17]. If agreement was not achieved at any stage, a third reviewer adjudicated.
Data extraction
Data extraction and quality assessment were completed independently by two reviewers according to the inclusion criteria. Information about sample size, diagnostic criteria, ultrasonic conditions, tissue samples and diagnostic outcomes were abstracted independently. If agreement was not achieved at any stage, a third reviewer adjudicated.
Statistical analysis
For the analysis of diagnostic value of sonication, eligible trials were entered into Meta-DiSc software (version 1.4). Analysis of heterogeneity between studies was conducted using the χ 2 test. If there was no significant heterogeneity between studies (P > 0.1, I 2 ≤ 50 %), the analysis was performed using a fixed-effects model; otherwise, the random-effects model (P ≤ 0.1, I 2 > 50 %) was used. The specificity, sensitivity, positive likelihood ratio (PLR), negative likelihood ratio (NLR), diagnostic odds ratio (DOR), and area under the curve (AUC) of summary receiver operating characteristic (SROC) were assessed. Comparison of sonication with traditional culture was analysed in Review Manager 5 software (version 5.1.2). The results were expressed as relative risk (RR) with 95 % confidence intervals (CIs) for dichotomous outcomes. Heterogeneity across trials was assessed via a standard chi-square test with significance being set at P < 0.10 and also assessed by means of I 2 statistic with significance being set at I 2 > 50 %.
Results
A total of 632 articles were identified by the literature search, and the flow diagram is shown in Fig. 1. After literature review of the title, abstract and full text of the articles, 17 studies were chosen as possible references; however, one did not provide data details and was excluded [1]. Finally, a total of 16 studies were recruited for the diagnostic meta-analysis, all of which were of moderate to high quality (Figs. 2 and 3). Fourteen studies were included that compared sensitivity of sonication with traditional, 13 studies compared specificity and four studies compared specificity in patients with previous antibiotic treatment. The baseline of the studies is described in Table 1.
Diagnostic value of sonication
No threshold effect existed (Spearman correlation coefficient: 0.065, P = 0.81) in the pooled data. Heterogeneity was detected in sensitivity (I 2 = 65.8 %), specificity (I 2 = 91.2 %), DOR (I 2 = 81.3 %), PLR (I 2 = 93.7 %), and NLR (I 2 = 67.2 %); thus, the random-effects model was used. Pooling the results (Figs. 4, 5, 6, 7 and 8) produced the following summary estimates and 95 % confidence intervals (CIs): sensitivity 0.79 (0.76–0.81), specificity 0.95 (0.94–0.96), DOR 71.20 (31.08–163.10), PLR 15.25 (6.44–36.15), and NLR 0.23 (0.18–0.30). The SROC plot (Fig. 9) showed the summary sensitivity and specificity and the 95 % confidence and prediction regions, with an AUC of 0.90. We used likelihood ratios to simulate low, moderate, and high clinical scenarios using 25, 50, and 75 % pre-test probabilities of PJI and further calculated and plotted post-test probability on Fagan nomograms (Fig. 10–12). Positive sonication fluid cultures resulted in post-test probabilities of 85, 95, and 98 %, and negative sonication fluid cultures resulted in post-test probabilities of 7, 18, and 39 %. Subgroup analysis was performed by dividing the studies into subgroups according to procedures such as vortexing, centrifugation, culture period and cut-off (Table 2).
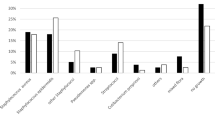
Comparison with traditional tissue culture
Six studies provided the data for both sonication and tissue culture. Analysis of the synthesized data, shown in Fig. 13, revealed that the application of sonication was more sensitive than traditional tissue culture (P < 0.0001) without heterogeneity among the studies (P = 0.74, I 2 = 0 %). However, there was no significant difference with regard to specificity between the two options (P = 0.44), with between-study heterogeneity (P = 0.48, I 2 = 0 %) analysed from five included studies using a random effects model (Fig. 13).
For patients who received antibiotic therapy within 14 days in four studies (Fig. 14), sonication performed better than traditional tissue culture (P = 0.00), with no heterogeneity (P = 0.98, I 2 = 0 %).
Discussion
Currently, the only effective treatment for biofilm infection is to remove the implant, fight the infection with antibiotics, and replace the implant, which is a costly and stressful procedure. PJI can result in a disaster, not only for the patient but also for society because of expensive treatments, multiple required surgeries and long hospital stays [4]. Although considerable effort has already been expended, the incidence of PJI had not been significantly reduced. It was reported that PJI occurred in approximately 1 % of the joints after primary hip or shoulder arthroplasty, 2 % after knee arthroplasty, and up to 9 % after elbow arthroplasty [18].
Detection of pathogens from PJI patients in a rapid, convenient, and economic method is still challenging for researchers and surgeons. It was always a consensus that the diagnosis of PJI was challenging because the diagnostic tests were inaccurate [19]. Currently, periprosthetic tissue culture was regarded as the “gold standard” for microbiological diagnosis of PJI, yet this method yielded considerable false positives and false negatives [3]. Recovery of the pathogens is essential to bacterial culture and selection of antibiotics [6]. However, the biofilm protected the bacteria from being detected and attacked by antibiotics, which prevented recovery.
A series of new technologies was applied to promote diagnosis of PJI, including sonication. It was reported that long-wave ultrasound would dislodge the bacteria growing within the biofilm and enhance bacterial growth [13]. Although sonication presented improved detection in diagnosing urinary tract infection [20] and contamination of electrophysiological cardiac devices [21], the efficacy of sonication for detection in PJI was controversial. Our results showed that the application of sonication may be of great value in PJI diagnosis with a pooled sensitivity of 0.79 (95 % confidence interval [CI] = 0.76–0.81), specificity of 0.95 (CI = 0.94–0.96), DOR of 71.20 (CI = 31.08–163.10), PLR of 15.25 (CI = 6.44–36.15), and NLR of 0.23 (CI = 0.18–0.30). The AUC value of the SROC curve was 0.90. According to the above data, sonication should be regarded as a reliable method to diagnose PJI with the meta-analysis pooled sensitivity and specificity aspiration culture as 72 and 95 %, respectively. Furthermore, the last meta-analysis of 12 studies reported the pooled sensitivity of 0.80 (0.74–0.84) and specificity of 0.95 (0.90–0.98). The results were similar to our analysis, which included four additional clinical studies.
It was reported that ultrasound could release more bacteria from protection of the biofilm without decreasing its activity. Compared with traditional tissue culture, sonication was less specific, but more sensitive in patients with and without previous antibiotics. The results of this meta-analysis suggested that sonication before culture improves microbial recovery in comparison to conventional periprosthetic tissue culture, making it a valid approach and adding important insight into the diagnosis of PJI. Additionally, it could be concluded from the subgroup analysis that the application of vortexing and centrifugation could improve specificity for detecting PJI. Intuitively, sonication would not lead to additional costs or complexity. To assess the value of sonication, cost-effectiveness studies should be conducted. Furthermore, it should be highlighted that sonication can serve as a valuable additional tool for diagnosing PJI, as antibiotic susceptibility testing could be performed more efficiently for adequate treatment.
Preoperative administration of antimicrobial therapy can significantly affect the diagnosis of PJI. Even after stopping antibiotic therapy 14 days before tissue culture, which was usually chosen in clinical practice, the sensitivity was not ideal [22]. It was speculated that this was because planktonic bacteria present in tissue were more susceptible to antimicrobial agents and were killed upon antibiotic therapy. However, bacteria within the biofilm were difficult to kill and be cultured. On this occasion, the application of sonication demonstrated an advantage in dislodging the bacteria out of the biofilm and enhancing its growth, leading to higher sensitivity.
The use of sonication to detect the pathogens is promising. Ultrasound had been used in multiple applications, is well accepted, and has few if any side effects. Using ultrasound, the biofilm-infected device can be specifically targeted. The disadvantages of sonication lay in its false-positive determinations coming from contamination, frequently caused by coagulase-negative Propioni bacterium or Staphylococcus (CNS). Contamination was thought to occur in transportation to the diagnostic unit, especially due to leakages in plastic transport bags. Interestingly, Esteban [23] reported that organisms isolated as contributing to false positives were all non-fermenter, gram-negative rods or uncommon isolates (environmental mycobacteria and fungi) with a low pathogenic potential for humans, and none of these patients had clinical symptoms. Compared to the high number of colonies detected at the surface of the implants, with the absence of these organisms in control cultures from the sonicator, the authors believed that these organisms could have contributed to the “aseptic loosening” of the implants without causing clinical infection.
Conclusions
The results of meta-analysis showed that culture of fluid after sonication was of great value for PJI diagnosis. This technique was more sensitive than traditional tissue culture with lower specificity, especially for patients with previous antibiotic treatment. Sonication was simple and could be performed in most microbiology laboratories. Further study should focus on the optimal sonication working parameters, and situations with high isolate colony counts but without clinical symptoms need to be better distinguished as contaminants or pathogens [23].
References
Achermann Y, Vogt M, Leunig M, Wust J, Trampuz A (2010) Improved diagnosis of periprosthetic joint infection by multiplex PCR of sonication fluid from removed implants. J Clin Microbiol 48(4):1208–1214. doi:10.1128/jcm.00006-10
Anguita-Alonso P, Hanssen AD, Patel R (2005) Prosthetic joint infection. Expert Rev Anti-Infect Ther 3(5):797–804. doi:10.1586/14787210.3.5.797
Springer BD (2015) The diagnosis of periprosthetic joint infection. J Arthroplasty 30(6):908–911
Qu X, Zhai Z, Li H, Li H, Liu X, Zhu Z, Wang Y, Liu G, Dai K (2013) PCR-based diagnosis of prosthetic joint infection. Europace 15(4):595–600
Vrgoc G, Japjec M, Gulan G, Ravlićgulan J, Marinović M, Bandalović A (2014) Periprosthetic infections after total hip and knee arthroplasty—a review. Coll Antropol 38(4):1259–1264
Holinka J, Bauer L, Hirschl AM, Graninger W, Windhager R, Presterl E (2011) Sonication cultures of explanted components as an add-on test to routinely conducted microbiological diagnostics improve pathogen detection. J Orthop Res Off Publ Orthop Res Soc 29(29):617–622
Bozic KJ, Ong K, Lau E, Kurtz SM, Vail TP, Rubash HE, Berry DJ (2010) Risk of complication and revision total hip arthroplasty among medicare patients with different bearing surfaces. Clin Orthop Relat Res 468(9):2357–2362
Kurtz S, Ong K, Lau E, Mowat F, Halpern M (2005) Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 87(7):1487–1497
Zimmerli W, Trampuz A, Ochsner PE (2004) Prosthetic-joint infections. N Engl J Med New Engl J Med 351(16):1645–1654
Trampuz A, Piper KE, Jacobson MJ, Hanssen AD, Unni KK, Osmon DR, Mandrekar JN, Cockerill FR, Steckelberg JM, Greenleaf JF (2007) Sonication of removed hip and knee prostheses for diagnosis of infection. N Engl J Med 357(357):654–663
Donlan RM (2005) New approaches for the characterization of prosthetic joint biofilms. Clin Orthop Relat Res 437(437):12–19
Atkins BL, Athanasou N, Deeks JJ, Crook DW, Simpson H, Peto TE, McLardy-Smith P, Berendt AR (1998) Prospective evaluation of criteria for microbiological diagnosis of prosthetic-joint infection at revision arthroplasty. The OSIRIS Collaborative Study Group. J Clin Microbiol 36(10):2932–2939
Carmen JC, Roeder BL, Nelson JL, Ogilvie RLR, Robison RA, Schaalje GB, Pitt WG (2005) Treatment of biofilm infections on implants with low-frequency ultrasound and antibiotics. Am J Infect Control 33(2):78–82
Trampuz A, Piper KE, Hanssen AD, Osmon DR, Cockerill FR, Steckelberg JM, Patel R (2006) Sonication of explanted prosthetic components in bags for diagnosis of prosthetic joint infection is associated with risk of contamination. J Clin Microbiol 44(2):628–631
Zhai Z, Li H, Qin A, Liu G, Liu X, Wu C, Li H, Zhu Z, Qu X, Dai K (2014) Meta-analysis of sonication fluid samples from prosthetic components for diagnosis of infection after total joint arthroplasty. J Clin Microbiol 52(5):1730–1736
The Cochrane Collaboration (2016) Handbook for DTA reviews. Diagnostic Test Accuracy Working Group, The Cochrane Collaboration. http://srdta.cochrane.org/handbook-dta-reviews. Accessed 15 September 2016
Whiting PF, Rutjes AWS, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, Leeflang MMG, Sterne JAC, Bossuyt PMM (2011) QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155(8):529–536
Phillips JE, Crane TP, Noy M, Elliott TS, Grimer RJ (2006) The incidence of deep prosthetic infections in a specialist orthopaedic hospital: a 15-year prospective survey. Bone Joint J 88(7):943–948
Trampuz A, Osmon DR, Hanssen AD, Steckelberg JM, Patel R (2003) Molecular and antibiofilm approaches to prosthetic joint infection. Clin Orthop Relat Res 76(414):69–88
Holá V, Ruzicka F, Horka M (2010) Microbial diversity in biofilm infections of the urinary tract with the use of sonication techniques. FEMS Immunol Med Microbiol 59(3):525–528
Rohacek M, Weisser M, Kobza R, Schoenenberger AW, Pfyffer GE, Frei R, Erne P, Trampuz A (2010) Bacterial colonization and infection of electrophysiological cardiac devices detected with sonication and swab culture. Circulation 121(15):1691–1697
Connaughton A, Childs A, Dylewski S, Sabesan VJ (2014) Biofilm disrupting technology for orthopedic implants: what’s on the horizon? Front Med 1(01):22
Esteban J, Gomez-Barrena E, Cordero J, Martín-de-Hijas NZ, Kinnari TJ, Fernandez-Roblas R (2008) Evaluation of quantitative analysis of cultures from sonicated retrieved orthopedic implants in diagnosis of orthopedic infection. J Clin Microbiol 46(2):488–492
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by the Guangdong Provincial Natural Science Foundation of China (2014A030310241), the Foundation of President of Nanfang Hospital (2014C018), and the National Natural Science Foundation of China (81501904).
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The ethics approval was not needed.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Liu, H., Zhang, Y., Li, L. et al. The application of sonication in diagnosis of periprosthetic joint infection. Eur J Clin Microbiol Infect Dis 36, 1–9 (2017). https://doi.org/10.1007/s10096-016-2778-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-016-2778-6