Abstract
Helicobacter pylori infection (HPI) imposes substantial social costs and is of major etiological importance in peptic ulcer disease, gastric cancer, and accelerated cardiovascular diseases. This study determined the risk of acute coronary syndrome (ACS) associated with HPI in a nationwide retrospective cohort study. By using the Taiwan National Health Insurance Research Database (NHIRD), we identified patients diagnosed with HPI from 1998 to 2010. In addition, we randomly selected non-HPI controls frequency-matched by age, sex, and index year from the general population free of HPI. The risk of ACS was analyzed using Cox proportional hazards regression models in which sex, age, and comorbidities were included as variables. We identified 17,075 participants for the HPI group and selected 68,300 participants for the comparison group. The incidence rates were increased in the patients in the HPI group compared with those in the comparison group. Overall, the HPI patients exhibited a 1.93-fold high crude hazard ratio for ACS, and a 1.48-fold adjusted hazard ratio after age, sex, and comorbidities were adjusted. However, the overall adjusted hazard ratio of ACS increased with increasing age with a 3.11 to 8.24 adjusted hazard ratio among the various age groups. Several comorbidities, such as diabetes, hyperlipidemia, and COPD exhibited synergistic effects for ACS risk. We determined a significant association between ACS and comorbidities and provide evidence to encourage clinicians to observe ACS-related comorbidities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiovascular disease (CVD) is the second leading cause of death in Taiwan [1]. Acute coronary syndrome (ACS) is a critical stage of the clinical manifestation of coronary artery disease (CAD) in CVD [2]. ACS results in substantial morbidity and mortality, accounting for half of all deaths from CVD and contributing to the heavy economic burden of the disease [3].
The effective treatment of ACS is guided by early diagnosis and risk stratification to predict those who are at high risk of short- and long-term adverse outcomes. A family history of premature coronary heart disease (CHD), modifiable risk factors such as hyperlipidemia [4], hypertension, diabetes, and metabolic syndrome [5], and non modifiable risk factors such as sex and age, can be used to predict atherosclerosis development and the risk of presenting with ACS [6].
Atherosclerosis is by far the most frequent cause of CAD. Life-threatening manifestations are typically precipitated by acute thrombosis superimposed on ruptured or eroded atherosclerotic plaque [7]. Multiple factors contribute to the pathogenesis of atherosclerosis, including endothelial dysfunction, dyslipidemia, inflammatory and immunological factors, plaque rupture, and smoking [8].
The importance of inflammation in the pathogenesis of atherosclerosis derives from the fact that markers of increased or decreased systemic inflammation are associated with the risk of atherosclerosis [9]. Evidence for inflammation in atherosclerotic lesions was obtained from early histological observations, and inflammation is central to understanding the pathogenesis of atherosclerosis [10].
Microbe infection could act according to a number of mechanisms, including direct vascular injury and induction of a systemic inflammatory state, such as that induced by Helicobacter pylori (HP) infection (HPI) [11].
HPI is the most common chronic bacterial infection of the human upper gastrointestinal tract [12]. Conservative estimates suggest that half of the world’s population is infected with HP [13]. HP is a microaerophilic spiral-shaped Gram-negative bacterium that colonizes the gastric lumen of humans and other primates and is of major etiological importance in peptic ulcer disease and gastric cancer [14]. Increasing evidence from both clinical and experimental observations suggests that inflammation plays a crucial role in CAD Fibre15].
However, subsequent studies have produced conflicting findings. Whether this relationship with inflammation arises from the bacterium itself or its association with other confounding factors related to atherosclerosis, such as a low socioeconomic class, old age, and smoking, primarily modifiable risk factors, such as hyperlipidemia, hypertension, diabetes, and metabolic syndrome, or non-modifiable risk factors, such as sex and age, remains uncertain [17–19]. Confounding by the strong relationship of HPI to other coronary heart disease risk factors, such as age and socioeconomic class may, at least partially, explain the conflicting results that have been obtained [20].
A large population-based study may help clarify the effect of such confounding factors. Therefore, we conducted an investigation by using records from the Taiwan National Health Insurance Research Database (NHIRD) to evaluate whether HPI patients are at risk of developing ACS after accounting for traditional risk factors of ischemic heart disease. The results of this study are provided as a reference to the public and medical professionals.
Materials and methods
Study design and data source
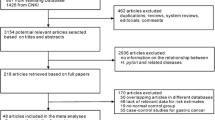
We used the Taiwan NHIRD to conduct a population-based retrospective cohort study. This database was established in 1995 when the Taiwan National Health Insurance (NHI), a comprehensive insurance program, was launched by the Taiwan Department of Health. The NHI covers 99.9 % of the population of Taiwan. The Taiwan National Health Research Institute is responsible for managing various databases, including the registration files of the insured and claims data for reimbursement. Before releasing the electronic files for study, the personal identification numbers were encrypted to protect patient privacy. We used the inpatient claims data as the datasets, and the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) was used to define diseases. The Institutional Review Board of China Medical University (CMU-REC-101-012) approved this study from full ethical review.
Study population
From the inpatient claims data, we selected patients who were newly diagnosed with HPI (ICD-9-CM 041.86) from 1998 to 2010 as the HPI group. For the comparison group, we randomly selected people from the general population who were 4-fold frequency-matched by age, sex, and diagnosis year. We excluded patients with a history of HPI and those with incomplete age or sex information at the baseline. Patients who had a history of comorbidities, such as hypertension (ICD 401–405), diabetes (ICD-9-CM codes 250), hyperlipidemia (ICD-9-CM codes 272), stroke (ICD-9-CM codes 430–438), chronic obstructive pulmonary disease (COPD) (ICD-9-CM codes 490–492,494, and 496), and heart failure (ICD-9-CM 428) were included in this study. Both groups were followed up until the observation of an ACS (ICD-9-CM 410, 411.1, and 411.8) event or the end of the study period (December 31, 2010).
Statistical analysis
To compare the distributions of demographic variables and comorbidities between the HPI group and non-HPI group, we analyzed the categorical variables by using a chi-squared test. Two sample t tests were used to determine differences in the continuous variables, such as mean age, between the two groups. The sex-, age- and comorbidity-specific incidence densities of ACS per 1,000 person-years of follow-up for each cohort were estimated. The crude hazard ratio (HR) with a 95 % confidence interval (CI) of the HPI group to the comparison group was calculated using univariable Cox proportional hazards regression. Multivariable Cox proportional hazards regression was used to measure the adjusted HR (aHR) of ACS for the HPI group, compared with non-HPI group, after controlling for sex, age, and comorbidities. The interactional effects between the comorbidities and HPI were also assessed using Cox models. All of the statistical analyses in this study were performed using the SAS 9.1 statistical package (SAS Institute Inc., NC, USA). P < 0.05 in 2-tailed tests was considered significant.
Results
We identified 17 075 patients for the HPI group and selected 68 300 participants for the comparison group (Table 1). After frequency matching, both groups had similar sex and age distributions and more men (62.9 %) and younger participants (34.8 %, ≤49 y). Comorbidities were more prevalent in the HPI group than in the non-HPI group (P < .0001).
The incidence of ACS was 1.93-fold higher in the HPI group than in the non-HPI group (6.41 vs 3.33 per 1,000 person-years; aHR = 1.48, 95 % CI = 1.30–1.69) (Table 2). In both groups, the risks of developing HPI were higher for men than for women. Analysis by sex yielded an aHR of 1.38 (95 % CI = 1.09–1.76) for the women and 1.53 (95 % CI = 1.31–1.79) for the men, compared with the non-HPI group.
The risks of developing ACS increased with increasing age in both groups, with a much greater gradient in the HPI group. The participants with comorbidities exhibited higher incidences of ACS in both groups (12.2 vs 9.35 per 1,000 person-years), and the HPI group exhibited a higher aHR of 1.53 (95 % CI = 1.29–1.80) compared with the non-HPI group.
Table 3 shows that the HPI group was significantly associated with the development of ACS. The risks of developing ACS increased as age increased. The aHR of ACS was 1.63 times higher among men than among women (95 % CI = 1.44–1.85). Compared with the participants without comorbidities, patients with comorbidities such as hypertension (aHR = 1.59; 95 % CI = 1.37–1.84), diabetes (aHR = 2.03; 95 % CI = 1.75–2.36), hyperlipidemia (aHR = 1.59; 95 % CI = 1.28–1.97), COPD (aHR = 1.41; 95 % CI = 1.16–1.71), heart failure (aHR = 1.50; 95 % CI = 1.12–2.00), and stroke (aHR = 1.14; 95 % CI = 0.95–1.36) exhibited a greater risk for developing ACS (all P < 0.05 except for stroke).
We also estimated risk of ACS in relation to HPI, hypertension, diabetes, hyperlipidemia, COPD, and heart failure, and the interaction among these factors (Table 4). The risk of developing ACS in patients with HPI increased with the existence of any comorbidity. HPI was observed to have an interaction with hyperlipidemia (P = 0.009) and COPD (P = 0.01). When HPI and hyperlipidemia were present, the aHR was 4.20 (95 % CI = 3.19–5.54), compared with the participants without HPI and hyperlipidemia. The aHR was 2.66-fold higher in the HPI patients with COPD than in the non-HPI/non-COPD participants (95 % CI = 2.01–3.52).
Discussion
We compared patients with HPI matched by age, sex, and history of comorbidities at the baseline, such as hypertension, hyperlipidemia, stroke, COPD, and heart failure. The risk of developing ACS in patients with HPI increased with the presence of any comorbidity. HPI had a synergistic interaction with hyperlipidemia (P = 0.009) and COPD (P = 0.01). The presence of both HPI and hyperlipidemia yielded an aHR of 4.20 (95 % CI = 3.19–5.54) compared with participants without HPI and hyperlipidemia. Patients with COPD yielded an aHR 2.66-fold higher than among non-HPI/non-COPD participants (95 % CI = 2.01–3.52). After age and other comorbidities were adjusted for, the results of this study suggested an inverse significant biological gradient for the development of the risk of ACS between the HPI and non-HPI groups.
Previous studies [21] on South Korean adults have shown that HPI is associated with cardiovascular risk factors, particularly levels of triglycerides, HDL-cholesterol, and apolipoproteins, independent of the presence of peptic ulcers. A study from India [22] reported that HPI and diabetes exacerbated glucose tolerance and CHD development. The colonization of CagA-positive HP does not seem to be an independent risk factor for severe CHD [27]. Previous studies provided evidence that HPI stimulates a cascade of inflammation, and subsequent immune responses include cellular and humoral immunity between T and B lymphocytes [24, 25], even bacterial colonization, persistence, virulence, and resulting innate and adaptive immunity play a crucial role in HP-related disease [26, 27]. However, HPI may influence atherogenesis through low-grade, persistent inflammatory stimulation [28] and is significantly associated with risk of short-term adverse outcomes [29]. The reduction in restenosis of coronary vessels after HP eradication could be interpreted as evidence of the involvement of an HP inflammatory process. Kowalski et al. stated that HP-eradication therapy may prolong the hospitalization-free period for patients with recurrent chest pain [30, 31]. Taiwan and other developing and underdeveloped countries [32, 33] have a high prevalence of HPI; thus, the eradication of HPI may reduce the emerging burden of CVD. Investigating more aggressive HPI and treatment for the disease may be necessary. Randomized controlled trials are required to evaluate the role of HP eradication in these patients. PPIs (proton pump inhibitors) have been shown to decrease the antiplatelet effects of clopidogrel ex vivo [34], raising concerns about the cardiovascular safety of this drug combination. Therefore, more caution when using PPIs for HP eradication is necessary.
This study used NHIRD claims data and as such has several limitations. The NHI database does not disclose patients’ personal histories, socioeconomic status, serum laboratory data, smoking status, or inflammatory markers. And the diagnoses of HPI were involved in several different methods, including blood antibody test, stool antigen test, or carbon urea breath test [35]. However, the most reliable protocol for HPI detection is a biopsy check during endoscopy with a rapid urease test, histological examination, and microbial culture which is only one way for requested insurance benefit in the NHIRD of Taiwan. Therefore the investigation of HPI activity or severity might not be accurately determined in claim data. We could not adjust for environmental factors, such as smoking habits, etc. The evidence suggests that smokers have a risk of ACS, which is compatible with the results of other studies [36]. This may account for much of the risk reduction for smoking-related ACS. However, HPI is not directly related to smoking. Data unadjusted for smoking status may reflect this possible relationship more adequately. In several case–control studies for proved association of HPI and ACS, there were less causal relationship evidence for clarification of HPI and ACS. We used the NHIRD to improve the evidence for clinical significance between HPI and ACS [36]. However, we need further approaches to clarify the relationship between different environmental factors, such as drugs, smoking habits and other individual exposed information, to account for the excessive risk for HPI-related ACS after adjustment for common risk factors for ACS. In the future it would be possible to clarify the detailed exposed information and intervening genetic factors of the host by the National Taiwan Biobank [37].
Conclusion
In this study, we determined a significant association between ACS and comorbidities and provide evidence to encourage clinicians to observe ACS-related comorbidities which might improve preventive ACS complications in the HPI population.
References
Directorate-General of Budget, Accounting and Statistics Executive Yuan, Republic of China (2010) Statistical yearbook of the Republic of China. Health 114
Lin YS, Liu PH, Wu LS, Chen YM, Chang CJ, Chu PH (2014) Major adverse cardiovascular events in adult congenital heart disease: a population-based follow-up study from Taiwan. BMC Cardiovasc Disord 14:38
Chang KC, Tseng MC (2003) Costs of acute care of first-ever ischemic stroke in Taiwan. Stroke 34:e219–e221
Regnström J, Jovinge S, Båvenholm P, Ericsson CG, De Faire U, Hamsten A et al (1998) Helicobacter pylori seropositivity is not associated with inflammatory parameters, lipid concentrations and degree of coronary artery disease. J Intern Med 243:109–13
Ongey M, Brenner H, Thefeld W, Rothenbacher D (2004) Helicobacter pylori and hepatitis a virus infections and the cardiovascular risk profile in patients with diabetes mellitus: results of a population-based study. Eur J Cardiovasc Prev Rehabil 11:471–476
Lu YH, Yen HW, Lin TH, Huang CH, Lee KT, Wang WM et al (2002) Changes of coronary risk factors after eradication of Helicobacter pylori infection. Kaohsiung J Med Sci 18:266–272
Hara K, Morita Y, Kamihata H, Iwasaka T, Takahashi H (2001) Evidence for infection with Helicobacter pylori in patients with acute myocardial infarction. Clin Chim Acta 313:87–94
Mair J, Jaffe AS (2014) Biomarker tests for risk assessment in coronary artery disease: will they change clinical practice? Mol Diagn Ther 18:5–15
Wang Y, Wang GZ, Rabinovitch PS, Tabas I (2014) Macrophage mitochondrial oxidative stress promotes atherosclerosis and nuclear factor-κB-mediated inflammation in macrophages. Circ Res 114:421–433
Grufman H, Gonçalves I, Edsfeldt A, Nitulescu M, Persson A, Nilsson M et al (2014) Plasma levels of high-sensitive C-reactive protein do not correlate with inflammatory activity in carotid atherosclerotic plaques. J Intern Med 275:127–133
Khan S, Rahman HN, Okamoto T, Matsunaga T, Fujiwara Y, Sawa T et al (2014) Promotion of atherosclerosis by Helicobacter cinaedi infection that involves macrophage-driven proinflammatory responses. Sci Rep 4:4680
Pounder RE, Ng D (1995) The prevalence of Helicobacter pylori infection in different countries. Aliment Pharmacol Ther 9:33–40
Brown LM (2000) Helicobacter pylori: epidemiology and routes of transmission. Epidemiol Rev 22:283–97
Axon AT (2007) Relationship between Helicobacter pylori gastritis, gastric cancer and gastric acid secretion. Adv Med Sci 52:55–60
Kowalski M, Pawlik M, Konturek JW, Konturek SJ (2006) Helicobacter pylori infection in coronary artery disease. J Physiol Pharmacol 57:101–111
Elizalde JI, Gómez J, Panés J, Lozano M, Casadevall M, Ramírez J et al (1997) Platelet activation in mice and human Helicobacter pylori infection. J Clin Invest 100:996–1005
Mendall MA, Goggin PM, Molineaux N, Levy J, Toosy T, Strachan D et al (1994) Relation of Helicobacter pylori infection and coronary heart disease. Br Heart J 71:437–439
Whincup PH, Mendall MA, Perry IJ, Strachan DP, Walker M (1996) Prospective relations between Helicobacter pylori infection, coronary heart disease, and stroke in middle aged men. Heart 75:568–572
Danesh J, Peto R (1998) Risk factors for coronary heart disease and infection with Helicobacter pylori: meta-analysis of 18 studies. BMJ 316:1130–1132
Patel P, Mendall MA, Carrington D, Strachan DP, Leatham E, Molineaux N et al (1995) Association of Helicobacter pylori and Chlamydia pneumoniae infections with coronary heart disease and cardiovascular risk factors. BMJ 311:711–714
Sung KC, Rhee EJ, Ryu SH, Beck SH (2005) Prevalence of Helicobacter pylori infection and its association with cardiovascular risk factors in Korean adults. Int J Cardiol 102:411–417
Rahman MA, Cope MB, Sarker SA, Garvey WT, Chaudhury HS, Khaled MA (2009) Helicobacter pylori infection and inflammation: implication for the pathophysiology of diabetes and coronary heart disease in Asian Indians. J Life Sci 1:45–50
Rogha M, Dadkhah D, Pourmoghaddas Z, Shirneshan K, Nikvarz M, Pourmoghaddas M (2012) Association of helicobacter pylori infection with severity of coronary heart disease. ARYA Atheroscler 7:138–41
Hussell T, Isaacson PG, Crabtree JE, Spencer J (1996) Helicobacter pylori-specific tumour-infiltrating T cells provide contact dependent help for the growth of malignant B cells in low-grade gastric lymphoma of mucosa-associated lymphoid tissue. J Pathol 178:122–127
Lundgren A, Suri-Payer E, Enarsson K, Svennerholm AM, Lundin BS (2003) Helicobacter pylori-specific CD4+ CD25high regulatory T cells suppress memory T-cell responses to H. pylori in infected individuals. Infect Immun 71:1755–1762
Gewirtz AT, Yu Y, Krishna US, Israel DA, Lyons SL, Peek RM Jr (2004) Helicobacter pylori flagellin evades toll-like receptor 5-mediated innate immunity. J Infect Dis 189:1914–1920
Algood HM, Gallo-Romero J, Wilson KT, Peek RM Jr, Cover TL (2007) Host response to Helicobacter pylori infection before initiation of the adaptive immune response. FEMS Immunol Med Microbiol 51:577–586
Tamer GS, Tengiz I, Ercan E, Duman C, Alioglu E, Turk UO (2009) Helicobacter pylori seropositivity in patients with acute coronary syndromes. Dig Dis Sci 54:1253–1256
Eskandarian R, Ghorbani R, Shiyasi M, Momeni B, Hajifathalian K, Madani M (2012) Prognostic role of Helicobacter pylori infection in acute coronary syndrome: a prospective cohort study. Cardiovasc J Afr 23:131–135
Eskandarian R, Malek M, Mousavi SH, Babaei M (2006) Association of Helicobacter pylori infection with cardiac syndrome X. Singapore Med J 47:704–706
Kowalski M, Rees W, Konturek PC, Grove R, Scheffold T, Meixner H et al (2002) Detection of Helicobacter pylori specific DNA in human atheromatous coronary arteries and its association to prior myocardial infarction and unstable angina. Dig Liver Dis 34:398–402
Longo-Mbenza B, Ngoma DV, Nahimana D, Mayuku DM, Fuele SM, Ekwanzala F et al (2008) Screen detection and the WHO stepwise approach to the prevalence and risk factors of arterial hypertension in Kinshasa. Eur J Cardiovasc Prev Rehabil 15:503–508
Longo-Mbenza B, Nsenga JN, Mokondjimobe E, Gombet T, Assori IN, Ibara JR et al (2012) Helicobacter pylori infection is identified as a cardiovascular risk factor in central Africans. Vasc Health Risk Manag 6:455–461
D'Ugo E, Rossi S, De Caterina R (2012) Proton pump inhibitors and clopidogrel: an association to avoid? G Ital Cardiol (Rome) 13:817–826
Marshall B, Stenström B, Mendis A (2008) Helicobacter pylori: the latest in diagnosis and treatment. Aust Fam Physician 37(8):608
Budzyński J, Koziński M, Kłopocka M, Kubica JM, Kubica J (2014) Clinical significance of Helicobacter pylori infection in patients with acute coronary syndromes: an overview of current evidence. Clin Res Cardiol 1–32
Fan C-T, Lin J-C, Lee C-H (2008) Taiwan Biobank: a project aiming to aid Taiwan’s transition into a biomedical island. Pharmacogenomics 9(2):235–246
Acknowledgments
This work was supported by grants from the China Medical University (CMU102-BC-2), Taiwan Ministry of Health and Welfare Clinical Trial and Research Center of Excellence (MOHW103-TDU-B-212-113002), Health and Welfare Surcharge of Tobacco Products, and the China Medical University Hospital Cancer Research Center of Excellence (MOHW103-TD-B-111-03, Taiwan). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Ching-Yuan Lai and Tse-Yen Yang contributed equally to this study.
Rights and permissions
About this article
Cite this article
Lai, CY., Yang, TY., Lin, CL. et al. Helicobacter pylori infection and the risk of acute coronary syndrome: a nationwide retrospective cohort study. Eur J Clin Microbiol Infect Dis 34, 69–74 (2015). https://doi.org/10.1007/s10096-014-2207-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-014-2207-7