Abstract
In July 2008, in France, guidelines for antibiotic prescriptions for urinary tract infections (UTIs) were amended. As general practitioners (GPs) treat numerous UTIs, we wanted to evaluate whether they followed these guidelines. In order to do this, we performed a prospective study. The point of call was urinalyses. Using this selection method together with criteria diagnostic for urinalysis, we confirmed that patients presented a UTI. Each GP was contacted. Prescriptions were analysed and compared to the 2008 French guidelines for UTIs. Our study included 185 urinalyses. UTIs diagnosed by GPs were as follows: acute cystitis: 72.4 %, prostatitis: 13.5 %, nephritis: 8.7 % and asymptomatic bacteriuria: 5.4 %. The principal antibiotics used were: quinolone (59.5 %), furan (17.8 %) and cotrimoxazole (6.5 %). Only 20 % of the prescriptions were compliant with the guidelines. The correct antibiotic but not the dose or the duration of prescription was selected in 8.1 % of the prescriptions. For cystitis, inappropriate prescription was associated with an extra cost of 694 €, namely, 7.4 € per treatment. GP prescriptions for UTIs do not follow the guidelines. Even if GPs assert that they are aware of the emergence of resistant strains, it seems that they do not take into account the objective of quinolone restriction, which was one of the backbones of these guidelines.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The widespread use of antibiotics leads to the emergence of resistant bacteria. Even if it is mainly seen in hospital-acquired infections, this phenomenon occurs in France in community-acquired infections [1, 2]. In France, more than 80 % of all antibiotics are prescribed by general practitioners (GPs), but they do not seem to be aware that they play a role in the progression of resistances. Among infections widely treated by GPs, urinary tract infections (UTIs) are one of the most frequent. These infections are commonly treated with fluoroquinolones, which are known to easily lead to the development of resistant bacterial strains [3]. In France, approximately 20 % of Escherichia coli are now resistant to fluoroquinolones [4]. In 2008, the French Agency for the Safety of Health Products (AFSSAPS) published new guidelines for UTIs. These guidelines included data for the diagnosis and different treatments for each type of community-acquired UTIs (cystitis, prostatitis, nephritis etc.) in adults [5]. These treatment guidelines are based on bacteriological data, such as the rate of resistant strains, but also with the intent of limiting fluoroquinolone use to avoid the increasing rate of fluoroquinolone-resistant strains. For example, for simple cystitis, fosfomycin trometamol or nitrofurantoine were the preferred antibiotics [5]. For nephritis, intravenous third-generation cephalosporins were proposed, with a relay with amoxicillin, amoxicillin–clavulanate, oral third-generation cephalosporins or sulfamethoxazole–trimethoprim [5].
As these guidelines were published in 2008, the aim of the present study was to evaluate GPs’ antibiotic prescriptions for UTIs in adults who underwent a urinalysis and to see if the goal of quinolone restriction was abided by GPs. In the literature, several studies were performed on the same subject. They find that clinicians poorly follow the guidelines [6–10]. This lack of follow-up could lead to a higher cost [11] because of, for example, a longer course of treatment [9, 12].
Materials and methods
We performed a prospective study during September 2010. This study was conducted in an outpatient context at the Biolyss laboratory (an outpatient biological laboratory in Limoges, France). The laboratory in which the study took place also performs urinalyses for five other laboratories located in the town but also in the suburbs and the rest of the county. Our starting point was urinalyses. All consecutive urinalyses performed in this laboratory were evaluated. Urinalyses were eligible if they fulfilled the following criteria: (i) leucocyte counts greater than 104/ml and bacteria count greater than the cut-off for each type of infection [i.e. >104 colony-forming units(CFU)/ml for nephritis or prostatitis; >103 CFU/ml for cystitis due to E. coli, Proteus spp., Klebsiella spp., Staphylococcus saprophyticus; >105 CFU/ml for cystitis due to other bacteria] and (ii) age over 18 years. Urinalyses were excluded if: (i) they were prescribed by a urologist and (ii) the patient was hospitalised. Urinalyses were anonymous (the staff of the biological laboratory kept the initial of the name and the first name) for confidentiality. GPs were then called on the phone with a delay of no more than 10 days to collect data concerning the diagnosis and antibiotic(s) prescribed after the urinalysis results. Patients with a permanent urinary catheter were secondarily excluded. Data were analysed versus the 2008 French guidelines for the treatment of UTIs.
If the antibiotic used was not one of those recommended, the treatment was considered as “Not adapted”. If the antibiotic was one proposed by the guidelines, the dosage and the length of treatment were checked. Treatments were considered as “Adapted” if the antibiotic, dosage and length of treatment were in agreement with those recommended. For this part, we took into account the type of infection but also their classification as “simple” or “complicated”. When possible, we evaluated the cost of each treatment prescribed by GPs compared to the cost of the recommended treatment (the one that should have been prescribed). The cost was based on the price of antibiotics in outpatient pharmacies. If an intravenous or intramuscular treatment was prescribed, the cost of the material used and the wages of the nurse were taken into account.
We compared the different types of infections to determine whether or not they had an impact on the follow-up of the guidelines. The Chi-square test was used.
Results
A total of 403 urinalyses were performed over the period of the study, among which 240 were eligible according to the inclusion and exclusion criteria. There were 122 GPs who agreed to answer our questions, which represented 80.8 % of the GPs contacted. Among the responses, nine patients had a permanent urinary catheter and were then excluded. Finally, 185 urinalyses were usable in our study. These 122 GPs represented 28.3 % of all the GPs in our county.
The mean age of the patients included in the study was 62 years. The population was mainly composed of women (85.4 %).
The diagnoses carried out by GPs were as follows:
-
Acute simple cystitis: 38.9 % (n = 72)
-
Acute complicated cystitis: 22.2 % (n = 41)
-
Acute recurrent simple cystitis: 5.9 % (n = 11)
-
Acute recurrent complicated cystitis: 4.9 % (n = 9)
-
Acute cystitis during pregnancy: 0.5 % (n = 1)
-
Prostatitis: 13.5 % (n = 25)
-
Acute simple nephritis: 4.9 % (n = 9)
-
Acute complicated nephritis: 2.7 % (n = 5)
-
Acute nephritis during pregnancy: 1.1 % (n = 2)
-
Colonisation: 5.4 % (n = 10)
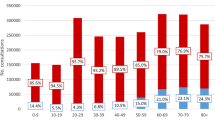
The antibiotics prescribed are shown in Fig. 1, along with their distribution within the different diagnoses. Figure 2 shows the length of prescription of each type of antibiotics according to the diagnosis.
A total of 197 bacteria were found in the 185 urinalyses (all urinalysis revealed bacteria). Gram-negative bacteria were found in 91.4 %. E. coli was found in 143 urinalyses (76.5 %). For E. coli, the resistance rate to furans was 1.4 %, 9.8 % to ciprofloxacin, 13.9 % to norfloxacin and ofloxacin, 20.3 % to cotrimoxazole, 48.3 % to amoxicillin and 40.6 % to amoxicillin–clavulanate.
In only 20 % (n = 37) of the patients, the prescription was “Adapted” as previously defined, i.e. the antibiotic, dosage and length of treatment were as recommended in the guidelines. In 71.4 % (n = 132) of the patients, the antibiotic was not the one recommended as a first line of treatment. In 8.6 % (n = 16) of the patients, the antibiotic was the right one but either the dosage and/or the duration of prescription was incorrect. Dosages errors were due to the use of ciprofloxacin and furan at half the recommended dose. For the duration of therapy, mistakes were principally due to too short courses for prostatitis and too long courses for cystitis.
We were only able to assess the cost for cystitis. Concerning the prescriptions which did not follow the recommendations (n = 94, 70.1 % of all cystitis), the extra expenditure was 694 €, namely, 7.4 € per treatment.
There was a better adapted treatment for nephritis, complicated cystitis and prostatitis than the adapted treatment for cystitis (respectively, p = 0.001; p = 0.009; p = 0.0002). However, there was no statistical difference between the adapted treatment for prostatitis and nephritis (p = 0.9) or between cystitis and recurrent cystitis (p = 0.65).
Discussion
Using urinalysis as a starting point, and following the recommendations for the interpretation of white blood cell counts and CFU counts in the urine, ensured that the patient did or did not have a UTI. Furthermore, based on the bacteriological results, we had some additional elements to use for the interviews of GPs. We found this approach better than asking GPs what they should have prescribed in reported cases to avoid wrong and polite answers.
Our results are concordant with other studies realised around the world where the adherence to guidelines for UTIs is poor. Such reports come, for example, from Spain [6], Israel [7] and the United States [8–10].
Curiously, we had many cystitis cases (72.4 %). This is surprising because the starting point was urinalysis. Indeed, in the guidelines, urinalyses are not recommended for cystitis, unless it is a complicated or recurrent one, which was not the case. This approach has been reported by another team where urinalyses were performed even if dip-sticks were positive [10]. However, this is a good point for our study, as cystitis is the major UTI treated by GPs. Thus, we were able to analyse a type of infection that we should not have been able to recruit using this methodology.
Fluoroquinolones were prescribed in 59.5 % of UTIs in our study. Even if this is not the best choice regarding resistance emergence, this prescription is understandable. Since the discovery of nalidixic acid, quinolones and then fluoroquinolones have been proposed in France as the best choice to treat UTIs (this recommendation is found in the two previous guidelines published in 1991 and 1995). So it stands to reason that, despite the new guidelines, fluoroquinolones still remain the best choice for many practitioners. We reviewed each prescription containing fluoroquinolones to analyse if another antibiotic family could have been prescribed, taking into account the diagnosis, potential allergies and the antibiogram. In 77.3 % (n = 85), quinolones should not have been used. The idea of quinolones limitation advocated by the guidelines is not, for the moment, shared by all practitioners. In a recent study from Norway, but based on data from 2003, only 6 % of the prescriptions were quinolones [12]. So there is a possibility for improvement in French prescriptions.
Among all the quinolones, we only found fluoroquinolones but no first-generation quinolones in the prescriptions given by GPs. This is probably due to the fact that they were already excluded in the previous guidelines. We found no prescription with fourth-generation fluoroquinolones (levofloxacin or moxifloxacin). Even if their use increases, mainly for lung infections, they have, for the moment, no indication for UTIs [13, 14]. Indeed, classical fluoroquinolones (ofloxacin, ciprofloxacin) are still effective in these infections and the new ones do not improve the outcomes in UTIs caused by Gram-negative bacteria. It seems that, for the moment, GPs did not switch to the use of new fluoroquinolones in UTIs.
There was only a slight use of single-dose fosfomycin trometamol, which is recommended as a first-line treatment for cystitis. This is not surprising, as our starting point was urinalyses. Indeed, this molecule is used mainly for the first episode of cystitis, when there is no need for a urinalysis. Thus, the way we selected our patients did not allow us to analyse this type of infection, even though we had many urinalyses performed for cystitis.
The fact that there was a statistical difference in the rate of adapted treatments between cystitis and nephritis, prostatitis or complicated cystitis, but not with recurrent cystitis, indicated that GPs are more anxious and pay more attention to potentially more severe infections than to commonplace cystitis. We did not find other studies that arrived at the same conclusions in the literature.
An incorrect treatment duration has already been described (either too short or too long) in Norway and the United States and, thus, does not seem to be related to French doctors [9, 12]. Following the 2008 guidelines, would have had a favourable impact on bacterial ecology, because of a reduced use of fluoroquinolones, as well as a favourable influence on treatment costs, reducing them dramatically (about 700 € only for cystitis). A similar economic impact has previously been reported when the guidelines were followed. In their study, Kahan et al. found that, in 53 % of treated cases, the cost exceeded that which was expected [11]. As in another study by the same team, we noticed that the treatment length was one of the causes of a higher cost [15]. In France, where health care costs are increasing and which we are attempting to control, following guidelines could be a beginning.
GPs are family practitioners and need treat to treat many different diseases and pathologies. It is not easy to be aware of all the new data and recommendations. This probably explains these poor results. It has already been reported in a study by Kahan et al. that urologists adhere more closely to guidelines than GPs [7], probably because they know the disease and its treatment better.
Our study has some limitations. First of all, as previously stated, the majority of community-acquired UTIs (cystitis) are treated without the use of urinalyses but only with clinical examination and urinary sticks. Thus, the use of urinalyses as a starting point leads to the fact that our patient group and diagnoses are probably not representative of the typical population of community-acquired UTI. That said, this method of selection was better than an interview based on an opinion poll, which would not have reflected the reality of prescriptions.
Another point is that treatment comparison with the guidelines was based on the diagnosis established by the GP. However, we had no means to determine if the diagnosis was the correct one. Thus, a treatment considered as not adapted according to the guidelines could be the right one for the GP if the diagnosis was wrong. For example, temperature is often not considered as a sign of nephritis or prostatitis and misleads to a diagnosis of cystitis. This mistake is even found in men for whom cystitis is considered not to exist and that all UTIs must be considered as prostatitis. Therefore, the prescription of furans is incorrect, not because of the lack of compliance to the guidelines but because the diagnosis was wrong. However, wrong diagnosis seems to occur in up to 33 % using only clinical data [16].
Another French study in 2007 (de Saint Aubin, unpublished data) reported that the diagnosis was more often incorrect rather than the prescription [17]. Indeed, clinical signs of a more severe disease (such as temperature) tend to be underestimated. However, the guidelines at this time were more approximative than those published in 2008. In our study, the widespread prescription of fluoroquinolones in contrast to a large amount of cystitis suggests more treatment error rather than an incorrect diagnosis.
Conclusion
Our study evaluates the actual antibiotic prescription for urinary tract infections (UTIs) by general practitioners (GPs) 2 years after the publication of new guidelines which recommended reducing fluoroquinolones use. Our results show that these guidelines are, for the moment, not followed sufficiently and that there is still a majority of UTIs treated with fluoroquinolones. The prescriptions still adhere to the previous and out-of-date recommendations. Moreover, it is difficult to change habits when, individually, they give good results. Indeed, without complications, UTI treatment is usually effective, whatever it is. So it is easy to understand why GPs do not change their prescription, moreover if they are unaware of their role in the development of resistant bacteria. However, prescription modification is proposed in other countries such as South Africa as a consequence of changing resistance patterns [18]. It also seems that part of these poor practices result not only from poor awareness of the guidelines but from misdiagnoses. Our study highlights the necessity to better publicise these guidelines and to increase Continuing Medical Education (CME) for both diagnosis and treatment.
References
Masiero G, Filippini M, Ferech M, Goossens H (2010) Socioeconomic determinants of outpatient antibiotic use in Europe. Int J Public Health 55(5):469–478
van de Sande-Bruinsma N, Grundmann H, Verloo D, Tiemersma E, Monen J, Goossens H, Ferech M; European Antimicrobial Resistance Surveillance System Group; European Surveillance of Antimicrobial Consumption Project Group (2008) Antimicrobial drug use and resistance in Europe. Emerging Infect Dis 14(11):1722–1730
Mérens A, Servonnet A (2010) Mechanisms and epidemiology of fluoroquinolone resistance in 2010. Rev Francoph Lab 422:33–41
European centre for Disease Prevention and Control (ECDC) (2012) Susceptibility of Enterococcus faecalis isolates to aminopenicillins in participating countries in 2010. Available online at: http://www.ecdc.europa.eu/en/activities/surveillance/EARS-Net/database/Pages/table_reports.aspx. Accessed 5 Feb 2012
AFSSAPS (Agence française de sécurité sanitaire des produits de santé) (2008) AFSSAPS Practice recommendations for diagnosis and antibiotic therapy of adult community urinary tract infections. Méd Mal Infect 38(Suppl 3):S203–S252
Llor C, Rabanaque G, López A, Cots JM (2011) The adherence of GPs to guidelines for the diagnosis and treatment of lower urinary tract infections in women is poor. Fam Pract 28(3):294–299
Kahan NR, Friedman NL, Lomnicky Y, Hemo B, Heymann AD, Shapiro M, Kokia E (2005) Physician speciality and adherence to guidelines for the treatment of unsubstantiated uncomplicated urinary tract infection among women. Pharmacoepidemiol Drug Saf 14(5):357–361
Taur Y, Smith MA (2007) Adherence to the Infectious Diseases Society of America guidelines in the treatment of uncomplicated urinary tract infection. Clin Infect Dis 44(6):769–774
McEwen LN, Farjo R, Foxman B (2003) Antibiotic prescribing for cystitis: how well does it match published guidelines? Ann Epidemiol 13(6):479–483
Grover ML, Bracamonte JD, Kanodia AK, Bryan MJ, Donahue SP, Warner AM, Edwards FD, Weaver AL (2007) Assessing adherence to evidence-based guidelines for the diagnosis and management of uncomplicated urinary tract infection. Mayo Clin Proc 82(2):181–185
Kahan NR, Kahan E, Waitman D-A, Chinitz DP (2004) Economic evaluation of an updated guideline for the empiric treatment of uncomplicated urinary tract infection in women. Isr Med Assoc J 6(10):588–591
Agdestein B, Lindbæk M, Gjelstad S (2011) Do general practitioners follow the national guidelines for treating urinary tract infections with antibiotics? Tidsskr Nor Laegeforen 131(17):1641–1644
Stein GE, Schooley S (2004) Urinary concentrations and bactericidal activities of newer fluoroquinolones in healthy volunteers. Int J Antimicrob Agents 24(2):168–172
Bush LM, Chaparro-Rojas F, Okeh V, Etienne J (2011) Cumulative clinical experience from over a decade of use of levofloxacin in urinary tract infections: critical appraisal and role in therapy. Infect Drug Resist 4:177–189
Kahan NR, Chinitz DP, Kahan E (2004) Longer than recommended empiric antibiotic treatment of urinary tract infection in women: an avoidable waste of money. J Clin Pharm Ther 29(1):59–63
Schmiemann G, Kniehl E, Gebhardt K, Matejczyk MM, Hummers-Pradier E (2010) The diagnosis of urinary tract infection: a systematic review. Dtsch Arztebl Int 107(21):361–367
de Saint Aubin H (2008) Prise en charge des infections urinaires en médecine générale: état des connaissances et étude de pratique par entretiens confraternels auprès de 57 médecins généralistes de Haute-Normandie
Bosch FJ, van Vuuren C, Joubert G (2011) Antimicrobial resistance patterns in outpatient urinary tract infections—the constant need to revise prescribing habits. S Afr Med J 101(5):328–331
Conflict of interest
There is no conflict of interest.
Financial disclosure
No financial support was received for the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Denes, E., Prouzergue, J., Ducroix-Roubertou, S. et al. Antibiotic prescription by general practitioners for urinary tract infections in outpatients. Eur J Clin Microbiol Infect Dis 31, 3079–3083 (2012). https://doi.org/10.1007/s10096-012-1668-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-012-1668-9