Abstract
General practitioners often have to manage urinary tract infections (UTI) with probabilistic treatments, although bacterial resistances are increasing. Therefore, the French Society of Infectious Diseases published new guidelines in 2014. The aim of this study was to investigate the bacterial epidemiology of UTI in the general population in primary care and analyse risk factors for Escherichia coli resistance to antibiotics. A cross-sectional study was conducted in 12 ambulatory laboratories. Patients over 18 years of age coming for urinalysis were included. Risk factors for UTI were collected using a questionnaire and the laboratory records. Bacteria meeting criteria for UTI were analysed. A positive urinalysis was found in 1119 patients, corresponding to 1125 bacterial isolates. The bacterial species were: E. coli (73 %), Enterococcus spp. (7 %), Klebsiella spp. (6 %), Proteus spp. (4 %), Staphylococcus spp. (3 %) and Pseudomonas spp. (2 %). Regardless of the bacteria, the most common resistance was that to co-trimoxazole: 27 % (95 % confidence interval [CI] = [0.24; 0.30]), followed by ofloxacin resistance: 16 % [0.14; 0.18]. Escherichia coli resistances to co-trimoxazole, ofloxacin, cefixime, nitrofurantoin and fosfomycin were, respectively, 25.5 % [0.23; 0.28], 17 % [0.14; 0.20], 5.6 % [0.04; 0.07], 2.2 % [0.01; 0.03] and 1.2 % [0.005; 0.02]. Independent risk factors for E. coli resistance to ofloxacin were age over 85 years (odds ratio [OR] = 3.08; [1.61; 5.87]) and a history of UTI in the last 6 months (OR = 2.34; [1.54; 3.52]). Our findings support the guidelines recommending fluoroquinolone sparing. The scarcity of E. coli resistance to fosfomycin justifies its use as a first-line treatment in acute cystitis. These results should be reassessed in a few years to identify changes in the bacterial epidemiology of UTI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the United Kingdom, during the 1991–2012 period, bacterial resistance has led to a 12 % increase in antibiotic monotherapy failure in primary care, but urinary tract infections (UTI) have not been studied [1]. The ARESC France study on cystitis conducted in primary care has found that 83.8 % of resistances were related to Escherichia coli, 4.3 % to Staphylococcus saprophyticus, 3.1 % to Proteus mirabilis, 1.2 % to Enterococcus spp. and 1 % to Klebsiella pneumoniae [2]. According to the National Observatory of Epidemiology of Bacterial Resistance to Antibiotics (ONERBA), between 2007 and 2009, E. coli sensitivity to antibiotics has remained stable or slightly decreased with, respectively, a sensitivity of 56 % versus 57 % to ampicillin, 98 % versus 96 % to third-generation cephalosporin (3GC), 90 % versus 84.8 % to ciprofloxacin, 80 % versus 76.1 % to co-trimoxazole, 96 % versus 95.2 % to nitrofurantoin and 99 % versus 99.3 % to fosfomycin. Extended-spectrum beta-lactamase (ESBL) bacteria have doubled over this period [3]. Factors associated with increased bacterial resistances were age over 50 years, the presence of complicated UTI, the use of antibiotics in the past 3 months before the onset of UTI [4] and the use of quinolones in the last 6 months [5]. Fluoroquinolones, co-trimoxazole and beta-lactams are frequently involved in the increase in bacterial resistances [6–8].
Since an improved use of antibiotics could reduce the development of bacterial resistance in UTI [9], the new 2014 Société de Pathologie Infectieuse de Langue Française (SPILF) guidelines recommend quinolone sparing. The aim of this study was to investigate the bacterial species and resistances in UTI and to identify risks factors for bacterial resistance in primary care, especially those related to E. coli.
Methods
A cross-sectional study was conducted in patients from 12 ambulatory medical laboratories in the Parisian area. Patients aged over 18 years who came to the laboratories for urinalysis were included consecutively between April and July 2014. They received an information sheet and a consent form. Those who did not meet UTI criteria were excluded. Data on patient sex, age, past or present antibiotic treatments, history of UTI and hospitalisations in the last 6 months were collected using a questionnaire and the laboratory records.
UTI was confirmed if the urinalysis showed pyuria (>104 white blood cells/ml) with bacteriuria >103 colony-forming units (CFU)/ml for Enterobacteriaceae and S. saprophyticus, >104 CFU/ml for the other bacteria in women and >103 CFU/ml in men, according to the current guidelines [5]. The urinalysis results were given by an automated urinalysis device (Vitek 2).
As the estimated resistance to ofloxacin and prevalence of E. coli are, respectively, 15 % [3] and 80 % [2], 980 positive urinalyses were needed in order to achieve an accuracy of 2.5 %. Statistical analyses were performed using bilateral tests with α equal to 5 %. Univariate analyses were performed using a simple logistical regression. Multiple logistical regressions including factors with p < 0.2 in the univariate analyses were used for multivariate analyses. Data collection and statistical analyses were performed using the R software (http://cran.r-project.org/). This study did not receive any funding.
Results
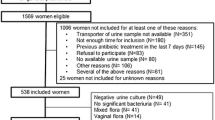
A total of 6133 urinalyses were screened and 1410 were excluded because they involved children, 3602 because they did not meet criteria for UTI and two because they were positive for Candida spp. Finally, 1,119 urinalyses were included (Fig. 1). Only 21 % of subjects with UTI returned the questionnaire. The mean patient age was 59.1 years (±21), and 16.4 % of patients were men (Table 1).
Among the 1119 patients, six were infected by two bacteria and 1125 bacterial isolates were studied. Escherichia coli were the most common bacteria, with a frequency of 73 % (95 % confidence interval [CI] = [0.70; 0.76]), followed by Enterococcus spp., with a frequency of 6.6 % [0.05; 0.08], and Klebsiella spp., with a frequency of 5.6 % [0.04; 0.07]. Then, less common bacteria with, respective, frequencies were: Proteus spp. with 3.5 % [0.02; 0.05], Staphylococcus spp. with 2.8 % [0.02; 0.04], Streptococcus B with 1.9 % [0.01; 0.03] and Pseudomonas spp. with 1.6 % [0.01; 0.02]. Finally, some Enterobacteriaceae (Citrobacter spp., Enterobacter spp., Providencia rettgeri, Serratia fonticola and Shigella) were related to 4.5 % of UTI.
Regardless of the bacteria, the most common resistance was that to co-trimoxazole, found in 27 % [0.24; 0.30] of bacteria, followed by ofloxacin resistance in 16 % [0.14; 0.18] of bacteria.
Resistance to co-trimoxazole, ofloxacin, cefixime, nitrofurantoin and fosfomycin was respectively found in 25.5 % [0.23; 0.28], 17 % [0.14; 0.20], 5.6 % [0.04; 0.07], 2.2 % [0.01; 0.03] and 1.2 % [0.005; 0.02] of E. coli (Table 2).
Nineteen bacterial isolates (1.7 %) were positive for ESBL, corresponding to E. coli in 18 patients and Klebsiella spp. in one. These patients were aged between 18 and 94 years (mean age 67 ± 19.3 years). Among them, 84 % were women, 21 % had diabetes mellitus and 63 % had a history of UTI in the last 6 months. Only one reported having been hospitalised recently.
A history of UTI in the last 6 months (p < 0.001) and age (p = 0.006) were related to bacterial resistance in the multivariate analyses. A history of UTI increased this risk by 2.34 [1.54–3.53] and age over 85 years by 3.09 [1.61–5.87]. Male gender, diabetes mellitus and medical laboratories were not significantly related to E. coli resistance (respectively: p = 0.12, p = 0.54 and p = 0.91) (Table 3).
Discussion
This study showed that E. coli were still the most common bacteria found in ambulatory UTI. In addition, 17 % were resistant to fluoroquinolones and 24 % to co-trimoxazole. This study confirmed that a history of UTI was one of the main independent risk factors for bacterial resistance and found that only age over 85 years increased this risk.
All patients were included consecutively from laboratories located in ten cities to obtain results more representative of the general population. Children were excluded for ethics reasons and difficulties in obtaining consent from these patients, because there is no consensual value to diagnose UTI in children using only urinalysis unlike in adults, and also because pathologies may be different depending on the child age, as many urinary tract diseases could be unknown at the time of urinalysis and be confounders.
Despite the large sample included, only a few questionnaires were returned. This could be due to the fact that it could contain too many questions, as it was also used for ancillary studies assessing urinalysis and antibiotic prescriptions. Moreover, patients could complete it at home, but the secretaries sometimes did not have time to provide enough explanation that could have improved its completion.
A 6-month time frame was chosen because it is the most common duration used for questioning about the last use of antibiotics, last UTI and hospitalisation [10, 11]. Oral ofloxacin was studied because it is used twice as much as ciprofloxacin in primary care [12]. Bacterial resistance to amoxicillin and ampicillin was not studied because these antibiotics are not recommended as probabilistic treatments.
Our results supported those found in other works in this field. In 1997 and 1999, Goldstein [13] and Quentin et al. [14] found that the most common species identified in UTI in medical laboratories were E. coli (75 % and 85 %), Proteus spp. (6 % and 7 %), Klebsiella spp. and Enterococcus spp. (less than 5 %). The ARESC France trial has studied cystitis and found that E. coli had the highest prevalence (84 %), followed by S. saprophyticus and P. mirabilis [2], which are involved more in cystitis than in pyelonephritis [15, 16].
The change in E. coli resistances may be seen in Table 4, where six ambulatory studies are presented [2, 13, 14, 17, 18]. There was no obvious increase in resistances because all the studies did not use the same antibiotics, especially for fluoroquinolones. Resistance to fluoroquinolones varied between 2 % in the ARESC study and 17 % in our study, and resistance to co-trimoxazole between 12 % and 24 %. The number of ESBL bacteria seemed to increase slightly, from 0.4 % in 1997 to 1.7 % in 2014. Finally, resistances to nitrofurantoin and fosfomycin remained stable, at under 5 %.
It should be noted that fosfomycin was associated with a resistance of less than 1 % in E. coli, which confirmed its place as a first-line treatment in acute cystitis. In the coming years, it would be interesting to study the effect of the new guidelines on bacterial species and resistances in UTI and to investigate whether fluoroquinolone sparing has induced a decrease in bacterial resistance.
References
Currie CJ, Berni E, Jenkins-Jones S, Poole CD, Ouwens M, Driessen S et al (2014) Antibiotic treatment failure in four common infections in UK primary care 1991–2012: longitudinal analysis. BMJ 349:g5493
Neuzillet Y, Naber KG, Schito G, Gualco L, Botto H (2012) French results of the ARESC Study: clinical aspects and epidemiology of antimicrobial resistance in female patients with cystitis. Implications for empiric therapy. Méd Mal Infect 42(2):66–75
Vachée A; ONERBA France (2010) Évolution de la résistance aux antibiotiques au sein de l’espèce E. coli. Journées Nationales d’Infectiologie, Session ONERBA
Alós J-I, Serrano M-G, Gómez-Garcés J-L, Perianes J (2005) Antibiotic resistance of Escherichia coli from community-acquired urinary tract infections in relation to demographic and clinical data. Clin Microbiol Infect 11(3):199–203
Société de Pathologie Infectieuse de Langue Française (SPILF) (2014) Diagnostic et antibiothérapie des infections urinaires bactériennes communautaires de l’adulte
Wright SW, Wrenn KD, Haynes M, Haas DW (2000) Prevalence and risk factors for multidrug resistant uropathogens in ED patients. Am J Emerg Med 18(2):143–146
Shilo S, Assous MV, Lachish T, Kopuit P, Bdolah-Abram T, Yinnon AM et al (2013) Risk factors for bacteriuria with carbapenem-resistant Klebsiella pneumoniae and its impact on mortality: a case–control study. Infection 41(2):503–509
Hayakawa K, Gattu S, Marchaim D, Bhargava A, Palla M, Alshabani K et al (2013) Epidemiology and risk factors for isolation of Escherichia coli producing CTX-M-type extended-spectrum β-lactamase in a large U.S. Medical Center. Antimicrob Agents Chemother 57(8):4010–4018
Butler CC, Dunstan F, Heginbothom M, Mason B, Roberts Z, Hillier S et al (2007) Containing antibiotic resistance: decreased antibiotic-resistant coliform urinary tract infections with reduction in antibiotic prescribing by general practices. Br J Gen Pract 57(543):785–792
van der Starre WE, van Nieuwkoop C, Paltansing S, van’t Wout JW, Groeneveld GH, Becker MJ et al (2011) Risk factors for fluoroquinolone-resistant Escherichia coli in adults with community-onset febrile urinary tract infection. J Antimicrob Chemother 66(3):650–656
Société de Pathologie Infectieuse de Langue Française (SPILF) (2014) Facteurs de risque de résistance aux fluoroquinolones. Annexe des recommandations sur la prise en charge des infections urinaires communautaires
Réseau ATB Raisin (2012) Surveillance de la consommation des antibiotiques. Résultats 2010. Institut de veille sanitaire (InVS)
Goldstein FW (2000) Antibiotic susceptibility of bacterial strains isolated from patients with community-acquired urinary tract infections in France. Multicentre Study Group. Eur J Clin Microbiol Infect Dis 19(2):112–117
Quentin C, Arpin C, Dubois V, André C, Lagrange I, Fischer I et al (2004) Antibiotic resistance rates and phenotypes among isolates of Enterobacteriaceae in French extra-hospital practice. Eur J Clin Microbiol Infect Dis 23(3):185–193
Johnson JR, Stamm WE (1989) Urinary tract infections in women: diagnosis and treatment. Ann Intern Med 111(11):906–917
(2014) Cystites aiguës simples chez les femmes. L’essentiel sur les soins de premier choix. Rev Prescrire 34(369):528–530
Fabre R, Mérens A, Lefebvre F, Epifanoff G, Cerutti F, Pupin H et al (2010) Sensibilité aux antibiotiques des Escherichia coli isolés d’infections urinaires communautaires. Méd Mal Infect 40(10):555–559
Rossignol L, Maugat S, Blake A, Barlier R, Vaux S, Heym B et al (2014) Étude Druti: Epidémiologie et prise en charge des infections urinaires en médecine générale en France métropolitaine. Institut de veille sanitaire (InVS)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Malmartel, A., Ghasarossian, C. Epidemiology of urinary tract infections, bacterial species and resistances in primary care in France. Eur J Clin Microbiol Infect Dis 35, 447–451 (2016). https://doi.org/10.1007/s10096-015-2560-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-015-2560-1