Abstract
The aim of this study was to delineate the potential risks and dynamics of the prolonged carriage of resistant E. coli in returned travellers. A sample of 274 previously collected E. coli resistant to ceftriaxone (CRO), ciprofloxacin, gentamicin and/or nalidixic acid recovered from 102 travellers was studied. Travellers were assessed pre-travel then longitudinally (maximum 6 months) with peri-rectal/rectal swabs. Clonality was determined by REP-PCR and the presence of O25b-ST131 was assessed. Comparison was made longitudinally for individuals and between identified co-travellers. The risk of prolonged carriage was lower for CRO than for ciprofloxacin or gentamicin resistance. Repeated isolation of the same phenotype at different time points occurred in 19% of initial CRO-resistant carriers compared with 50% of ciprofloxacin- or gentamicin-resistant carriers. The duration of carriage was also longer for the latter resistance phenotypes (75th quartile 8 vs 62 and 63 days respectively). In multivariate analysis, risks of prolonged carriage included antimicrobial use whilst travelling (3.3, 1.3–8.4) and phylogenetic group B2 (9.3, 3.4–25.6) and D (3.8, 1.6–8.8). Clonality amongst longitudinal isolates from the same participant was demonstrated in 92% of participants who were assessable and most marked amongst CRO-resistant isolates. ST-131 was surprisingly infrequent (3% of participants). Prolonged carriage of ciprofloxacin- and gentamicin-resistant isolates is more frequent and prolonged than CRO resistance after travel. Risks of prolonged carriage indicate a contribution of host and bacterial factors to this carriage. These require further elucidation. The strong clonality identified suggests that carriage of a “phenotype” was mediated by persistence of bacteria/plasmid combinations rather than persistence of the plasmid after horizontal transfer to other bacteria.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
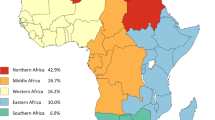
A number of recent publications have identified carriage of multi-resistant Enterobacteriaceae, primarily E. coli, in the gastrointestinal flora of returned travellers [1–5]. Individuals harbouring antibiotic-resistant organisms have frequently travelled from countries of low resistance incidence to countries of high incidence, e.g., Northern Europe to India. Key geographical regions for acquisition of multi-resistant Enterobacteriaceae include South-East Asia, the Indian Sub-continent and Africa.
One limitation of the current studies is that they provide only a “snapshot” of a narrow resistome immediately after travel, with only two studies thus far providing any longitudinal data [2, 4]. Such data help us to better understand the link between carriage of resistant Enterobacteriaceae in travellers and subsequent infection in the carrier (or others within the community). Factors impacting on this link may include the risk of acquisition whilst travelling, clonal dynamics and duration of carriage, risk factors for prolonged carriage and the potential for spread of resistance by carriers within the home community or healthcare setting.
Even from the perspective of the more frequently described health-care-associated carriage of resistant Enterobacteriaceae, longitudinal carriage studies are limited and varied. Median durations of carriage of E. coli range from 80 to 178 days with single and multiple clones identified in differing settings [6–11]. Furthermore, the dynamics of healthcare-associated carriage may vary considerably from that of travellers, given the differing mechanism of acquisition and population involved. Complicating our understanding of prolonged carriage of antibiotic-resistant Enterobacteriaceae is the potential that any given resistance phenotype may be mediated by persistence of a stable bacteria/plasmid combination or persistence of the plasmid after horizontal transfer to other bacteria [12].
In this study we aimed to define longitudinal and clonal aspects of the prolonged carriage of antimicrobial resistance in a cohort of returned travellers. The natural history and clonality of individual carriers was investigated using a sample of patients selected as being unlikely to have acquired new resistance after return from travel, by virtue of residence in an area of low background incidence of resistance and absence of antimicrobial exposure or re-travel [4, 13]. Shared clonality between travel partners and the incidence of the ST-131 O25B worldwide pandemic clone were explored in the entire cohort, comprising all samples collected during the study.
Materials and methods
Bacterial isolates and data collection
Bacterial isolates used for this study consisted of 274 Escherichia coli from 102 participants collected during a previous prospective study of returned travellers residing in Canberra, Australia [4]. The original study investigated the rate and duration of colonisation with resistant E. coli following international travel. Isolates presented were resistant to ciprofloxacin (cip-R), gentamicin (gent-R) and/or ceftriaxone (CRO-R). In addition, nalidixic acid-resistant E. coli also recovered from this cohort were included in this analysis. A full description of the methods of bacterial isolation and clinical data collection is contained in the original publication [4]. In brief, 102 prospectively enrolled travellers who completed the study were asked to collect rectal or perianal swabs within 14 days before an overseas trip and within 14 days after return to Australia. If isolates resistant to ciprofloxacin, gentamicin or ceftriaxone were detected on the first return swab, participants were asked to collect regular monthly swabs until resistant bacteria were not identified on two sequential swabs or for a maximum of 6 months. Swabs were subcultured on three media, HBA-gentamicin (Oxoid, Adelaide, SA, Australia), MacConkey agar (Oxoid) containing a nalidixic acid disc (Oxoid, Basingstoke, Hampshire, UK) and chromID (ESBL; bioMérieux, Craponne, France), after initial overnight broth enrichment. Resistant colonies were selected from each plate and underwent identification and susceptibility testing using Vitek2 (bioMérieux, Durham, NC, USA). If all colonies on a given plate appeared morphologically identical, then only a single colony was sampled. If morphological differences between colonies were apparent, each variant was sampled. Mechanisms of ceftriaxone resistance were confirmed by PCR and sequencing and are presented in the original study. They comprised ESBL and AmpC enzymes [4].
All participant and travel data used in this study were collected via a questionnaire completed directly by participants during the original study. Variables included travel destinations, antimicrobial use, intercurrent illness and food/water consumption whilst travelling. For this analysis “high risk” regions were defined as regions where >50% of travellers during the original study returned with a resistant isolate. As travellers frequently visited more than one destination, the duration of stay in each region was calculated and included.
Molecular methods
The phylogenetic group was determined on all isolates using triplex PCR [14]. Determination of the ST-131 O25B worldwide pandemic clone was undertaken by detection of pabB and trpA alleles via multiplex PCR with a positive control MLST, confirmed as ST-131 [15]. Repetitive extragenic palindromic PCR (REP-PCR) was undertaken using published methods [16]. The template was purified DNA (Mo-Bio, USA), using a BioRad C1000 Thermal Cycler. Primers REP-1 (5’-IIIGCGCCGICATCAGGC-3’) and REP-2 (5’-ACGTCTTATCAGGCCTAC-3’) were used. The products were separated on a 1% agarose gel (45 v, 3 h) and stained with ethidium bromide. Manual visual comparison was used to identify clonal isolates and any difference greater than two non-shared bands was considered non-clonal. Bacteria for comparison were always separated on the same agarose gel.
All isolates of the same phylogenetic group harboured by the same participant or shared by travel partners were considered potentially clonal. For CRO-R isolates, all potentially clonal isolates were subject to REP-PCR. For cip-R and gent-R isolates, if three or more potentially clonal isolates of the identical phylogenetic group and phenotypic antimicrobial susceptibility (amoxicillin, amoxicillin/clavulanate, cephazolin, ceftriaxone, ciprofloxacin, gentamicin, trimethoprim/sulfamethoxazole) occurred within 8 weeks, interval isolates were skipped (e.g. sample 2 of samples 1, 2 and 3 skipped). If differing presumptive clonality was identified amongst the isolates analysed then the interval isolate was subject to REP-PCR.
Definitions
Duration of carriage was calculated from the date of return to Australia until the date of collection of the last positive swab. Clearance of carriage was assumed if there was collection of at least one swab not containing the given antimicrobial resistance phenotype, without the occurrence of any subsequent positive swabs. Clonal carriage was defined as identification of clonal isolates (as defined by REP-PCR) at two time points (most > 4 weeks apart). As above, any isolates with more than two non-shared bands were considered unrelated.
Censoring and exclusions for longitudinal analysis
Participant results were censored (exclusion of all subsequent swab results) after events that may have potentiated new acquisition of resistance including further overseas travel or receipt of antimicrobial therapy for suspected or proven infection (n = 6 urinary tract infection, n = 2 other infection site). Participants who were still on doxycycline for malaria prophylaxis at the time of the return swab were not excluded. Participants harbouring clonally related isolates pre- and post-travel were excluded. To assess this, all pre-travel isolates were compared with post-travel isolates using REP-PCR in a similar manner to the longitudinal analysis (n = 7 participants). All participants remaining who had assessable swabs collected at two or more time points after travel were included.
Statistical methods
Kaplan–Meier plots were used to illustrate duration of resistance. Subjects were censored if they remained resistant at their final data collection time-point. Parametric survival models were used to estimate the magnitude of differences in the distribution of resistance duration due to the three antibiotics. More specifically, log normal accelerated failure time models were used, as the log normal provided the best fit to the observed data from a number of common alternatives (including Weibull and log-logistic models) and estimates from accelerated failure time models could be reported as proportional increases in resistance duration. Robust variances were used to take into account within-patient correlations of resistance to the three antibiotics of interest.
Potential risk factors were assessed for possible association with duration of resistance to any of the three antibiotics by including these variables as covariates in univariate survival models. All variables that showed some evidence of association in univariate analysis (p < 0.1) were included in multivariate analysis. Backwards elimination was used to remove non-significant (p > 0.1) variables until the best predictive model was obtained. SAS version 9.1 for Windows and Stata/IC 10.1 for Windows were used for analysis.
Results
Duration, clonal dynamics and risks of prolonged carriage
Of the 102 original participants in the study, 50 returned carrying antimicrobial-resistant E. coli of interest (CRO-R, cip-R and/or gent-R), with 44 included in the final analysis after censoring and exclusions (Fig. 1). Three participants reporting ongoing use of doxycycline for malaria prophylaxis at the initial return swab were not excluded.
Duration and risks of prolonged carriage of resistance
Upon initial assessment, after return from travel, the carriage of the three specified phenotypes was CRO-R 26% (n = 27), cip-R 27% (n = 28), gent-R 35% (n = 36). When compared with CRO resistance, cip-R and gent-R were associated with 2.1 (95% CI, 1.1 to 4.1, p = 0.027) and 3.5 (95% CI, 1.6 to 7.5, p = 0.001) times the duration of carriage of resistance respectively. There was no significant difference between the duration of cip-R and gent-R. The median durations and inter-quartile range for recovery of resistance from travellers was 3 (IQR, 1 to 8) days for CRO-R, 5 (IQR, 1 to 62) days for cip-R and 8 (IQR, 3 to 63) days for gent-R. This is represented longitudinally on a Kaplan–Meier curve (Fig. 2), demonstrating that the major difference is in the upper quartile of participants.
Potential risks for prolonged carriage of any resistance were analysed by three groups of factors: participant/travel characteristics, duration/location of travel and bacterial factors. Results of the univariate and multivariate survival model are presented in Tables 1 and 2.
Clonal dynamics of resistance
Clonality was almost always present in prolonged carriage of a given antimicrobial phenotype. Of 25 participants with isolation of bacteria of the same phenotype at two time points, the carriage of exclusively clonal isolates was demonstrated in 14 participants (56%). Carriage of a mixture of clonal and non-clonal isolates occurred in 9 (36%). Three participants (12%) carried more than one prolonged clone simultaneously. In only 2 (8%) was no clonal relationship found between the bacteria isolated. In both cases bacteria were only recovered on the return swab and a single subsequent swab. These patterns are illustrated in Fig. 3.
Travellers representative of different patterns of carriage of resistant isolates. A time-line is displayed across the top (days). Arrows represent the submission of swabs by travellers. Shaded squares indicate bacterial clones with the diamond in each square showing time points at which the bacteria were isolated in a sample
The dynamics of clonality differed between CRO-R and cip-R or gent-R isolates. With the exception of a single bacterial isolate, repeated isolation of CRO-R E. coli was invariably due to the presence of clonal bacteria. The carriage of ciprofloxacin and gentamicin resistance demonstrated more diversity, although by month 5 all the isolates recovered were clonal with earlier isolates (Fig. 4).
Graphical representation of the clonality of isolates amongst each individual. Left Comparison of CRO-resistant isolates with other CRO-resistant isolates amongst the same individual. Right Comparison of ciprofloxacin- and/or gentamicin-resistant isolates with other isolates of the same phenotype amongst the same individual. (Isolates harbouring CRO resistance have been excluded.) (Phenotypes that were only recovered at a single time point could not be assessed for clonality and are indicated in white/hash)
Travel partners
From the cohort of 102 travellers, 70 (68%) travelled with other study members (Fig. 1). This included 29 “pairs” (travel and sexual partners) and six “mixed groups” containing participants of other relationships (friends travelling together, families and one unknown relationship). For analysis, pairs within mixed groups were considered, within the “pairs” cohort.
Analysis of the 29 “pairs” revealed 14 with neither returning with resistance (48%), 8 (28%) with a single partner and 9 (31%) with both partners harbouring resistance. Thus, if one person was colonised, there was a 53% chance of the partner also harbouring one of the three resistant phenotypes sought (9 out of 17). However, using clonal analysis, just 2 of the 9 couples (22%) shared clones.
Shared clonality was also identified amongst one in six “mixed” groups of travellers.
ST-131 worldwide pandemic clone
The presence of the clone was assessed amongst all 274 E. coli isolates recovered from 102 participants. This included all CRO-R, gent-R, cip-R and/or nalidixic acid-resistant isolates recovered from participants throughout the study duration (Fig. 1). Pre-travel prevalence of the clone was 2% (2 out of 102). An additional two individuals acquired ST-131 E. coli while travelling. With the exclusion of the pre-travel carriers, only one prolonged clonal carrier was colonised with an ST-131 strain. All ST-131 E. coli isolated were phylogenetic group B2.
Discussion
Carriage of multi-resistant Enterobacteriaceae upon return from travel is a real and concerning phenomenon. The most serious outcome of such carriage is infection with resistant organisms after return home. Although we did not specifically assess infections in returned travellers, two recent studies have demonstrated this risk in diverse populations. Overseas travel afforded a relative risk of 2.7 for any infection after TRUS biopsy [17], and a relative risk of 5.7 for ESBL E. coli infection in a regional Canadian study [18]. Our analysis helps to delineate the complex link between acquisition and carriage during travel and infection after return.
The rapid decline in carriage of resistant isolates after travel is to some extent encouraging; however, persistence is significant. Analysis of the longitudinal nature of carriage highlights the marked persistence of cip-R and gent-R isolates beyond CRO resistance, with 10% of participants in the longitudinal arm of this study harbouring cip-R and/or gen-R at 6 months after return. This is noteworthy, given that fluoroquinolones and aminoglycosides are heavily relied upon for the treatment of E. coli infection, including urinary sepsis, in many national guidelines [19, 20]. The prolonged duration of carriage of fluoroquinolones resistance identified concurs with descriptions of healthcare-associated carriage [6, 7, 10]. Explanations for the shorter duration of CRO resistance potentially include the higher fitness cost for bacterium of maintaining this resistance plasmid in the absence of ongoing selection pressure and genetic differences between the host bacteria that harbour each resistance element.
Risk factors for prolonged carriage are intriguing. Antimicrobial use whilst travelling was strongly associated, leading to a 3.4 times increase in duration of carriage. Kennedy, in travellers [4], and many authors in other settings have identified antimicrobial use as a risk factor for the acquisition of resistance, an intuitive conclusion. However, this study examines a group who all harboured resistance and did not have further antimicrobial exposure to potentiate this risk. Another mechanism apart from simple selection of antimicrobial resistance may apply. We hypothesise potential modification of intestinal microbiota after antimicrobial use, leading to the loss of other potentially competitive non-resistant E. coli and other integral commensal bacteria [21].
The analysis of clonality answers interesting questions about the acquisition and carriage of such resistance. Whilst the “mobility” of resistance elements, particularly CRO resistance plasmids, was initially hypothesised in this study and is frequently discussed and demonstrated in “high stress” situations such as healthcare settings and antimicrobial use [12], it appears not to be significant in travellers. In fact, clonality was almost absolute for plasmid-mediated CRO resistance. The strong clonality of isolates amongst all phenotypes gives us an insight into the environment of acquisition. The identification of clonality amongst travel partners and mixed groups (where direct transmission from person to person was unlikely) suggests exposure and ingestion of a common source of resistant isolates, potentially food or water. This is also supported by the relatively low rate (22%) of shared clonality between partners. The pattern of contraction of a variety of resistant isolates on return to persistence of a single (or very few) clones implies the presence of only a limited number of clones in circulation able to colonise and persist amongst individuals even in such “environments” with high resistance burden. The shared clonality amongst partners/mixed groups and the correlation with period of exposure in “high-risk” regions supports this hypothesis. This can be compared with the observation of clonality amongst E. coli causing urinary tract infection, where a small handful of adapted clonal groups are thought to cause a significant proportion (10–20%) of all such infections [22]. Although not investigated in this study, other than ST131, further exploration of clonality across travellers and regions would be worthwhile.
The identification of “persistent” clones also highlights the issue of potential infection and both community- and healthcare-related transmission of resistant isolates. It is unknown whether travellers might be the point of introduction of antibiotic-resistant bacteria into a community, rather than imported food, animals or de novo development of resistance via antibiotic use. Importation of antibiotic-resistant bacteria into hospitals has been well documented via individuals who have been treated in hospitals in high-risk areas [23]. With respect to travellers, we speculate that a long duration after return from travel, e.g. 3–6 months, may be the most problematic in a healthcare system, given that these clones have been selected as those best adapted for colonisation and persistence.
The relationship between persistence of colonisation and subsequent infection needs further exploration. The phylogenetic groups, as identified in this study, represent a broad family of bacterial characteristics related to virulence. The markedly increased duration of the more virulent B2 and D groups, compared with commensal E. coli (predominantly groups A and B2) [24], indicates bacterial genetic factors other than the presence of resistance genes that may aid in persistence. Potential mechanisms requiring exploration include biofilm formation, competitive bacterial toxin production, e.g. colicins, and virulence factors including siderophore and fimbriae production mediating competitive advantages in iron capture and adhesion. Furthermore, the relation of factors that determine persistence to those that determine the classical virulence of invasion and infection also requires elucidation.
Limitations of this study include the exploratory nature using a previously collected sample. The collection method of recovering a single isolate from the plate has led to some limitation in determining clonality. To investigate this, a model was constructed using the assumption that clones recovered on a given swab were present, but not identified on all previous swabs because of this methodological issue. This model indicated that approximately one third of clones were not recovered on any given swab, suggesting that with the repeat sampling undertaken, there was a low chance of failing to identify truly persisting clones (data not shown).
In the multivariate analysis, only a limited number of factors were assessed. There may be other significant participant and isolate features that were not included in this analysis. Furthermore, the assumption that resistance was only acquired whilst travelling and did not occur after return is relied heavily upon in the data. We believe this was reasonable given the very low background rates of resistance in Canberra [4, 13]; however, it is likely not absolute. Acquisition of resistant clones after return (or the emergence of “low-level” pre-travel resistant clones owing to antimicrobial use) may have led to over-estimation of the duration of carriage and diversity of clonality. A control group of matched non-travellers from Canberra would have been optimal in assessing this situation.
Conclusion
Prolonged gastrointestinal carriage of resistant bacteria after return from travel is a complex phenomenon. The duration of carriage of CRO resistance was significantly shorter than for ciprofloxacin or gentamicin resistance. Risk factors for prolonged carriage of resistance include antimicrobial use whilst travelling and the duration of travel in “high risk” regions. Clonality was present amongst all phenotypes, but was almost absolute amongst CRO resistance. The contraction to a small number of clones and shared clonality amongst travel partners suggests a limited number of clones adapted to prolonged carriage circulating in regions of acquisition. ST-131, the worldwide pandemic clone, was surprisingly infrequent amongst the phenotypes assessed. The identification of clonality amongst travel partners and mixed groups (where direct transmission from person to person was unlikely) suggests exposure and ingestion of a common source of resistant isolates, potentially food or water.
References
Tham J, Odenholt I, Walder M, Brolund A, Ahl J, Melander E (2010) Extended-spectrum beta-lactamase-producing Escherichia coli in patients with travellers' diarrhoea. Scand J Infect Dis 42(4):275–280
Tangden T, Cars O, Melhus A, Lowdin E (2010) Foreign travel is a major risk factor for colonization with Escherichia coli producing CTX-M-type extended-spectrum beta-lactamases: a prospective study with Swedish volunteers. Antimicrob Agents Chemother 54(9):3564–3568
Dhanji H, Patel R, Wall R, Doumith M, Patel B, Hope R, Livermore DM, Woodford N (2011) Variation in the genetic environments of bla(CTX-M-15) in Escherichia coli from the faeces of travellers returning to the United Kingdom. J Antimicrob Chemother 66(5):1005–1012
Kennedy K, Collignon P (2010) Colonisation with Escherichia coli resistant to “critically important” antibiotics: a high risk for international travellers. Eur J Clin Microbiol Infect Dis 29(12):1501–1506
Peirano G, Laupland KB, Gregson DB, Pitout JD (2011) Colonization of returning travelers with CTX-M-producing Escherichia coli. J Travel Med 18(5):299–303
O'Fallon E, Gautam S, D'Agata EM (2009) Colonization with multidrug-resistant gram-negative bacteria: prolonged duration and frequent cocolonization. Clin Infect Dis 48(10):1375–1381
Lautenbach E, Tolomeo P, Mao X, Fishman NO, Metlay JP, Bilker WB, Nachamkin I (2006) Duration of outpatient fecal colonization due to Escherichia coli isolates with decreased susceptibility to fluoroquinolones: longitudinal study of patients recently discharged from the hospital. Antimicrob Agents Chemother 50(11):3939–3943
Horcajada JP, Vila J, Moreno-Martinez A, Ruiz J, Martinez JA, Sanchez M, Soriano E, Mensa J (2002) Molecular epidemiology and evolution of resistance to quinolones in Escherichia coli after prolonged administration of ciprofloxacin in patients with prostatitis. J Antimicrob Chemother 49(1):55–59
Weintrob AC, Roediger MP, Barber M, Summers A, Fieberg AM, Dunn J, Seldon V, Leach F, Huang XZ, Nikolich MP, Wortmann GW (2010) Natural history of colonization with gram-negative multidrug-resistant organisms among hospitalized patients. Infect Control Hosp Epidemiol 31(4):330–337
Oethinger M, Jellen-Ritter AS, Conrad S, Marre R, Kern WV (1998) Colonization and infection with fluoroquinolone-resistant Escherichia coli among cancer patients: clonal analysis. Infection 26(6):379–384
Stuart RL, Kotsanas D, Webb B, Vandergraaf S, Gillespie EE, Hogg GG, Korman TM (2011) Prevalence of antimicrobial-resistant organisms in residential aged care facilities. Med J Aust 195(9):530–533
Sidjabat HE, Silveira FP, Potoski BA, Abu-Elmagd KM, Adams-Haduch JM, Paterson DL, Doi Y (2009) Interspecies spread of Klebsiella pneumoniae carbapenemase gene in a single patient. Clin Infect Dis 49(11):1736–1738
Kennedy KJ, Roberts JL, Collignon PJ (2008) Escherichia coli bacteraemia in Canberra: incidence and clinical features. Med J Aust 188(4):209–213
Clermont O, Bonacorsi S, Bingen E (2000) Rapid and simple determination of the Escherichia coli phylogenetic group. Appl Environ Microbiol 66(10):4555–4558
Clermont O, Dhanji H, Upton M, Gibreel T, Fox A, Boyd D, Mulvey MR, Nordmann P, Ruppe E, Sarthou JL, Frank T, Vimont S, Arlet G, Branger C, Woodford N, Denamur E (2009) Rapid detection of the O25b-ST131 clone of Escherichia coli encompassing the CTX-M-15-producing strains. J Antimicrob Chemother 64(2):274–277
Rodriguez-Bano J, Navarro MD, Romero L, Martinez-Martinez L, Muniain MA, Perea EJ, Perez-Cano R, Pascual A (2004) Epidemiology and clinical features of infections caused by extended-spectrum beta-lactamase-producing Escherichia coli in nonhospitalized patients. J Clin Microbiol 42(3):1089–1094
Patel U, Dasgupta P, Amoroso P, Challacombe B, Pilcher J, Kirby R (2011) Infection after transrectal ultrasonography-guided prostate biopsy: increased relative risks after recent international travel or antibiotic use. BJU Int doi:10.1111/j.1464-410X.2011.10561.x
Laupland KB, Church DL, Vidakovich J, Mucenski M, Pitout JD (2008) Community-onset extended-spectrum beta-lactamase (ESBL) producing Escherichia coli: importance of international travel. J Infect 57(6):441–448
Gupta K, Hooton TM, Naber KG, Wullt B, Colgan R, Miller LG, Moran GJ, Nicolle LE, Raz R, Schaeffer AJ, Soper DE (2011) International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: a 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis 52(5):e103–e120
Antibiotic Expert Group, Spicer J, Therapeutic Guidelines Limited (2010) Therapeutic guidelines: antibiotic. Therapeutic Guidelines, Melbourne, p xxxiv, 445
Willing BP, Russell SL, Finlay BB (2011) Shifting the balance: antibiotic effects on host-microbiota mutualism. Nat Rev Microbiol 9(4):233–243
Manges AR, Tabor H, Tellis P, Vincent C, Tellier PP (2008) Endemic and epidemic lineages of Escherichia coli that cause urinary tract infections. Emerg Infect Dis 14(10):1575–1583
Rogers BA, Aminzadeh Z, Hayashi Y, Paterson DL (2011) Country-to-country transfer of patients and the risk of multi-resistant bacterial infection. Clin Infect Dis 53(1):49–56
Bailey JK, Pinyon JL, Anantham S, Hall RM (2010) Distribution of human commensal Escherichia coli phylogenetic groups. J Clin Microbiol 48(9):3455–3456
Acknowledgements
Thank you to Prof. Mark Schembri for his review of this manuscript.
Conflict of interests
BR, KK, HS, MJ and DP declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rogers, B.A., Kennedy, K., Sidjabat, H.E. et al. Prolonged carriage of resistant E. coli by returned travellers: clonality, risk factors and bacterial characteristics. Eur J Clin Microbiol Infect Dis 31, 2413–2420 (2012). https://doi.org/10.1007/s10096-012-1584-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-012-1584-z