Abstract
The antifungal properties of 25-azalanosterol was investigated. Compared to normal antifungal reagents, fluoconazole, clotrimazole and voriconazole, it exhibited significant anti-Candida activity (the minimum inhibitory concentration [MIC] ranges were 0.125–8, 0.5–8 and 0.5–32 µg/mL against C. albicans, C. krusei and C. glabrata, respectively), but showed little toxicity to mice liver cells at clinical dosage after 24 h of exposure, with the lowest lactate dehydrogenase and the highest ED50 compared to four other azoles antifungal agents. 25-Azalanosterol inhibited the incorporation of [methyl-3H3] AdoMet into the C-24 of ergosterol in whole cells of C. albicans. Thus, 25-azalanosterol, as an inhibitor of the growth of C. albicans in vitro, may have considerable potential as a new class of anti-Candida agent that lacks toxic side effects in the mammalian host.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The occurrence frequency of human fungal infections have been increasing over the past decade in response to a combination of factors, including advances in invasive surgical techniques which allow for opportunistic pathogen access, immuno-suppression employed in transplantation or resulting from chemotherapy, disease such as acquired immune deficiency syndrome (AIDS), and the frequent use of cytotoxic and/or antibacterial drugs [1]. Candidiasis was caused by Candida species; typically, C. albicans was the predominant causal organism of most candidiasis [2]. Other species, including C. krusei, C. glabrata, C. dubliniensis and C. inconspicua, have been recognised [3].
Until recently, fluoconazole and amphotericin B were the standard therapy for many fungal infections, but a high frequency of renal or hepatic toxicity had limited their use [4]. Although many research groups have carried out intensive research in attempts to develop new antifungal drugs, and some of which have now entered clinical trials, some new candin antifungal agents were also investigated [5]. Moreover, side effects were noted for currently available antimycotics at the therapeutic dosage and reports of fungal pathogens resistant to antifungal agents were increasing in frequency [6]. The success in developing a new drug would depend upon the identification of new antifungal targets that had no mammalian host counterpart, but a broad spectrum of pathogenic fungi [7].
The current treatment of this fungal infection involved chemotherapy with azole antifungal drugs which could inhibit the cytochrome P-450-dependent 14a-demethylation of lanosterol or 24-methylene-24,25-dihydrolanosterol, resulting in a decreased availability of an essential membrane component, such as ergosterol, and a corresponding accumulation of 14a-methylated sterols in cell membranes, which eventually lead to cell growth arrest [8]. We have previously demonstrated a series of sterol substrate analogues which significantly inhibited the growth of Candida species [9]. Here, compared to normal antifungal agents, fluoconazole, clotrimazole, ketoconazole and voriconazole, we describe the effects of a lanosterol derivative, 25-azalanosterol (Fig. 1) on: (i) the growth of Candida species; (ii) activities of Candida sterol C-24 methyltransferase (SMT; E.C. 2.1.1.142); and (iii) mammalian rat liver toxicity. Our results indicated that fungal growth inhibition by low levels of 25-azalanosterol was clearly caused by the inhibition of sterol biosynthesis. Also, 25-azalanosterol had the lowest liver toxicity compared to other antifungal agents. So, 25-azalanosterol may have considerable potential as a novel anti-Candida agent that lacks mammalian host toxicity.
Materials and methods
Materials and reagents
The fungal strains used in this study were C. albicans, C. krusei and C. glabrata, which were clinically isolated from candidiasis patients by the Department of Clinical Laboratory, Shanxi Modern Woman’s Hospital, China. The cells were maintained on slants of Sabouraud’s dextrose agar at 4°C. For culture, the cells were inoculated and grown at 35°C for 18 h in YEPD medium (yeast extract, 10 g/L; peptone, 20 g/L; bidest water, 960 mL, after autoclaving, 20mL of sterile glucose solution was added (50% wt/vol), pH 7.0; Meidi Biochemical Product Co., Wuxi, China) [10]. Late exponential phase cells (18 h) were harvested and washed by centrifugation, and used for the preparation of microsomes.
The antifungal agents, fluoconazole, clotrimazole, ketoconazole and voriconazole, were purchased from Kangning Medicine Co. (Shandong, China). 25-Azalanosterol was synthesised and supported by the Shanxi Chemical Industrial Institute. AdoMet iodide salt was purchased from Sigma and [methyl-3H3] AdoMet (10–15 Ci/mmol) was purchased from PerkinElmer Life Sciences. All other reagents and chemicals were purchased from Sigma Co. Ltd.
BALB mice (Experimental Animal Laboratory, Shanxi Medical University), 70 days old, were divided into five different groups (six mice/group) and were housed singly. The liver from six mice in each group at 70 days were dissected separately and cultivated in RPMI1640 medium. The cells were mechanically dispersed by repeated triturating and filtered through a 200-µm metal mesh. Two-millilitre aliquots of the cell suspension were plated at a final density of 106 cells/mL for cytotoxicity analysis. Hepatic cytotoxicity was evaluated by lactate dehydrogenase (LDH) activity and MTT (3-(4,5-dimethyl-2-thiazolyl)-2,5-diphenyl-2H-tetrazolium bromide) in mice liver homogenates.
Inhibition of growth
Minimum inhibitory concentrations (MICs) to C. albicans (n = 53), C. krusei (n = 13) and C. glabrata (n = 21) were estimated after inoculation in RPMI1640 medium containing various doses of antifungal agents, 25-azalanosterol, fluoconazole, clotrimazole, ketoconazole and voriconazole. The preincubation of each Candida species were carried out at 35°C, and late exponential phase cells were washed with PBS (pH 7.0) and resuspended in RPMI medium. The antifungal agents were dissolved in dimethyl sulphoxide (DMSO) and then added to inoculation, with a final cell concentration of approximately 1.5×106 cells/mL The concentrations of the antifungal agents were varied from 0.125, 0.25, 0.5, 1, 2, 4, 8, 16, 32, 64 to 128 µg/mL. The diluted Candida cells with the addition of varied doses of antifungal agents were incubated at 35°C for 24 h. Growth was determined by cell counts and quantisation of the numbers of colony-forming units (CFU) [11].
Microsomal preparation
The preparation of microsomes of C. albicans was carried out by a method described previously [12]. The cells were broken with a French Pressure cell at 20,000 psi and the cell debris was removed by centrifugation at 100,000g for 1 h at 4°C. Microsomal pellets were resuspended to a final protein concentration of 10 mg/mL, and the mixture was stored at −80°C until use. Protein concentration was determined at A600nm with bovine serum albumin as a standard. Assays for C24-SMT activity were conducted as described in our earlier studies [13]. The activity of SMT catalysis was characterised with respect to the observed ability of the enzyme to produce hexane-extractable 3H in the presence of [methyl-3H3] AdoMet. Briefly, the reaction mixture of freshly prepared enzyme in a final volume of 600 µL contained varying concentrations of sterol substrate from 5 to 100 µM, a fixed amount of 100 µM [methyl-3H3] AdoMet (0.6 µCi) and Tween 80 (1%, v/v), and 100 µL of C. albicans SMT and was incubated for 60 min. The enzymatic reaction was terminated by the addition of 600 µL of 10% methanolic KOH, followed by boiling for 20 min and extracting with three 2.5-mL portions of hexane [14].
Sterol biosynthesis assay
Cells of Candida species were incubated with radio-labelled substrates, [methyl-3H3] AdoMet. Then, washed cells were incubated in buffer A (50 mM Tris-HCl, 2 mM MgCl2, 2 mM β-mercaptoethanol and 20% glycerol (v/v), pH 6.8) and harvested after 18 h at 30°C by centrifugation at 10,000g for 20 min. The washed cells were resuspended in buffer B (0.1 mM potassium phosphate buffer, including 1 mM EDTA, 0.5 mM dithiothreitol and 20% (vol/vol) glycerol). Test compounds dissolved in DMSO were added to the cell suspensions (980 μL, 108 cells/mL). The reaction mixture also consisted of cofactor solution (100 μl; containing 1 μmol of NADP+, 1 μmol of NADPH, 1 μmol of NAD+, 3 μmol of glucose-6-phosphate, 5 μmol of ATP and 3 μmol of reduced glutathione) and divalent cation solution (10 μL of 0.5 mM MgCl2 and 5 μL of 0.4 mM MnCl2). The reaction was initiated by the addition of 100 μL of [methyl-3H3] AdoMet and the cells were incubated at 30°C for 1.5 h with shaking (110 rpm). The reaction was stopped by the addition of 1 mL 10% (w/v) KOH, 90% ethanol, and the samples were saponified at 80°C for 30 h [15]. The saponified lipids were then extracted with hexane and combined for separation by high-performance liquid chromatography (HPLC). All of the collections of each peak from HPLC were analysed by combined capillary gas chromatography-mass spectrometry (GC-MS), performed on a Hewlett-Packard 6890 GC-quadropole mass selective detector interfaced with a Hewlett-Packard Chemstation. A fused silica capillary column (0.25 µM/mm, i.d. 30 µm) coated with a 0.25-µm film of ZB-5 purchased from Phenomenex, Torrrance, CA, was employed with He as the carrier gas (10 psi) set at 1.2°C (1 min hold) to 280°C at 20°C/min. EI were recorded at 70 eV with the electron multiplier voltage set at 2,200 V. Full mass spectra were obtained and the products identified by a comparison of the retention time and spectrum to those of the authentic standard referenced to cholesterol [12].
LDH assay for hepatic damage
Liver cells collected from 70-day-old mice were resuspended with a final density of 1.5×106 cells/mL in RPMI1640 medium and incubated for 60 min with a certain dose (maximum of each MICs determined above) of antifungal agents at 37°C, 5% CO2. As a quantitative measure of cellular toxicity, the cytotoxic release of LDH in the culture medium was estimated using the CytoTox96 non-radioactive cytoxicity assay kit purchased from Promega Co. Ltd. The activities of LDH released into the culture medium were determined spectrophotometrically by A490nm at 3, 6, 12 and 24 h separately [16].
MTT assay for hepatic proliferation
MTT (3-(4,5-dimethyl-2-thiazolyl)-2,5-diphenyl-2H-tetrazolium bromide) (Promega Co. Ltd.) was a yellow water-soluble tetrazolium dye that was reduced by liver cells to a water-insoluble purple formazan. The amount of formazan could be determined spectrophotometrically. The A490nm of liver cells preincubated with varied concentrations of antifungal agents (0, 2.5, 5, 7.5, 12.5, 25, 37.5 and 50 µg/mL) were recorded and plotted in order to determine the ED50, which is the concentration of antifungal agents giving one-half inhibition to cell proliferation [17].
Results
Effect of 25-azalanosterol on the growth of Candida species
The antifungal activities of 25-azalanosterol, fluoconazole, clotrimazole, ketoconazole and voriconazole against Candida species were investigated and the results are summarised in Table 1. 25-Azalanosterol showed a wide range of anti-Candida activities, with MIC values ranging from 0.125 to 32 μg/mL. In particular, 25-azalanosterol showed significant potency against C. albicans, C. krusei and C. glabrata, which were close to clotrimazole, ketoconazole and voriconazole, but much greater than fluoconazole.
Effect of 25-azalanosterol on sterol biosynthesis
To determine the mechanism and target of growth inhibition by 25-azalanosterol, the relative rates of total cellular sterol synthesis in whole-cell homogenates of Candida species were measured in the presence of 80 μM 25-azalanosterol with [methyl-3H3] AdoMet. This approach was based on our earlier observation that 25-azalanosterol is a potent inhibitor of C24-SMT activity (Scheme 1) [14]. In this experiment, [methyl-3H3] AdoMet was added to Candida species that had been cultured previously in a medium without amino acids, in phosphate buffer containing glucose (2%, w/v). As shown in Fig. 2, the incorporation of [methyl-3H3] AdoMet into the C-24 of ergosterol was especially inhibited around 50% by the presence of 80μM 25-azalanosterol. The decrease in the incorporation of [methyl-3H3] AdoMet into ergosterol appeared to be a consequence of the inhibition of reactions involving C24-SMT, which was the key enzyme that catalysed the transmethylation of sterols from the precursor. Our previous study also indicated a dose-dependent inhibition of the rate of [methyl-3H3] AdoMet incorporation into ergosterol by 25-azalanosterol (IC50 20μM) [12].
Sterols biosynthesised in Candida species after incubation with the addition of 80 μM 25-azalanosterol. The sterol concentrations in the supernatant of cell homogenates were analysed by high-performance liquid chromatography (HPLC) and gas chromatography-mass spectrometry (GC-MS). The experimental results are shown as the average of three repetitions
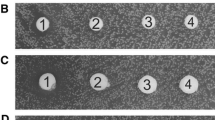
Hepatic toxicity of 25-azalanosterol on mice liver cells
LDH is released when cells are damaged or destroyed. Because of this, the LDH test could be used as a general marker of injury to cells or as a monitor of progressive conditions [17]. So, the LDH of mice liver cells exposed to antifungal agents for certain periods were analysed. From Fig. 3, it is clear that 25-azalanosterol exhibited the lowest inhibition compared to clotrimazole, ketoconazole and voriconazole, and especially much lower than fluoconazole. Meanwhile, since the MTT provided a more efficient format for assessing cellular proliferation, the critical component of the CellTiter 96 AQueous One Solution assay was used in this study to analyse the effect of these five antifungal agents on mice liver cell proliferation. Figure 4 shows the ED50 and MICs of mice liver cells exposed to five antifungal agents for 24 h. Clearly, the ED50 of 25-azalanosterol was the highest, which meant that its toxicity to liver cells was the lowest. Also, their ED50 and MICs were significantly different. Except for 25-azalanosterol, the ED50 of the other three antifungal agents, fluoconazole, clotrimazole and ketoconazole, were much lower than their maximal MICs, while the two values of voriconazole were close. This meant that 25-azalanosterol was the only agent which exhibited, at the clinical dosage level, little toxicity to liver cell, because its ED50 was higher than the maximum MIC, which suggests that 25-azalanosterol may have some form of indirect effect on C24-SMT in vivo.
Percentage of cytotoxic release of lactate dehydrogenase (LDH) in the culture medium of mice liver cells exposed to certain doses of antifungal agents: 32 μg/mL fluoconazole (open squares); 32 μg/mL ketoconazole (closed squares); 32 μg/mL clotrimazole (open triangles); 16 μg/mL voriconazole (closed triangles); 32 μg/mL 25-azalanosterol (open circles). The results are shown as the average of three repetitions
Comparison of minimum inhibitory concentrations (MICs) (solid bars) to the ED50 (open bars) of mice liver cells exposed to certain concentrations of antifungal agents. 1: 25-azalanosterol; 2: fluoconazole; 3: clotrimazole; 4: ketoconazole; 5: voriconazole. The results are shown as the average of three repetitions
It is well known that mammals and fungi share many reactions in their pathways of sterol biosynthesis [18], so we investigated whether lanosterol analogue, 25-azalanosterol, also inhibited mammalian cholesterol biosynthesis. As shown in Fig. 2, 25-azalanosterol (80 μM) almost completely blocked ergosterol biosynthesis by causing the accumulation of lanosterol and zymosterol, which, otherwise, would have been demethylated by 14-demethylase in Candida species, but exhibited virtually much less inhibition to mice hepatic cholesterol biosynthesis, and little toxicity to mammalian cells at the clinical dosage level.
Discussion
The azoles are fungistatic drugs by the inhibition of the cytochrome P-450-mediated removal of the C-14 methyl group from the ergosterol precursor, lanosterol, which are then subjected to the accumulation of resistant phenotypes due, in part, to the need of continuous administration to patients who are immuno-compromised [19]. Resistance has been reported in C. albicans as well as in other species of Candida [20, 21]. In addition, other fungal pathogens, including species of Histoplasma, Cryptococcus and Aspergillus [2], have been the subjects of recent reports on azole resistance. The increase in infections, coupled with the reduced efficacy of the currently available drugs, makes the discovery and development of new antifungal agents an urgent matter. The pathway for fungal sterol biosynthesis had provided an excellent target for antifungal development, but there remain additional sites in the pathway that have not been thoroughly investigated.
The identification of a novel antifungal drug with unique modes of action is desirable, since fungi resistant to currently available antifungal agents would unlikely be cross-resistant to these newer drugs. Based on our previous results that described the anti-Candida activities of 25-azalanosterol [12, 18], here, we set out a new class of drug derived from lanosterol that may be targetted against major enzymes involved in fungal growth. Our results indicated that the chemical modification of the natural lanosterol, such as the addition of a methyl, fluoro or bromol group, could lead to significant improvements in inhibitory activity against the growth of C. albicans [13, 22]. This modification was likely to have made the compound more lipophilic in nature, which, in turn, may have made it a more effective inhibitor of enzymes involved in lipids. However, this modification appeared to have changed its inhibitory behaviour against C24-SMT in vitro. In contrast, the inhibition abilities of fluoconazole or clotrimazole were not related to the inhibition ability of sterol C-14 demethylation, which were consistent with the results obtained in other studies [23]. Borgers et al. [24] reported that, in addition to their effects on sterol synthesis, the triazole antifungal agents affected ATPase as well as other membrane enzymes, membrane transport and fatty acid metabolism, which caused physical membrane damage. Thus, although 4-methyl-lanosterol effectively blocked the C24-SMT reaction in vivo, it failed to directly inhibit this enzyme activity in vitro. One explanation for this result may be that 25-azalanosterol was metabolised by the fungus to an inhibitor of C24-SMT activity. Alternatively, 25-azalanosterol may have had an, as yet unidentified, indirect effect on the C24-SMT reaction in vivo, which may mean that derivatives of lanosterol will represent a new class of antifungal compound with low host toxicity. These compounds may provide a safer alternative to fluoconazole or clotrimazole.
In conclusion, our results suggested that 25-azalanosterol has promising selective anti-Candida activity and deserves further in vitro and in vivo investigation.
References
Long SS, Stevenson DK (2005) Reducing Candida infections during neonatal intensive care: management choices, infection control, and fluconazole prophylaxis. J Pediatr 147:135–141
Blyth CC, Palasanthiran P, O’Brien TA (2007) Antifungal therapy in children with invasive fungal infections: a systematic review. Pediatrics 119:772–784
Pfaller MA, Pappas PG, Wingard JR (2006) Invasive fungal pathogens: current epidemiological trends. Clin Infect Dis 43:S3–S14
Fidel PL Jr, Vazquez JA, Sobel JD (1999) Candida glabrata: review of epidemiology, pathogenesis, and clinical disease with comparison to C. albicans. Clin Microbiol Rev 12:80–96
Hoppe JE (1997) Treatment of oropharyngeal candidiasis and candidal diaper dermatitis in neonates and infants: review and reappraisal. Pediatr Infect Dis J 16:885–894
Kauffman CA (2006) Endemic mycoses: blastomycosis, histoplasmosis, and sporotrichosis. Clin Infect Dis N Am 20:645–662
Kaufman D, Boyle R, Hazen KC, Patrie JT, Robinson M, Grossman LB (2005) Twice weekly fluconazole prophylaxis for prevention of invasive Candida infection in high-risk infants of <1000 grams birth weight. J Pediatr 147:172–179
Kim CK, Jeon KI, Lim DM, Johng T, Trzaskos JM, Gaylor JL, Paik YK (1995) Cholesterol biosynthesis from lanosterol: regulation and purification of rat hepatic sterol 14-reductase. Biochim Biophys Acta 1259:39–48
Kanagasabai R, Zhou WX, Liu JL, Nguyen TT, Veeramachaneni P, Nes WD (2004) Disruption of ergosterol biosynthesis, growth, and the morphological transition in Candida albicans by sterol methyltransferase inhibitors containing sulfur at C-25 in the sterol side chain. Lipids 39:737–746
Zhou WX, Lepesheva GI, Waterman MR, Nes WD (2006) Mechanistic analysis of a multiple product sterol methyltransferase implicated in ergosterol biosynthesis in Trypanosoma brucei. J Biol Chem 281:6290–6296
Kaneshiro ES, Rosenfeld JA, Basselin M, Stringer JR, Keely S, Smulian AG, Giner JL (2002) The Pneumocystis carinii drug target S-adenosyl-L-methionine: sterol C-24 methyl transferase has a unique substrate preference. Mol Microbiol 44:989–999
Zhou WX, Cross GA, Nes WD (2007) Cholesterol import fails to prevent catalyst-based inhibition of ergosterol synthesis and cell proliferation of Trypanosoma brucei. J Lipid Res 48:665–673
Wang JQ, Liu JL, Song ZH, Nes WD (2008) Sterol C24-methyltransferase: mechanistic studies of the C-methylation reaction with 24-fluorocycloartenol. Bioorg Med Chem Lett 18:232–235
Nes WD, Jayasimha P, Zhou WX, Kanagasabai R, Jin C, Jaradat TT, Shaw RW, Bujnicki JM (2004) Sterol methyltransferase: functional analysis of highly conserved residues by site-directed mutagenesis. Biochemistry 43:569–576
Arora A, Raghuraman H, Chattopadhyay A (2004) Influence of cholesterol and ergosterol on membrane dynamics: a fluorescence approach. Biochem Biophys Res Commun 318:920–926
Deyes R (2002) Cell viability assays. Promega Notes 81:32–33
Nanotechnology Characterization Laboratory (NCL) (2006) HEP G2 hepatocarcinoma cytotoxicity assay. NCL Method GTA-2. SAIC-Frederick Inc. pp 3–7
Wang JQ, Nes WD (2008) Mechanism and scope of cyclobranol modulated 24-sterol methyltransferase catalysis enzyme inactivation and concurrent C24-alkylation and dealkylation. J Biol Chem (in Press)
Worsham DN, Basselin M, Smulian AG, Beach DH, Kaneshiro ES (2003) Evidence for cholesterol scavenging by Pneumocystis and potential modifications of host-synthesized sterols by the P. carinii SAM:SMT. J Eukaryot Microbiol 50:678–679
Smith PB, Steinbach WJ, Benjamin DK Jr (2005) Neonatal candidiasis. Infect Dis Clin North Am 19:603–615
Zaoutis TE, Heydon K, Localio R, Walsh TJ, Feudtner C (2007) Outcomes attributable to neonatal candidiasis. Clin Infect Dis 44:1187–1193
Song ZH, Zhou WX, Liu JL, Nes WD (2004) Mechanism-based active site modification of the soybean sterol methyltransferase by 26,27-dehydrocycloartenol. Bioorg Med Chem Lett 14:33–36
Taylor FR, Rodriguez RJ, Parks LW (1983) Relationship between antifungal activity and inhibition of sterol biosynthesis in miconazole, clotrimazole, and 15-azasterol. Antimicrob Agents Chemother 23:515–521
Borgers M, Van den Bossche H (1982) The mode of action of antifungal drugs. Ketoconazole in the management of fungal disease. Adis Press, New York, pp 25–47
Acknowledgement
The authors wish to thank Prof. W. D. Nes for his assistance in the experimental procedures and the manuscript preparation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, J., Wu, J. Antifungal activity of 25-azalanosterol against Candida species. Eur J Clin Microbiol Infect Dis 27, 1131–1136 (2008). https://doi.org/10.1007/s10096-008-0554-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-008-0554-y