Abstract
Background
Recent medical advances have enabled the control of neurological symptoms and increased survival of patients with myasthenia gravis (MG). However, MG has many veiled consequences that may be underestimated by neurologists. Our aim was to clarify the social, professional, and neuropsychiatric issues of MG patients.
Methods
We carried out a cross-sectional cohort study with MG patients from a university-affiliated referral hospital. We registered clinical and sociodemographic data, and patients were classified according the MGFA classification. Clinical severity was assessed with Myasthenia Gravis Composite (MGC) scale. Trained and blind investigators analyzed social and professional outcomes. Neuropsychiatric symptoms were evaluated with the Hospital Anxiety and Depression Scale (HADS) and the social support with the Multidimensional Scale of Perceived Social Support (MSPSS).
Results
We enrolled 49 patients with MG. The mean age was 45.3 ± 18.1 years and 39 (79.6%) were women. There were 19 (38.8%) patients who become unemployed, 23 (46.9%) who had to retire prematurely, 31 (63.3%) that reported a significant reduction in work performance, and 23 (46.9%) who had a reduction in monthly income after the diagnosis of MG. Only 16 (32.6%) received any financial support and 24 (48.9%) patients had the perception of receiving a satisfactory social support. The practice of physical activity is a habit in only 10 patients (20.4%). Neuropsychiatric symptoms were present in 26 (53.1%) patients.
Conclusion
Patients with MG are vulnerable to social, professional, and mental disadvantages. Therapeutic success in MG goes beyond symptom relief and inevitably depends on a personalized approach to the patient.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
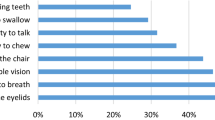
Myasthenia gravis (MG) is the most common neuromuscular junction disease, with a prevalence of 50 to 125 per million population [1]. It can begin in any age group, with incidence about three times higher in women in the age group up to 40 years, but with an increase in the male proportion in the age group over 50 years. MG is clinically marked by fluctuating muscle weakness such as ptosis, diplopia, dysarthria, dysphagia, dyspnea, weakness of arms and legs, and fatigue [2]. Yet, there is no cure for MG, but advancement in our understanding and treatment of MG has transformed it into one of the most treatable neuromuscular disorders [3]. Nevertheless, people suffering from MG experience lower quality of life, and the interferences of daily functioning due to the symptoms of MG are undeniable. Still, even today, many patients with MG find it difficult to maintain their daily activity levels due to insufficient improvement in disease status and the long-term side effects of treatment.
Although the disability resulting from MG usually leads to major disruptions of the patients’ social roles and quality of life, to date, this area of research has received little attention. Only a few studies have examined the effects of MG on the patient’s family life, psychological well-being, and the ability to keep a job or pursue leisure and recreational activities. Commonly, the measure of therapeutic success and disease severity assessment used in clinical studies relies only on clinical and physical examination data [4]. However, the consequences of MG are wide, varied, complex, and often reach the social and professional sphere of patients. Therefore, even in the daily clinical practice of the neurologist, the socio-professional outcomes of MG are invisible or at least underestimated. Moreover, there are few studies looking for possible predictors of the poor socio-professional scenario of these patients.
Successful management of MG depends on the interpretation of the patient in all its individual aspects. Therefore, the purpose of this study was to capture the prevalence and the associated factors of social and professional outcomes in patients with MG.
Methods
We carried out a cross-sectional cohort study that was conducted in a myasthenia gravis outpatient clinic of a university-affiliated, tertiary referral hospital in São Paulo, Brazil. All consecutive patients older than 18 years old admitted to our clinic with an established diagnosis of MG between January 2017 and June 2019 were eligible for participation in our study. Data collection and clinical evaluation of the patients were done by two independent neurologists so that the assessment of outcomes was done blindly to the patient’s clinical characteristics. Patients with any missing clinical data were excluded. Written informed consent was obtained from all patients before study inclusion and anonymity was assured. The study was approved by the local Ethics Committee.
The diagnosis of MG was based on clinical findings (fluctuating symptoms with easy fatigability and recovery after rest) with amelioration of symptoms after intravenous administration of anticholinesterase, decremental muscle response to a train of low-frequency repetitive nerve stimuli of 3 Hz, or the presence of autoantibodies specific for the acetylcholine receptor (AChR) of skeletal muscle (AChR-Ab) or for muscle-specific tyrosine kinase (MuSK-Ab).
Baseline data were collected through medical records and clinical interviews. We obtained information on patient’s demographics, social characteristics, habits (e.g., alcohol use, cigarette smoking, and use of illicit drugs), medical conditions, associated autoimmune disorders, use of other medications, previously diagnosed psychiatric disorders, number of prescribed medications, and daily number of drugs pills. Disease-related variables included first symptoms (ocular, bulbar, generalized symptoms), thymectomy, treatment profile (immunosuppressive agents, cholinesterase inhibitors, and steroids), duration of immunosuppression, time of diagnosis, and exacerbation in the past 1 year of the disease. The immunosuppressive agents possibly used were azathioprine and methotrexate. Adherence to pharmacological treatment was evaluated using the 8-item Morisky Medication Adherence Scale (MMAS-8). The total score ranges from 0 to 8 points, and those who score 8 points are considered adherent to the treatment 5.
Patients with MG were classified into subgroups according to clinical severity in the worst condition using MGFA Clinical Classification [6]. Neurological dysfunction was determined with the Myasthenia Gravis Composite (MGC) scale [7], which consists of 10 test items that measure symptoms and signs of MG, with weighted response options.
Outcomes
We assessed social and professional MG-related issues. All information of patients at diagnosis and at the time of the interview was sought from patients and confirmed by their relatives. We first elucidated whether each patient had experienced unemployment and unwilling job transfer and/or premature retirement. Those who remained employed were asked about reducing their monthly income, receiving financial assistance, or reducing their working capacity due to MG.
To examine the social impact of MG on patients and their relatives, four variables were studied. These were the marital and employment status, psychological well-being of patients and their relatives, and patients’ ability to continue their chosen recreational activities and to maintain their usual social relationships. We evaluated social support with the Multidimensional Scale of Perceived Social Support (MSPSS) [8]. A mean total scale score of more than 5 was considered as adequate/acceptable support. Patients were also asked about marital status and the number of inhabitants in the house. The regular practice of physical activity was investigated as well.
Assessment of neuropsychiatric symptoms was performed via the Hospital Anxiety and Depression Scale (HADS), a 14-item questionnaire that assesses symptoms of depression (HADS-D) and anxiety (HADS-A). Total scores range from 0 to 21 on each scale and scores ≥ 11 indicate probable anxiety or depression [9]. All outcomes found were associated with the clinical and demographic characteristics of the patients, including the severity of the disease.
Statistical analysis
Continuous variables are presented as means and standard deviations and categorical variables are presented as counts and percentages. Dichotomous or categorical variables were compared using the Chi-square test. Differences in continuous variables were assessed using the Student’s t test. For all the analyses, P < 0.05 for the two-tailed tests was considered statistically significant. All statistical analyses were performed using IBM SPSS Statistics 22.0 (IBM Corp. New York, NY, USA).
Results
The crude cohort consisted of 57 patients. After excluding 8 patients whose information could not be confirmed or refused to participate in the study, 49 patients were enrolled in the study. The mean age was 45.3 ± 18.1 years (range: 20–83 years) and 39 (79.6%) were women. There was no difference between men and women regarding age, type of clinical presentation, and duration of myasthenia gravis. The mean duration of the disease was 8.5 ± 7.2 years (range: 0–31 years). There were 7 (14.3%), 21 (42.8%), 17 (34.7%), and 4 (8.2%) patients with class I, class II, class III, and class IV, regarding the worst MGFA classification, respectively. All the patients presented compatible findings with MG in electroneuromyography and 9 (15.5%) patients were seronegative. Among the comorbidities present, 34.6% endocrinological, 28.9% were cardiological, 17.4% rheumatological, 5.8% neurological, 3.8% gastroenterological, 1.9% pneumological, 1.9% psychiatric, 1.9% otorhinolaryngological, 1.9% ophthalmological, and 1.9% hematological. Among the patients who used immunosuppressive agents, 30 (81.1%) used azathioprine and 7 (18.9%) methotrexate. Details of the clinical and demographic characteristics are presented in Table 1.
Among our patients, due to MG, 19 (38.8%) become unemployed, 20 (40.8%) were taken off work at least once, and 8 (16.3%) needed to change jobs or perform other paid functions (Table 2). Regarding the employed patients, the mean age was 50.6 years, the mean duration of immunosuppressant use was 2.7 years, and the mean HAD score was 10.4 years. Only 16 (32.6%) received any financial support while 23 (46.9%) had to retire prematurely due to the disease. Furthermore, 31 (63.3%) patients reported a significant reduction in work performance and 23 (46.9%) had a reduction in monthly income after the diagnosis of MG. Those who became unemployed were more likely to have been on prolonged immunosuppressive therapy, to have neuropsychiatric manifestations, to be younger, and to have started symptoms earlier (p < 0.05).
The practice of a physical activity is a habit in only 10 patients (20.4%). The regular practice of physical activity was significantly associated with a lower HAD score (4.9 vs 10.7, p = 0.02). Only 24 (48.9%) patients had the perception of receiving satisfactory social support. Regarding marital status, 31.7% were married, 46.3% were single, 19.5% were separated or divorced, and 2.4% were widowed. Living alone was reported by only 4.1% of MG patients. Neuropsychiatric symptoms were present in 26 (53.1%) patients. In contrast, only 14 (22.6%) patients were diagnosed with mood disorders. Being female (92.3%), using immunosuppressants (92.3%), inaugurating the disease with its generalized form (92.3%) and having frequent exacerbations were associated with neuropsychiatric disorders (42.3%) (p < 0.05). Detailed characterization of patients according to outcomes is expressed in Table 3.
Discussion
A substantial number of patients with MG are burdened with socioeconomic disadvantages. We found that at least two out of three MG patients will suffer changes in work and/or income. A large cohort in Japan demonstrated that unemployment or a decrease in income was experienced by approximately one-third of MG patients [10]. In a study in Thailand, the unemployment rate among patients with MG was 26–58%, and reduced income was seen in almost half of the population [11]. In a German MG cohort, 21.0% of the patients experienced hardships in their jobs, and 28.3% were forced to retire early due to MG [12]. In a community-based survey of Australian patients with MG, 39.4% had been forced to stop working due to MG, and 19.4% had to change their occupation [13]. In our country, the unemployment rate is found to be much higher than the countrywide rate of 2019 (11.0%). Participation in work is important because of the financial resources and access to benefits that jobs provide (including conditions for the treatment of MG [5]), and also because of a person’s sense of self-respect, social network, and feelings of usefulness and personal satisfaction [12]. Besides, while at work, individuals are stimulated by physical and mental activities, which is particularly important in MG. Professional changes can be naturally attributed to the physical difficulties of MG. Nevertheless, our study also suggests that the professional consequences seem to affect democratically MG patients. Boscoe et al. corroborate this finding by demonstrating that whether or not refractory MG, the impairment in professional life is notorious [14].
The treatment of a neurological disease cannot fail to highlight the social aspects related to the illness, especially the social support that the patient with MG must receive. We demonstrated that MG patients are “socially vulnerable” as they do not have the social support they deem necessary. Nagane et al. have already described a significant decreased social positivity in MG patients [10]. High functional disability and poor treatment outcomes have already been associated with lower social support in neurological disorders [15]. Moreover, social support has also moderated the relationship between depressive symptoms and functional disability. Indeed, social support was one of the effective factors for quality of life and well-being of patients with chronic neurological diseases [16]. Therefore, enhancement of social support is highly recommended as an important part of the treatment for neurological disorders, including MG.
Traditionally, exercise was thought to exacerbate symptoms of patients suffering from MG as their muscle weakness and fatigue were thought to be brought on or worsened by physical exertion and improved with rest. Nevertheless, physical exercise is currently known to be beneficial for adults with established MG [17]. Previous studies show that despite the disease, engagement in sports activities increases strength, reduces the levels of fatigue, and promotes symptom improvement [18, 19]. Also, physical activity gives confidence to MG patients and helps them understand their disease and their limits. Indeed, recently, the use of exercise has been proposed in the management of various neuromuscular diseases [20]. Unfortunately, we showed that only a few MG patients regularly exercise. Possible explanations include patients’ misinformation about the role of physical activity and doctors’ lack of adequate incentive and recommendation. The recognition of this information can provide insights to prevent neurologists and patients from neglecting physical activity in MG.
We found a significant prevalence of mood disorders in our MG cohort. The high risk of neuropsychiatric diseases is consistent with previous reports of high rates of depression and anxiety in patients with MG [21, 22]. This correlation has already been found in studies of patients with other autoimmune chronic diseases [23, 24] and neurodegenerative disorders [25]. However, there are very few data on the prevalence and the consequences of such psychiatric symptoms in patients with MG, and those available in the literature are generally from old studies with poor methodology. Therefore, it is not uncommon that neurologists underestimate the risk of psychiatric comorbidities in these patients [26]. In our study, a piece of possible evidence that corroborates this fact is that surprisingly, only half of the patients diagnosed with mental disorders were diagnosed and were receiving adequate treatment. Three mechanisms may explain the neuropsychiatric manifestations of MG: the direct immune effect of the disease on the brain, the MG-related physical disability/impairment, and the adverse effects of medications used to treat MG [27,28,29]. Indeed, patients using immunosuppressors with generalized disease and recent exacerbations appear to be at higher risk for associated mood disorders. Recognizing and treating mental illness must be a priority when treating patients for MG.
We present an original study that assesses many underrated issues of patients with MG and with direct implications in clinical practice. It is pioneering research that evaluates different outcomes of MG pertinent to all patients. We were able to include several variables and clinical scales, evaluating their potential relationship. This study has also some limitations that must be acknowledged to better interpret the results. One of the limitations of this study relates to the patient self-report method used. Nevertheless, adherence questionnaires are practical, inexpensive, easily applicable, and validated tools that are commonly used in most studies of medication adherence. We were unable to discriminate between the occupation of our patients because, on the one hand, many of our patients performed many professional activities, on the other, the limits that determine the vulnerability of a profession to the symptoms of myasthenia gravis are also very tenuous. In addition, our sample is not very large, which may have reduced the statistical power of our study, and some baseline-specific characteristics could not be included (e.g., type of antibody). Another limitation pertains to the convenience sample which consisted of patients receiving treatment for MG in a specialized tertiary hospital. Probably due to this bias, for example, the number of patients using immunosuppressants is higher in our cohort [30]. Outcomes might be different in this sample as compared to patients who do not receive specialized care and reside in other regions of the country and beyond. While generalization of results might be an issue, the information in this study contributes to the extremely limited research literature, though further research using prospective longitudinal cohorts and larger representative sample sizes are recommended. It is recommended that future research explore these factors as they pertain to individuals with MG.
Conclusions
MG has several “invisible” but extremely important consequences. Our study suggests the importance of adopting a personalized approach to the MG patient. Therapeutic success in MG goes beyond symptom relief and should consider all the aspects involved as a result of the disease. Ignoring socioeconomic, professional, and mental issues in MG is allowing multiple conditions of inequality to plague the life of the patient.
References
Jayam Trouth A, Dabi A, Solieman N, Kurukumbi M, Kalyanam J (2012) Myasthenia gravis: a review. Autoimmune Dis 2012:874680–874610. https://doi.org/10.1155/2012/874680
Gilhus NE, Verschuuren JJ (2015) Myasthenia gravis: subgroup classification and therapeutic strategies. Lancet Neurol 4(10):1023–1036. https://doi.org/10.1016/S1474-4422(15)00145-3
Sanders DB, Wolfe GI, Benatar M, Evoli A, Gilhus NE, Illa I, Kuntz N, Massey JM, Melms A, Murai H, Nicolle M, Palace J, Richman DP, Verschuuren J, Narayanaswami P (2016) International consensus guidance for management of myasthenia gravis: executive summary. Neurology. 87(4):419–425. https://doi.org/10.1212/WNL.0000000000002790
Barnett C, Herbelin L, Dimachkie MM, Barohn RJ (2018) Measuring clinical treatment response in myasthenia gravis. Neurol Clin 36(2):339–353. https://doi.org/10.1016/j.ncl.2018.01.006
Vitturi BK, Pellegrinelli A, Valerio BCO (2019) Medication adherence in patients with myasthenia gravis in Brazil: a cross-sectional study. Acta Neurol Belg 120:83–89. https://doi.org/10.1007/s13760-019-01209-0
Jaretzki A, Barohn RJ, Ernstoff RM, Kaminski HJ, Keesey JC, Penn AS, Sanders DB (2000) Myasthenia gravis: recommendations for clinical research standards. Ann Thorac Surg 70(1):327–334. https://doi.org/10.1212/WNL.55.1.16
Burns TM, Conaway M, Sanders DB (2010) The MG composite: a valid and reliable outcome measure for myasthenia gravis. Neurology. 55(1):16–23. https://doi.org/10.1212/WNL.0b013e3181dc1b1e
Dahlem NW, Zimet GD, Walker RR (1991) The multidimensional scale of perceived social support: a confirmation study. J Clin Psychol 47(6):756–761. https://doi.org/10.1002/1097-4679(199111)47:6<756::AID-JCLP2270470605>3.0.CO;2-L
Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67(6):361–370. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x
Nagane Y, Murai H, Imai T, Yamamoto D, Tsuda E, Minami N, Suzuki Y, Kanai T, Uzawa A, Kawaguchi N, Masuda M, Konno S, Suzuki H, Aoki M, Utsugisawa K (2017) Social disadvantages associated with myasthenia gravis and its treatment: a multicentre cross-sectional study. BMJ Open 7(2):e013278. https://doi.org/10.1136/bmjopen-2016-013278
Kulkantrakorn K, Sawanyawisuth K, Tiamkao S (2010) Factors correlating quality of life in patients with myasthenia gravis. Neurol Sci 31(5):571–573. https://doi.org/10.1007/s10072-010-0285-6
Twork S, Wiesmeth S, Klewer J, Pöhlau D, Kugler J (2010) Quality of life and life circumstances in German myasthenia gravis patients. Health Qual Life Outcomes 8:129. https://doi.org/10.1186/1477-7525-8-129
Blum S, Lee D, Gillis D, McEniery DF, Reddel S, McCombe P (2015) Clinical features and impact of myasthenia gravis disease in Australian patients. J Clin Neurosci 22(7):1164–1169. https://doi.org/10.1016/j.jocn.2015.01.022
Boscoe AN, Xin H, L’Italien GJ, Harris LA, Cutter GR (2019) Impact of refractory myasthenia gravis on health-related quality of life. J Clin Neuromuscul Dis 20(4):173–181. https://doi.org/10.1097/CND.0000000000000257
Kamenov K, Cabello M, Caballero FF, Cieza A, Sabariego C, Raggi A, Anczewska M, Pitkänen T, Ayuso-Mateos JL (2016) Factors related to social support in neurological and mental disorders. PLoS One 11(2):e0149356. https://doi.org/10.1371/journal.pone.0149356
Winter Y, Von Campenhausen S, Gasser J et al (2010) Social and clinical determinants of quality of life in Parkinson’s disease in Austria: a cohort study. J Neurol 257(4):638–645. https://doi.org/10.1007/s00415-009-5389-7
Westerberg E, Molin CJ, Lindblad I, Emtner M, Punga AR (2017) Physical exercise in myasthenia gravis is safe and improves neuromuscular parameters and physical performance-based measures: a pilot study. Muscle Nerve 56(2):207–214. https://doi.org/10.1002/mus.25493
Westerberg E, Molin CJ, Nees SS, Widenfalk J, Punga AR (2018) The impact of physical exercise on neuromuscular function in Myasthenia gravis patients: a single-subject design study. Med (United States) 97(31):e11510. https://doi.org/10.1097/MD.0000000000011510
Lohi EL, Lindberg C, Andersen O (1993) Physical training effects in myasthenia gravis. Arch Phys Med Rehabil 74(11):1178–1180
Cup EH, Pieterse AJ, ten Broek-Pastoor JM, Munneke M, van Engelen BG, Hendricks HT, van der Wilt GJ, Oostendorp RA (2007) Exercise therapy and other types of physical therapy for patients with neuromuscular diseases: a systematic review. Arch Phys Med Rehabil 88(11):1452–1464. https://doi.org/10.1016/j.apmr.2007.07.024
Kulaksizoglu IB (2007) Mood and anxiety disorders in patients with myasthenia gravis: aetiology, diagnosis and treatment. CNS Drugs 21(6):473–481. https://doi.org/10.2165/00023210-200721060-00004
Ybarra MI, Kummer A, Frota ERC, de Oliveira JT, Gomez RS, Teixeira AL (2011) Psychiatric disorders in myasthenia gravis. Arq Neuropsiquiatr 69(2A):176–179. https://doi.org/10.1590/s0004-282x2011000200006
Vitturi BK, Nascimento BAC, Alves BR, de Campos FSC, Torigoe DY (2019) Cognitive impairment in patients with rheumatoid arthritis. J Clin Neurosci 69:81–87. https://doi.org/10.1016/j.jocn.2019.08.027
Kronish IM, Rieckmann N, Halm EA, Shimbo D, Vorchheimer D, Haas DC, Davidson KW (2006) Persistent depression affects adherence to secondary prevention behaviors after acute coronary syndromes. J Gen Intern Med 21(11):1178–1183. https://doi.org/10.1111/j.1525-1497.2006.00586.x
Scalzo P, Kummer A, Cardoso F, Teixeira AL (2009) Depressive symptoms and perception of quality of life in Parkinson’s disease. Arq Neuropsiquiatr 67(2A):203–208. https://doi.org/10.1590/s0004-282x2009000200006
Misra UK, Kalita J, Singh VK, Kumar S (2019) A study of comorbidities in myasthenia gravis. Acta Neurol Belg 0123456789:59–64. https://doi.org/10.1007/s13760-019-01102-w
Brown ES, Chandler PA (2001) Mood and cognitive changes during systemic corticosteroid therapy. Prim Care Companion J Clin Psychiatry 3(1):17–21. https://doi.org/10.4088/PCC.v03n0104
Keesey JC (1999) Does myasthenia gravis affect the brain? J Neurol Sci 170(2):77–89. https://doi.org/10.1016/S0022-510X(99)00205-1
Aysal F, Karamustafalioǧlu O, Özçelik B et al (2013) The relationship of symptoms of anxiety and depression with disease severity and treatment modality in myasthenia gravis: a cross-sectional study. Noropsikiyatri Ars 50(4):295–300. https://doi.org/10.4274/npa.y5611
Santos E, Bettencourt A, Duarte S, Gabriel D, Oliveira V, da Silva AM, Costa PP, Lopes C, Gonçalves G, da Silva BM, Leite MI (2019) Refractory myasthenia gravis: characteristics of a Portuguese cohort. Muscle Nerve 60(2):188–191. https://doi.org/10.1002/mus.26507
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical approval
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vitturi, B.K., Kim, A.I.H., Mitre, L.P. et al. Social, professional and neuropsychiatric outcomes in patients with myasthenia gravis. Neurol Sci 42, 167–173 (2021). https://doi.org/10.1007/s10072-020-04528-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-020-04528-w