Abstract
Introduction
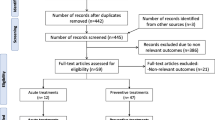
Chronic migraine is a disease of altered cortical excitability. Repetitive transcranial magnetic stimulation provides a novel non-invasive method to target the nociceptive circuits in the cortex. Motor cortex is one such potential target. In this study, we targeted the left motor cortex using fMRI-guided neuronavigation.
Materials and Methods
Twenty right-handed patients were randomized into real and sham rTMS group. Baseline subjective pain assessments were done using visual analog scale (VAS) and questionnaires: State-Trait Anxiety Inventory, Becks Depression Inventory, and Migraine Disability Assessment (MIDAS) questionnaire. Objectively, pain was assessed by means of thermal pain thresholds using quantitative sensory testing. For corticomotor excitability parameters, resting motor thresholds and motor-evoked potentials were mapped. For rTMS total, 600 pulses in 10 trains at 10 Hz with an intertrain interval of 60 s were delivered in each session. Ten such sessions were given 5 days per week over 2 consecutive weeks. The duration of each session was 10 min. Real rTMS was administered at 70% of Resting MT. All the tests were repeated post-intervention and after 1 month of follow-up. There are no studies reporting the use of fMRI-based TMS for targeting the motor cortex in CM patients.
Results
We observed a significant reduction in the mean VAS rating, headache frequency, and MIDAS questionnaire in real rTMS group which was maintained after 1 month of follow-up.
Conclusion
Ten sessions of fMRI-based rTMS over the left motor cortex may provide long-term pain relief in CM, but further studies are warranted to confirm our preliminary findings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Repetitive transcranial magnetic stimulation (rTMS) has emerged as a novel treatment for migraine [1,2,3]. Chronic migraine (CM) is a by-product of processes altering cortical excitability [4, 5]. Existing literature suggests that higher frequency rTMS is effective and “well tolerated” for CM [3, 6, 7]. The mechanisms of pain relief remain unexplored accompanied by variations in the findings of sensory tests and corticomotor excitability parameters in CM patients [7, 8]. There are inadequate studies that report the efficacy of multiple-session rTMS in CM patients along with the paucity of optimal stimulation parameters for persistent analgesic effect [3, 9]. There are no studies reporting the use of fMRI-based TMS targeting the motor cortex in CM patients. Here, we ventured to explore the substrate for the pain relief using neuronavigation over the left motor cortex and investigated the efficacy of 10 sessions of high-frequency rTMS paradigm.
Material and methods
Subject recruitment and randomization
The study was approved by the Institute Ethics Committee, All India Institute of Medical Sciences, New Delhi, and registered in Clinical Trial Registry, India CTRI/2017/02/007973. Twenty right-handed participants (11 females, 9 males; age 33 ± 8 years, mean ± SD) diagnosed with CM (ICHD 2013 code 1.3) were recruited from Neurology Headache Clinics, AIIMS, New Delhi. None of the patients had aura or side predominance of attack. Medications of patients were not discontinued (see Table 1). Patients with other forms of headache or any chronic comorbidity or psychiatric illness were excluded. Medication overuse headache was ruled out before recruitment. Clinical examination was done, and informed written consent was taken from each participant. Both investigator and participants were blinded during the study. Stratified block randomization was generated at www.randomiser.com and kept in a sealed opaque envelope by a third party who was not a part of the study.
Recording and measurements
Each subject maintained headache diary for headache frequency, rescue medication, and associated symptoms. Mean headache intensity was assessed using the visual analog scale (VAS) rating. Headache-associated disability was assessed before therapy, and after 3 months of follow-up by the Migraine Disability Assessment (MIDAS) questionnaire. Patient anxiety and depression were assessed using State-Trait anxiety inventory (STAI) and Becks depression inventory (BDI) at three time point i.e., baseline/pre-intervention, post-intervention, and after 1 month follow-up.
Functional MRI (using Ingenia 3T, Philips Healthcare, The Netherlands) was done during right-hand thumb abduction (Abductor Pollicis Brevis muscle), to localize the area over the left primary motor cortex (M1) cortex. After fMRI recording at NMR facility, AIIMS, New Delhi, subjects were called for neuro-navigated (Neural Navigator Software 2.2, Brain Science Tools BV., The Netherlands) targeting of M1 and measurement of corticomotor excitability parameters using TMS device (Neuro MS/D TMS device, Neurosoft, Russia) with a figure of 8 coil (Model FEC-02-100-C) over the M1. The scalp was kept grease-free and the common impedance for recording electrodes was maintained below 10 kΩ. The coil was oriented anteroposteriorly, inclined at 45° from the midline and placed tangentially over the left side of the scalp.
Neuro-navigated M1 coordinates for APB
Participant’s M1 coordinates were obtained for the right ABP muscle using NeNa software (Supplementary Table 1). Neuro-navigation provided accurate localization of the M1 and helped to repeat the procedure for localization during future sessions (Supplementary Fig. 1).
Surface EMG was recorded using Ag/AgCl ECG electrodes (REF: F3001ECG, Fiab, Italy) by placing patch electrodes 3 cm apart over APB muscle belly and tendon. Resting motor threshold (RMT) was recorded as the minimum intensity of stimulator output that produced motor-evoked potential (MEP) amplitude greater than 50 μV in 3 of 6 trials. MEP amplitude and latency were determined at intensities ranging from 110 to 150% of RMT. All the above parameters were recorded at Pain Research and TMS Laboratory, AIIMS, New Delhi, and repeated on completion of therapy and after 1 month for follow-up.
Repetitive TMS therapy
A total of 600 pulses in 10 trains at 10 Hz with an intertrain interval of 60 s were delivered in each session over the M1 [3]. Ten such sessions were given 5 days per week over 2 consecutive weeks. The duration of each session was 10 minutes. Real rTMS was administered at 70% RMT using the same orientation as for determining RMT and MEP. To achieve sham stimulation, the coil was placed perpendicularly to the vertex at the minimum stimulation strength of the stimulator. Thus, the magnetic field did not penetrate the scalp although the patient heard the sound produced by the coil.
Quantitative sensory testing (QST)
The thermal tests were performed using Neurosensory analyzer device MEDOC TSA 2001-II apparatus (Medoc, Ramat-Yishai, Israel). The system contains a metal contact plate (contact area 30 × 30 mm) that was cooled and heated by an external Peltier/Foil element to the target levels. Medoc TSA-II was used to quantitatively assess the thermal thresholds of subjects. The neurosensory analyzer was set to baseline temperature (32 °C) and depending on paradigm/test applied temperature was raised or lowered by 1 °C/s. Lower limits of 0 °C and upper limit of 50 °C were set to prevent any thermal damage to the site to be tested. The tests for determining thermal pain thresholds (cold and hot) were first done at the left hand (dorsum of thumb) which was the reference site in our study.
Statistical analysis
All analysis was performed using GraphPad Prism version 5. Baseline scores of parameters were checked for normality using D’Agostino and Pearson omnibus test. To compare the changes between real vs sham rTMS group at three different time points, i.e., baseline/pre-intervention, post-intervention, and follow-up, Mann-Whitney U or unpaired t test was used for non-parametric or parametric data, respectively. For comparison of the changes within the real/sham rTMS therapy group for three different time points, i.e., baseline/pre-intervention, post-intervention, and follow-up, either one-way ANOVA followed by post hoc Tukey test or Kruskal-Wallis test followed by post hoc Dunn’s test was used for parametric and non-parametric data, respectively. Data are expressed as mean ± SD and/or median (25Q–75Q).
Results
Both groups had similar demographic characters (Table 2). The rTMS was generally well tolerated and no side effects were reported.
Subjective assessment of pain
One-way ANOVA of VAS scores for within-group comparison of Real rTMS (8.000 ± 1.33 vs 4.200 ± 2.04 vs 4.800 ± 2.25; p = 0.0003, F = 11.38) and sham rTMS group (7.70 ± 1.42 vs 6.60 ± 1.35 vs 6.70 ± 1.29, p = 0.15, F = 2.02) showed significant difference in Real rTMS group. Tukey’s multiple comparison test revealed a significant difference between baseline vs post-intervention, and baseline vs follow-up VAS score of real rTMS group. No significant difference observed between post-treatment vs follow-up VAS score of real rTMS group proves that the effect was maintained until a month of follow-up period (Fig. 1).
The graph shows mean VAS scores of chronic migraine patients in sham and real rTMS group at baseline/pre-intervention, post-intervention, and follow-up stages. Data is expressed as mean ± SD. Comparison between baseline/pre-intervention, post-intervention, and follow up stages within sham/real group were done with one-way ANOVA followed by post hoc analysis by Tukey test (**p < 0.01, ***p < 0.001)
The headache frequency per month was noted, and within-group comparison of real rTMS group (17.4 ± 1.33 vs 10.2 ± 2.21 vs 9.8 ± 1.8, p ≤ 0.0001, F = 55.67) and sham rTMS group (17.6 ± 1.42 vs 18 ± 1.6 vs 18.5 ± 2.1) showed significant difference in real rTMS group only. Post hoc analysis for real rTMS group with Tukey’s multiple comparison test indicated a significant difference between baseline/pre-intervention vs follow-up (Fig. 2).
The graph shows headache frequency of chronic migraine patients in sham and real rTMS group at baseline/pre-intervention, post-intervention, and follow-up stages. Data is expressed as mean ± SD. Comparison between baseline/pre-intervention, post-intervention, and follow-up stages within sham/real rTMS group were done with one-way ANOVA followed by post hoc analysis by Tukey test (***p <0.001)
The MIDAS scores between real rTMS vs sham rTMS group at 3 months follow-up (3.700 ± 4.001 vs 13.80 ± 19.40; p = 0.1243) did not show any difference. A significant difference was observed when the comparison was done between pre-intervention vs follow-up within real rTMS (30.30 ± 30.18 vs 3.700 ± 4.001; p = 0.0157) or sham rTMS (24.50 ± 21.16 vs 13.80 ± 19.40; p = 0.0293) group with paired t test after checking for normality.
The STAI-State scores between real rTMS 55.10 ± 14.39, 52.90 ± 17.08, 50.60 ± 14.44 vs sham rTMS 48.90 ± 13.11, 21.70 ± 13.17, 24.10 ± 15.88 did not vary significantly between baseline/pre-intervention, post-intervention, and follow-up. The STAI-Trait scores between real rTMS 57.80±13.51.57.80 ± 15.41, 50.30 ± 15.99 vs sham rTMS 53.50 ± 13.20, 50.40 ± 13.54, 47.60 ± 9.72 did not vary significantly between baseline/pre-intervention, post-intervention, and followup. No significant changes were observed in within group comparison of sham or real rTMS group.
The BDI-II scores between real rTMS 30.90 ± 13.14, 23.80 ± 12.43, and 25.30 ± 18.671 vs sham rTMS 30.70 ± 16.67, 46.60 ± 12.96, and 45.10 ± 11.83 did not vary significantly between baseline, post-intervention, and follow-up. No significant changes were observed in within group comparison.
Corticomotor excitability
Resting motor threshold
No significant difference was observed during within group comparison in real rTMS [30.00 (30.00, 60.75) vs 30.00 [30.00, 41.25) vs 37.50 (30.00, 45.00); p = 0.1696] or sham rTMS [30.00 (30.00, 42.50) vs 30.00 (30.00, 32.50) vs 30.00 (30.00, 40.00); p = 0.7517] group.
Motor-evoked potential
The baseline/pre-intervention vs post-intervention comparison of MEP amplitudes (mV) at 110, 120, 130, 140, and 150% RMT in real rTMS vs sham rTMS group was not significantly different (Table 3). The comparison of MEP latency (ms) in real rTMS vs sham rTMS group [19.75 (15.30, 24.28) vs 21.65 (16.48, 33.48)] was also not significant (Table 4).
To understand the changes in sham and real groups the MEP amplitude is expressed as change within three-time points of baseline, post-intervention, and follow-up (Figs. 3, 4, and 5).
Change in motor-evoked potential amplitude post-intervention from baseline in sham and real rTMS groups. The difference in MEP amplitude (post-intervention– baseline) at different percentages of the resting motor threshold is represented as median with interquartile range and was statistically not significant
Change in motor-evoked potential amplitude at follow-up from post-intervention sham and real rTMS groups. The difference in MEP amplitude (follow up– postintervention) at different percentages of the resting motor threshold is represented as median with interquartile range and was statistically not significant
Quantitative Sensory testing
Cold pain thresholds did not show any significant changes in the sham rTMS group (Fig. 6) but they were significantly decreased between baseline vs follow-up and baseline vs post-intervention in the real rTMS group (Fig. 7).
Hot pain thresholds were not significantly different in sham group (Fig. 8) and real group (Fig. 9).
Discussion
The main finding of the present study is that ten sessions of high-frequency rTMS over the primary motor cortex attenuates pain in patients with chronic migraine and the effect is maintained for at least 1 month. The subjective pain relief was not accompanied by significant changes in the corticomotor excitability.
Our results are consistent with the available literature on chronic migraine [1, 3, 9] which provided evidence of the efficacy and safety of 10 Hz rTMS over the motor cortex in migraine prophylaxis. The primary motor cortex might represent an appropriate portal to reach deep brain structures with difficult access: the motor cortex stimulation triggers corticothalamic output to the brainstem, spinal cord, and also limbic system and hence, modulates the pain matrix [10]. We observed a significant reduction in the VAS rating for pain which was maintained after 1 month of follow-up. Pain relief was also reflected by the reduction in headache frequency which further decreased after follow-up, suggesting that rTMS triggered a synaptic plasticity causing reverberation in the neural circuitry which may outlast the period of active stimulation [11]. We did not get any significant reduction in the anxiety scales (State-Trait Anxiety Inventory) or depression gauged by Becks Depression Inventory. Such changes are consistently seen with rTMS over the dorsolateral prefrontal cortex [12, 13]. Motor cortex stimulation does not perhaps efficiently target the affective-emotional circuitry of pain [14].
We also observed a significant reduction in the overall impact caused by migraine on the patient's life; this was reflected in the MIDAS scores of patients. Studies targeting motor cortex rTMS for chronic pain conditions have previously reported a reduction in disability and an improvement in the quality of life [14, 15]. These studies indicate that motor cortex rTMS has a common mechanism of reducing disability both in widespread chronic pain of fibromyalgia and localized chronic pain of Chronic Regional Pain Syndrome type 1.
Despite getting significant changes in the subjective pain, the changes failed to echo in the neurophysiological parameters of corticomotor excitability. The resting motor thresholds and the motor-evoked potentials did not show any changes in the recruitment pattern after intervention or follow-up. This is in line with the post train observations done for rTMS of limited pulses. No change in MEP size was seen for stimulation intensity of 100% RMT or below as well as for train of 1600 pulses or less [16,17,18,19,20]. The resting motor threshold also did not show any change following a train of stimulations used in previous studies [21, 22]. Though increased excitability at higher intensities with a greater number of pulses was observed, even so, there is a paucity of evidence regarding modulation in cortical excitability at higher frequencies of 10 and 20 Hz which are frequently used for therapeutic purposes [23]. This study fills this gap in the literature suggesting that no changes occur in excitability post multiple sessions of multiple trains at higher frequency of 10 Hz. Also, as suggested by previous studies, the use of neuronavigation during the application of rTMS is associated with a focused neurophysiologic impact when compared to therapy without neuronavigation [24]. The unavoidable scattering of the stimulus locations, during non-navigated rTMS, may explain this discrepancy. Neural navigation achieves greater precision in targeting the cortical areas resulting in an efficient transsynaptic, interhemispheric impact [25]. MEPs reflect the net sum of local excitatory and inhibitory input onto pyramidal cells within the motor cortex and lack of change in MEP amplitudes has been also reported previously [26, 27]. Perhaps this may be attributed to the paradoxical cortical hyperresponsivity seen in migraineurs due to homeoplastic effects which may prevent the attainment of suprathreshold activations [1, 28, 29].
In our data of quantitative sensory testing of cold/hot pain thresholds, we observed a significant decrease in the cold pain threshold in the real rTMS group. But our small sample size prevents us from drawing any firm conclusions from this. Possibly, high-frequency rTMS that was applied to the motor cortex increased the excitability of the anterior cingulate cortex which further activates medial thalamus, and finally, it decreased the participant’s thermal pain threshold [30]. These medial systems are probably separable from the somatosensory system; therefore, they could have produced a dissociable effect on the sensory perception threshold [31, 32] which we observed in our study.
The mechanism of pain relief appears to be top-down modulation of descending pain control system as functional connectivity is revealed between the motor cortex, thalamus, insula, anterior cingulate cortex, and periaqueductal gray [10, 33, 34]. Post-TMS increased levels of β-endorphins and dopamine and changes in the level of other neurotransmitters and neuromodulators have been documented [35, 36]. Maintenance of the effect for 1 month suggests the establishment of neuroplasticity, which can be explained based on long-term potentiation (LTP) of pain modulating areas that are functionally connected to the motor cortex [37, 38].
Although present study is amongst the first few studies exploring the role of neuronavigation-based rTMS in chronic migraine, there a few limiting factors which should be taken into deliberation before we decisively comment on some of our results. One is the limited sample size of the study. Also, continuation of pharmacological therapy, which could not be stopped due to chronicity of headache, is a potential confounding factor. Standalone sham coil should have been used for sham stimulation, instead of keeping the figure of 8 coil at different orientation for sham stimulation, to explain the placebo effects.
Conclusion
As chronic migraine becomes non-responsive to medicine, rTMS can be considered as adjuvant or independent therapy for the amelioration of migraine pain and headache frequency. Ten sessions of neuronavigated high-frequency repetitive transcranial magnetic stimulation of left primary motor cortex is a safe and effective therapy in decreasing chronic migraineurs’ pain and attack rate. As the present study could not find any significant relief in anxiety and depression levels possibly M1 should not be targeted for reducing the psychological and affective component of pain. The lack of any effects on cortical excitability needs further exploration with the neuropharmacological bases of the analgesia which may explain the dichotomy of effects over the sensory and pain thresholds.
References
Brighina F, Palermo A, Daniele O, Aloisio A, Fierro B (2010) High-frequency transcranial magnetic stimulation on motor cortex of patients affected by migraine with aura: a way to restore normal cortical excitability? Cephalalgia Int J Headache 30(1):46–52
Brighina F, Piazza A, Vitello G, Aloisio A, Palermo A, Daniele O, Fierro B (2004) rTMS of the prefrontal cortex in the treatment of chronic migraine: a pilot study. J Neurol Sci 227(1):67–71
Misra UK, Kalita J, Bhoi SK (2013) High-rate repetitive transcranial magnetic stimulation in migraine prophylaxis: a randomized, placebo-controlled study. J Neurol 260(11):2793–2801
Schoenen J (2006) Neurophysiological features of the migrainous brain. Neurol Sci 27(2):s77–s81
Barbanti P, Fofi L, Aurilia C, Egeo G (2019) Does the migraine attack start in the cortex and is the cortex critical in the migraine process? Neurol Sci 40(1):31–37
Teepker M, Hötzel J, Timmesfeld N, Reis J, Mylius V, Haag A, Oertel WH, Rosenow F, Schepelmann K (2010) Low-frequency rTMS of the vertex in the prophylactic treatment of migraine. Cephalalgia. 30(2):137–144
Conforto AB, Amaro E, Gonçalves AL, Mercante JP, Guendler VZ, Ferreira JR et al (2014) Randomized, proof-of-principle clinical trial of active transcranial magnetic stimulation in chronic migraine. Cephalalgia. 34(6):464–472
Andreou AP, Holland ÃPR, Akerman ÃS, Summ O, Fredrick J, Goadsby PJ (2016) Transcranial magnetic stimulation and potential cortical and trigeminothalamic mechanisms in migraine. Brain 139(Pt 7):2002–14
Kalita J, Laskar S, Bhoi SK, Misra UK (2016) Efficacy of single versus three sessions of high rate repetitive transcranial magnetic stimulation in chronic migraine and tension-type headache. J Neurol 263(11):2238–2246
García-Larrea L, Peyron R, Mertens P, Gregoire MC, Lavenne F, Le Bars D et al (1999) Electrical stimulation of motor cortex for pain control: a combined PET-scan and electrophysiological study. Pain. 83(2):259–273
Di Lazzaro V, Ziemann U (2013) The contribution of transcranial magnetic stimulation in the functional evaluation of microcircuits in human motor cortex. Front Neural Circuits 7(February):1–9
Mattoo B, Tanwar S, Bhatia R, Tripathi M, Bhatia R (2019) Repetitive transcranial magnetic stimulation in chronic tension-type headache: a pilot study. Indian J Med Res 150:73–80
Tanwar S, Mattoo B,Kumar U, Bhatia R (2020) Repetitive transcranial magnetic stimulation of the prefrontal cortex for fibromyalgia syndrome: a randomised controlled trial with 6-months follow up. Advances in Rheumatology. https://doi.org/10.1186/s42358-020-00135-7
Passard A, Attal N, Benadhira R, Brasseur L, Saba G, Sichere P, Perrot S, Januel D, Bouhassira D (2007) Effects of unilateral repetitive transcranial magnetic stimulation of the motor cortex on chronic widespread pain in fibromyalgia. Brain J Neurol 130(Pt 10):2661–2670
Picarelli H, Teixeira MJ, Ciampi de Andrade D, Myczkowski ML, Luvisotto TB, Yeng LT, Fonoff ET, Pridmore S, Marcolin MA, (2010) Repetitive transcranial magnetic stimulation is efficacious as an add-on to pharmacological therapy in complex regional pain syndrome (CRPS) Type I. J Pain Res 11(11):1203–1210
Wu T, Sommer M, Tergau F, Paulus W (2000) Lasting influence of repetitive transcranial magnetic stimulation on intracortical excitability in human subjects. Neurosci Lett 287(1):37–40
Pascual-Leone A, Valls-Solé J, Wassermann EM, Hallett M (1994) Responses to rapid-rate transcranial magnetic stimulation of the human motor cortex. Brain J Neurol 117(Pt 4):847–858
Modugno N, Nakamura Y, MacKinnon C, Filipovic S, Bestmann S, Berardelli A, Rothwell J (2001) Motor cortex excitability following short trains of repetitive magnetic stimuli. Exp Brain Res 140(4):453–459
Peinemann A, Reimer B, Löer C, Quartarone A, Münchau A, Conrad B, Roman Siebner H (2004) Long-lasting increase in corticospinal excitability after 1800 pulses of subthreshold 5 Hz repetitive TMS to the primary motor cortex. Clin Neurophysiol Off J Int Fed Clin Neurophysiol 115(7):1519–1526
Maeda F, Keenan JP, Tormos JM, Topka H, Pascual-Leone A (2000) Modulation of corticospinal excitability by repetitive transcranial magnetic stimulation. Clin Neurophysiol Off J Int Fed Clin Neurophysiol 111(5):800–805
Siebner HR, Mentschel C, Auer C, Lehner C, Conrad B (2000) Repetitive transcranial magnetic stimulation causes a short-term increase in the duration of the cortical silent period in patients with Parkinson’s disease. Neurosci Lett 284(3):147–150
Daskalakis ZJ, Möller B, Christensen BK, Fitzgerald PB, Gunraj C, Chen R (2006) The effects of repetitive transcranial magnetic stimulation on cortical inhibition in healthy human subjects. Exp Brain Res 174(3):403–412
Fitzgerald PB, Fountain S, Daskalakis ZJ (2006) A comprehensive review of the effects of rTMS on motor cortical excitability and inhibition. Clin Neurophysiol Off J Int Fed Clin Neurophysiol 117(12):2584–2596
Bashir S, Edwards D, Pascual-Leone A (2011) Neuronavigation increases the physiologic and behavioral effects of low-frequency rTMS of primary motor cortex in healthy subjects. Brain Topogr 24(1):54–64
Julkunen P, Säisänen L, Danner N, Niskanen E, Hukkanen T, Mervaala E, Könönen M (2009) Comparison of navigated and non-navigated transcranial magnetic stimulation for motor cortex mapping, motor threshold and motor evoked potentials. NeuroImage. 44(3):790–795
Fierro B, Piazza A, Brighina F, La Bua V, Buffa D, Oliveri M (2001) Modulation of intracortical inhibition induced by low- and high-frequency repetitive transcranial magnetic stimulation. Exp Brain Res 138(4):452–457
Berardelli A, Inghilleri M, Gilio F, Romeo S, Pedace F, Currà A, Manfredi M (1999) Effects of repetitive cortical stimulation on the silent period evoked by magnetic stimulation. Exp Brain Res 125(1):82–86
Cosentino G, Fierro B, Brighina F (2014) From different neurophysiological methods to conflicting pathophysiological views in migraine: a critical review of literature. Clin Neurophysiol Off J Int Fed Clin Neurophysiol 125(9):1721–1730
Cosentino G, Brighina F, Talamanca S, Paladino P, Vigneri S, Baschi R, Indovino S, Maccora S, Alfonsi E, Fierro B (2014) Reduced threshold for inhibitory homeostatic responses in migraine motor cortex? A tDCS/TMS study. Headache. 54(4):663–674
Mylius V, Borckardt JJ, Lefaucheur J-P (2012) Noninvasive cortical modulation of experimental pain. Pain. 153(7):1350–1363
Woolf CJ (2011) Central sensitization: implications for the diagnosis and treatment of pain. Pain 152(Supplement):S2–S15
Malo-Urriés M, Estébanez-de-Miguel E, Bueno-Gracia E, Tricás-Moreno JM, Santos-Lasaosa S, Hidalgo-García C (2020 [cited 2020 May 8]) Sensory function in headache: a comparative study among patients with cluster headache, migraine, tension-type headache, and asymptomatic subjects. Neurol Sci [Internet]. https://doi.org/10.1007/s10072-020-04384-8
Peyron R, Faillenot I, Mertens P, Laurent B, Garcia-Larrea L (2007) Motor cortex stimulation in neuropathic pain. Correlations between analgesic effect and hemodynamic changes in the brain. A PET study. NeuroImage. 34(1):310–321
Strafella AP, Paus T, Fraraccio M, Dagher A (2003) Striatal dopamine release induced by repetitive transcranial magnetic stimulation of the human motor cortex. Brain J Neurol 126(Pt 12):2609–2615
Misra UK, Kalita J, Tripathi G, Bhoi SK (2017) Role of β endorphin in pain relief following high rate repetitive transcranial magnetic stimulation in migraine. Brain Stimulat 10(3):618–623
Cho SS, Strafella AP (2009) rTMS of the left dorsolateral prefrontal cortex modulates dopamine release in the ipsilateral anterior cingulate cortex and orbitofrontal cortex. PLoS One 4(8):e6725
Lefaucheur JP, Drouot X, Ménard-Lefaucheur I, Nguyen JP (2004) Neuropathic pain controlled for more than a year by monthly sessions of repetitive transcranial magnetic stimulation of the motor cortex. Neurophysiol Clin Clin Neurophysiol 34(2):91–95
Lefaucheur J-P, André-Obadia N, Antal A, Ayache SS, Baeken C, Benninger DH, Cantello RM, Cincotta M, de Carvalho M, de Ridder D, Devanne H, di Lazzaro V, Filipović SR, Hummel FC, Jääskeläinen SK, Kimiskidis VK, Koch G, Langguth B, Nyffeler T, Oliviero A, Padberg F, Poulet E, Rossi S, Rossini PM, Rothwell JC, Schönfeldt-Lecuona C, Siebner HR, Slotema CW, Stagg CJ, Valls-Sole J, Ziemann U, Paulus W, Garcia-Larrea L (2014) Evidence-based guidelines on the therapeutic use of repetitive transcranial magnetic stimulation (rTMS). Clin Neurophysiol 125(11):2150–2206
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 1.62 MB)
Rights and permissions
About this article
Cite this article
Kumar, A., Mattoo, B., Bhatia, R. et al. Neuronavigation based 10 sessions of repetitive transcranial magnetic stimulation therapy in chronic migraine: an exploratory study. Neurol Sci 42, 131–139 (2021). https://doi.org/10.1007/s10072-020-04505-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-020-04505-3