Abstract
We report the efficacy of three versus single session of 10 Hz repetitive transcranial magnetic stimulation (rTMS) in chronic migraine (CM) and chronic tension-type headache (CTTH). Ninety-eight patients with CM or CTTH were included and their headache frequency, severity, functional disability and number of abortive medications were noted. Fifty-two patients were randomly assigned to group I (three true sessions) and 46 to group II (one true and two sham rTMS sessions) treatment. 10 Hz rTMS comprising 600 pulses was delivered in 412.4 s on the left frontal cortex. Outcomes were noted at 1, 2 and 3 months. The primary outcome was 50 % reduction in headache frequency, and secondary outcomes were improvement in severity, functional disability, abortive drugs and side effects. The baseline headache characteristics were similar between the two groups. Follow up at different time points revealed significant improvement in headache frequency, severity, functional disability and number of abortive drugs compared to baseline in both group I and group II patients, although these parameters were not different between the two groups. In group I, 31 (79.4 %) had reduction of headache frequency and 29 (74.4 %) converted to episodic headache. In group II, these were 24 (64.8 %) and 22 (59.2 %), respectively. In chronic migraine, the severity of headache at 2 months reduced in group I compared to group II (62.5 vs 35.3 %; P = 0.01). Both single and three sessions of 10 Hz rTMS were found to be equally effective in CM and CTTH, and resulted in conversion of chronic to episodic headache in 67.1 % patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic daily headache (CDH) is characterized by primary headaches that occurs for 4 h or more in a day on 15 or more days per month for at least 3 months [1]. The treatment of CDH is a challenge for the physician. In general population, the prevalence of CDH ranges between 2.4 and 4.7 %. About 10–20 % patients in headache clinic in Europe are due to CDH, and 50–80 % in USA [2]. CDH may be due to chronic migraine (CM), chronic tension-type headache (CTTH), medication overuse headache, hemicrania continua and new daily persistent headache. Majority of CDH patients are due to migraine. Migraine affects 18 % of women and 6 % of men with the highest prevalence during 30–39 years of age [3]. Approximately 90 % of migraineurs have moderate to severe pain, 70 % have functional impairment, and 20 % require bed rest during an attack. About 2.5 % patients with episodic migraine convert to chronic migraine annually [4]. The aim of the therapy in CDH, therefore, is not to have complete remission but at least to revert back to episodic migraine. The quality of life is worse in CM compared to those with episodic migraine resulting in the absence from work, school, reduced productivity and more frequent visit to doctors which incur fourfold increase in annual health budget per patient [5]. Various drugs have been tried in migraine prophylaxis, which are effective in 50–60 % patients [6, 7]. These studies included both episodic and chronic migraine. The response to drug in CM is not as good as to episodic migraine [8]. Chronic daily headache patients are prone to develop medication overuse headache; therefore, the role of non-pharmacological treatment needs to be explored. Single pulse transcranial magnetic stimulation (sTMS) is now an approved therapy for acute migraine with aura in Europe and in USA [9]. High rate repetitive transcranial magnetic stimulation (rTMS) has been reported to be effective in reducing migraine frequency and severity at 1 month in an open labeled randomized controlled trial [10]. In this study, three sessions of 10 Hz rTMS was delivered on alternate day requiring three hospital visits in 5 days. There is paucity of report on efficacy of high rate rTMS in CDH. If the efficacy and safety of stimulation are objectively evaluated, it may help in optimizing the stimulation parameters. In this communication, we compare the efficacy and safety of single versus three sessions of high rate rTMS in the patients with CDH due to CM and CTTH.
Materials and methods
Study design
This is a randomized placebo controlled trial comparing the efficacy and safety of high rate rTMS in CDH due to CM and CTTH. This is a single center investigator initiated trial conducted in a tertiary care teaching hospital in India. The protocol was designed by JK and UK, and the study was approved by the Institute Ethics Committee (No. 2014-172-IP-80). The patients who consented for the study were included in this study.
Sample size calculation
The sample size was calculated considering the reduction in headache frequency by 70 % in the patients receiving three sessions and 35 % in the single session rTMS arm considering the previous report on three sessions of rTMS in migraine and placebo response. The type I error was considered as 0.05 and type II error 0.1 using Z test of proportion. The sample size in each arm was 45 with 90 % power of the test. It was a non-inferiority trial.
Inclusion criteria
Consecutive patients with CDH due to CM and long duration CTTH were recruited from the outpatient neurology service of our institute during 2014–2015. The diagnosis of CM was based on the presence of headache frequency 15 days or more per month lasting for more than 4 h if untreated for at least 3 months in the absence of secondary headache [11]. The CM and CTTH patients were further categorized into medication overuse headache (MOH). The diagnosis of CTTH was based on ICHD IIR criteria [11]. The diagnosis of MOH was based on ICHD III β criteria [12]. Mixed CDH was considered if the patients had tension-type headache with less than eight migraine attacks per month.
Exclusion criteria
Children below 15 years of age, pregnant mother, patients with secondary headache, pacemaker or any metallic implant, seizure, major psychiatric illness, structural brain disease, liver or kidney failure, organ transplantation, uncontrolled hypertension, uncontrolled diabetes or malignancy and those on immune suppressive therapy were excluded. The patients who refused consent were also excluded.
Clinical evaluation
A detailed clinical history was obtained and physical examination was done. The demographic information and duration of illness were noted. The patients were enquired about visual aura, duration of migraine attack, frequency per month, severity of associated symptoms and disability. Presence of migraine triggers and allodynia was assessed using a questionnaire [13, 14]. The severity of headache was graded on a 0–3 scale (0 none, 1 mild, 2 moderate, 3 severe) and also assessed on a 0–10 visual analog scale (VAS). The disability during the headache was assessed by a 0–4 scale (0 none; 1 mid, 2 moderate, 3 severe, 4 most severe needing bed rest). Presence of photophobia, phonophobia, nausea and vomiting, number of analgesic, and other abortive treatments were recorded. Hospital Anxiety and Depression Scale (HADS) was done in some patients.
Investigations
Blood counts, hemoglobin, erythrocyte sedimentation rate at 1 h, fasting blood sugar, blood urea nitrogen, serum creatinine, bilirubin, transaminase and lipid profile were done. Cranial CT scan was done and MRI or MR venography was done in selected patients in whom cerebral venous sinus thrombosis was suspected. Electrocardiogram and chest radiograph were also done.
Randomization and intervention
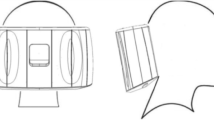
Patients were advised to stop prophylactic medication 15 days prior to the randomization. During this period, the patients were advised to maintain a headache diary, and to take paracetamol or a combination of ibuprofen and paracetamol if the headache was unbearable. The patients were randomized to group I (three sessions of high rate rTMS) or group II (one session true rTMS and two sessions sham stimulation). 10 Hz rTMS was delivered by a figure of eight coil on the left frontal region corresponding to the hot spot of abductor digiti minimi which is approximately 7 cm lateral from midline and 2 cm anterior to inter-aural line. Motor threshold was determined, and 70 % of motor threshold was used for stimulation. The patients received ten trains comprising 60 pulses in each train at 10 Hz with an inter train interval of 45 s. Each session of rTMS comprised 600 pulses which were delivered in 412.4 s. The rTMS sessions were given on alternate day between 10 a.m. and 2 p.m. The group II patients received sham stimulation on second and third session which was delivered using an identical looking figure of eight sham coil producing similar sound.
Outcome measures
The patients maintained a headache diary and they were evaluated on fifth day, 1, 2 and 3 months. The primary outcome was 50 % or more improvement in headache frequency at 1, 2 and 3 months and secondary outcome measures were reduction in severity, functional disability, number of abortive medication and side effects.
Statistical analysis
The baseline characteristics of group I and group II patients were compared using Chi-square for categorical and independent-t test for continuous variables. The improvement in headache frequency, severity, functional disability and number of abortive drugs at different time points within the group was evaluated using one way ANOVA employing Tukey post hoc correction. The primary outcome (>50 % improvement in frequency) was evaluated by Chi-square test. Per protocol and intention to treat analysis were done. Number of CDH patients converted to episodic headache after rTMS at different time points between group I and group II were evaluated using Chi-square test. The secondary outcomes within the groups and in between the groups were evaluated using one way ANOVA employing post hoc Tukey correction. The sub analysis was also done in the patients with CM, and CM with and without MOH to evaluate the effects of rTMS. The variable with a two tailed P value of less than 0.05 was considered significant. The statistical analysis was done using SPSS 16 version software and graphs were prepared by GraphPad prism 5.
Results
During the study period, 107 patients with CDH due to CM and long duration CTTH were screened, and nine of them were excluded due to refusal of consent in two, major psychiatric illness in two, and pregnancy, history of seizure, pituitary adenoma, chronic kidney disease and technical default in one patient each. This study is therefore based on 98 patients (Fig. 1). Their age ranged between 18 and 55 (median 32) years and 79 (80.6 %) were females. Six (6.1 %) patients had migraine with aura. The duration of illness ranged between 0.75 and 20 (median 7) years and the median duration of CDH was 12 (range 3–120) months. 82 (83.7 %) patients had CM, ten (10.3 %) long duration CTTH and six (6.1 %) both features of CM and CTTH.
Randomization
Fifty-two patients were randomized to group I (triple true rTMS) and 46 to group II (one true and two sham rTMS). The baseline demographic, duration of illness, migraine trigger and migraine characteristics were not significantly different between group I and group II patients (Table 1).
Follow up
Thirty nine patients in group I and 37 in group II adhered to treatment till 3 months. Ten patients (seven in group I and three in group II) were lost from follow up and 12 (six each in group) had to be shifted to other treatment modalities due to lack of satisfactory response.
Outcome
Primary outcome
In group I, the frequency of headache significantly reduced at 1 month (P < 0.001), 2 months (P < 0.001) and 3 months (P < 0.001) compared to the baseline. Similar reduction in headache frequency was also observed in group II patients. At 3 months, 81.6 % patients could be converted to episodic headache or complete remission; four (7.7 %) patients had complete remission and CDH converted to episodic headache in 29 (74.4 %) patients in group I, and these were seven (18.9 %) and 22 (59.2 %), respectively, in group II (Fig. 2). The reduction in frequency of headache and number of patients converted to episodic migraine was not significantly different between group I and group II. On per protocol and intention to treat analysis, the primary outcome was also not significantly different between group I and group II patients (Table 2).
Bar diagram shows improvement in frequency of headache in group I and group II patients. a, b The frequency of headache significantly reduced at 1, 2 and 3 months follow up compared to baseline in both group I and group II patients. c, d Number of patients who had >50 % reduction in frequency, converted to episodic headache, complete remission and remained as chronic daily headache at 1, 2 and 3 month follow up in group I (c) and group II which was not significantly different between the two groups
Secondary outcome measures
The duration and severity of headache, and number of abortive medication at 1, 2 and 3 months also improved significantly compared to baseline in both group I and group II (Supplementary Table 1). The improvement in these parameters, however, was not significantly different between group I and group II (Fig. 3). The details are presented in Supplementary Table 2.
Frequency curve showing various outcome parameters in group I and II at 1, 2 and 3 months follow up. The frequency, severity, visual analog scale (VAS) score, duration of headache and analgesic use although improved significantly compared to baseline in group 1 and 2, but these outcome parameters were not significantly different between the two groups
Side effects
None of the patients had severe adverse events needing termination of rTMS. Acceptable discomfort due to noise of rTMS, however, was reported by all.
Sub analysis
Out of 82 patients with CM, 48 were in group I and 34 in group II, and their baseline characteristics were not different. All the primary and secondary outcome parameters improved significantly in group I and group II. The frequency of headache at 2 months was significantly reduced in group I compared to group II on intention to treat analysis (62.5 vs 35.3 %; P = 0.01) and per protocol analysis (69.8 vs 35.3 %; P = 0.005).
In group I, 48 patients had CM and 17 of them had MOH. In group II out of 34 patients with CM, 19 had MOH. The reduction in frequency of headache at 1, 2 and 3 months between CM patients with and without MOH was not significantly different following single and triple stimulation (Supplementary Table 3).
Amongst the patients with CTTH (10) and mixed type of CDH (6), five had MOH. Three out of five patients in MOH and out of 11 without MOH had improvement in headache frequency following rTMS, and the difference is not statistically significant (P = 1.00).
Discussion
In the patients with CM and CTTH, both single and three sessions of high rate rTMS were effective in reducing frequency and severity of headache and number of abortive drugs till 3 months. 81.6 % of patients converted to episodic, but only 14.5 % patients achieved complete remission. On per protocol and intension to analysis, there was no difference in primary outcome between the two groups. This study reports the role of high rate rTMS in CM and CTTH including adequate sample size. There is only one study in which high rate rTMS was compared with sham stimulation in 18 patients with CM having severe depression. In this study, 32 trains of 10 Hz rTMS comprising 1600 pulses were delivered over the left dorsolateral prefrontal cortex and 23 sessions were given in 8 weeks. The severity and frequency of headache at 4 and 8 weeks after the rTMS did not improve compared to placebo. The protocol used in this study was extrapolated from the rTMS protocol for depression [15]. There are only few randomized controlled trials of rTMS in migraine prophylaxis. In a randomized placebo controlled trail, 10 Hz rTMS over left dorsolateral frontal cortex corresponding to the hot spot of abductor digiti minimi resulted in significant reduction in frequency and severity of headache and number of analgesic intake at 1 month in the rTMS group compared to the placebo. These effects were maximum at 15 days after the rTMS. At 1 month, 78.7 % had more than 50 % reduction in frequency in the rTMS group compared to 33.3 % in sham group. The VAS score also improved (>50 %) in 76.6 % in the rTMS group compared to 27.1 % in the sham group [10]. Similar improvement has also been reported in other studies [16, 17]. In one study, six patients received 12 sessions of 400 pulses delivered at 20 Hz at 90 % of motor threshold and five patients received sham stimulation. Headache frequency, headache index and abortive pill intake reduced significantly from the baseline and the benefit lasted for 2 months in the rTMS group [17]. In another study, low-frequency rTMS in 27 migraine patients although resulted in improvement of headache frequency from the baseline but the difference was not significant when compared with the sham stimulation group [18]. The variation in the results in different studies may be due to different patient population, inadequate sample size and difference in rTMS protocol. The stimulation rate, number of pulses, number of session and site of stimulation are different in different studies [15–18]. In this study, we have used the same protocol which was used in our earlier study [10, 17].
Left dorsolateral frontal cortex has an important role in pain relief. Capsaicin induced pain on dorsum of hands in the volunteers was relieved by stimulating left dorsolateral frontal cortex, whereas this effect was not observed by right side stimulation [19]. Electrical cathodal stimulation of supra orbital region, occipital region and cerebellum has also been reported effective in migraine [20–22].
The exact mechanism of rTMS in preventing migraine is not well understood. Low intensity TMS probably stimulates low-threshold inhibitory interneurons, whereas higher intensities excite projection neurons. Depending on the frequency of rTMS, it can induce either long-term potentiation or long-term depression; high frequency rTMS (≥5 Hz) increases excitability, whereas slow rTMS (≤1 Hz) decreases it [23]. The excitation and impaired habituation of sensory neurons in migraineurs have been demonstrated using visual, somatosensory and event related potentials [24–26]. Improvement in impaired habituation and reduction in neuronal excitability have been observed in visual evoked potential following rTMS [27]. These biological phenomena may also be altered by amitriptyline, beta blocker and antiepileptic drug, and are also found effective in migraine prophylaxis in randomized controlled trials. High rate rTMS in migraine has been reported to increase in endorphin release that correlated with clinical improvement suggesting the role of endorphin in migraine [28]. Endorphin is closely linked to hypothalamus and hypothalamic abnormalities have been reported in PET and functional MRI studies [29]. Following rTMS increase in hippocampal dopamine, reduction in 11C raclopride and change in glutamate/glutamine has been reported [30–32]. These changes result in headache relief for variable duration.
The aim of treatment of CDH is to convert it to episodic headache if not total remission. In an epidemiological study, 26 % patients with CM remitted to episodic migraine annually. Patients who had headache remission had lower headache frequency compared with the patients with persistent CM [33]. Preventive medicine alone or in combination also reduces more than 50 % headache frequency in about 60 % patients at the end of 12 weeks [34]. In a pooled analysis of double blind randomized controlled trials, topiramate was found to be superior to placebo resulting in at least 50 % reduction in migraine parameters in 46.3 % patients [35]. Following rTMS, 62.5 % patients had more than 50 % reduction in headache frequency which is comparable to the pharmacological treatment. Conversion to episodic headache in 80.3 % of our patients in turn reduced the frequency of MOH. Other non-pharmacological treatment like acupuncture has been reported to reduce headache days by 10–12 in a randomized controlled trial [36].
Strength and weakness
This is the first study on the role of three versus single session of rTMS in the patients with CM and CTTH, using well defined inclusion and evaluation criteria having adequate sample size. This study is limited by lack of placebo arm and double blind design. We did not have a placebo arm because of ethical issues and previous report of efficacy of three sessions of rTMS in migraine prophylaxis [10]. Our aim was to evaluate the efficacy of three versus single session of rTMS, and if single session is effective, the protocol will be more acceptable to the patients. Our patients were blinded about the stimulation type; however, the examiners were not. This is unlikely to influence our results as outcome measure was based on the headache diary maintained by the patients.
It can be concluded from this study that single session of 10 Hz rTMS over left frontal cortex is equally effective to three sessions in CM and CTTH. Further studies are needed to evaluate the effect of rTMS in combination with antimigraine drugs in the patients with CM.
References
Silberstein SD (1993) Tension-type and chronic daily headache. Neurology 43(9):1644–1649
Bigal ME, Sheftell FD (2006) Chronic daily headache and its subtypes. Continuum-Lifelong Learn Neurol 12(6):133–152
Lipton RB, Bigal ME, Diamond M, Freitag F, Reed ML, Stewart WF, AMPP Advisory Group (2007) Migraine prevalence, disease burden, and the need for preventive therapy. Neurology 68(5):343–349
Natoli JL, Manack A, Dean B, Butler Q, Turkel CC, Stovner L, Lipton RB (2010) Global prevalence of chronic migraine: a systematic review. Cephalalgia 30(5):599–609
Munakata J, Hazard E, Serrano D, Klingman D, Rupnow MF, Tierce J, Reed M, Lipton RB (2009) Economic burden of transformed migraine: results from the American Migraine Prevalence and Prevention (AMPP) Study. Headache 49(4):498–508
Kalita J, Bhoi SK, Misra UK (2013) Amitriptyline vs divalproate in migraine prophylaxis: a randomized controlled trial. Acta Neurol Scand 128(1):65–72
Jackson JL, Cogbill E, Santana-Davila R, Eldredge C, Collier W, Gradall A, Sehgal N, Kuester J (2015) A comparative effectiveness meta-analysis of drugs for the prophylaxis of migraine headache. PLoS One 10(7):e0130733
Mathew NT, Jaffri SF (2009) A double-blind comparison of onabotulinumtoxina (BOTOX) and topiramate (TOPAMAX) for the prophylactic treatment of chronic migraine: a pilot study. Headache 49(10):1466–1478
Bhola R, Kinsella E, Giffin N, Lipscombe S, Ahmed F, Weatherall M, Goadsby PJ (2015) Single-pulse transcranial magnetic stimulation (sTMS) for the acute treatment of migraine: evaluation of outcome data for the UK post market pilot program. J Headache Pain 16:535
Misra UK, Kalita J, Bhoi SK (2013) High-rate repetitive transcranial magnetic stimulation in migraine prophylaxis: a randomized, placebo-controlled study. J Neurol 260(11):2793–2801
Headache Classification Subcommittee of the International Headache Society (IHS) (2005) The International Classification of Headache Disorders. 2nd edition. 1st revision. Cephalalgia 25:460–465
Headache Classification Committee of the International Headache Society (IHS) (2013) The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia 33(9):629–808
Kalita J, Yadav RK, Misra UK (2009) A comparison of migraine patients with and without allodynic symptoms. Clin J Pain 25(8):696–708
Yadav RK, Kalita J, Misra UK (2010) A study of triggers of migraine in India. Pain Med 11(1):44–47
Conforto AB, Amaro E Jr, Gonçalves AL, Mercante JP, Guendler VZ, Ferreira JR, Kirschner CC, Peres MF (2014) Randomized, proof-of-principle clinical trial of active transcranial magnetic stimulation in chronic migraine. Cephalalgia 34(6):464–472
Misra UK, Kalita J, Bhoi SK (2012) High frequency repetitive transcranial magnetic stimulation (rTMS) is effective in migraine prophylaxis: an open labeled study. Neurol Res 34(6):547–551
Brighina F, Piazza A, Vitello G, Aloisio A, Palermo A, Daniele O, Fierro B (2004) rTMS of the prefrontal cortex in the treatment of chronic migraine: a pilot study. J Neurol Sci 227(1):67–71
Teepker M, Hotzel J, Timmesfeld N, Reis J, Mylius V, Haag A, Oertel WH, Rosenow F, Schepelmann K (2010) Low-frequency rTMS of the vertex in the prophylactic treatment of migraine. Cephalalgia 30(2):137–144
Brighina F, de Tommaso M, Giglia F, Scalia S, Cosentino G, Puma A, Panetta M, Giglia G, Fierro B (2011) Modulation of pain perception by transcranial magnetic stimulation of left prefrontal cortex. J Headache Pain 12(2):185–191
Meng FG, Zhang JG, Schoenen J, Vandersmissen B, Herroelen L, Vandenheede M, Gerard P, Magis D (2013) Migraine prevention with a supraorbital transcutaneous stimulator: a randomized controlled trial. Neurology 81(12):1102
Brighina F, Palermo A, Panetta ML, Daniele O, Aloisio A, Cosentino G, Fierro B (2009) Reduced cerebellar inhibition in migraine with aura: a TMS study. Cerebellum 8(3):260–266
Fumal A, Bohotin V, Vandenheede M, Schoenen J (2003) Transcranial magnetic stimulation in migraine: a review of facts and controversies. Acta Neurol Belg 103(3):144–154
Klein MM, Treister R, Raij T, Pascual-Leone A, Park L, Nurmikko T et al (2015) Transcranial magnetic stimulation of the brain: guidelines for pain treatment research. Pain 156(9):1601–1614
Coppola G, Currà A, Di Lorenzo C, Parisi V, Gorini M, Sava SL, Schoenen J, Pierelli F (2010) Abnormal cortical responses to somatosensory stimulation in medication-overuse headache. BMC Neurol 10:126
Kropp P, Gerber WD (1993) Is increased amplitude of contingent negative variation in migraine due to cortical hyperactivity or to reduced habituation? Cephalalgia 13(1):37–41
Kalita J, Bhoi SK, Misra UK (2014) Is lack of habituation of evoked potential a biological marker of migraine? Clin J Pain 30(8):724–729
Fumal A, Coppola G, Bohotin V, Gérardy PY, Seidel L, Donneau AF et al (2006) Induction of long-lasting changes of visual cortex excitability by five daily sessions of repetitive transcranial magnetic stimulation (rTMS) in healthy volunteers and migraine patients. Cephalalgia 26(2):143–149
Misra UK, Kalita J, Tripathi GM, Bhoi SK (2013) Is β endorphin related to migraine headache and its relief? Cephalalgia 33(5):316–322
Maniyar FH, Sprenger T, Monteith T, Schankin C, Goadsby PJ (2014) Brain activation in the premonitory phase of nitroglycerin—triggered migraine attacks. Brain 137(1):232–241
Czéh B, Welt T, Fischer AK, Erhardt A, Schmitt W, Müller MB, Toschi N, Fuchs E, Keck ME (2002) Chronic psychosocial stress and concomitant repetitive transcranial magnetic stimulation: effects on stress hormone levels and adult hippocampal neurogenesis. Biol Psychiatry 52(11):1057–1065
Cho SS, Strafella AP (2009) rTMS of the left dorsolateral prefrontal cortex modulates dopamine release in the ipsilateral anterior cingulate cortex and orbitofrontal cortex. PLoS One 4(8):e6725
Michael N, Gösling M, Reutemann M, Kersting A, Heindel W, Arolt V, Pfleiderer B (2003) Metabolic changes after repetitive transcranial magnetic stimulation (rTMS) of the left prefrontal cortex: a sham-controlled proton magnetic resonance spectroscopy (1H MRS) study of healthy brain. Eur J Neurosci 17(11):2462–2468
Manack A, Buse DC, Serrano D, Turkel CC, Lipton RB (2011) Rates, predictors, and consequences of remission from chronic migraine to episodic migraine. Neurology 76(8):711–718
Silberstein SD, Dodick DW, Lindblad AS, Holroyd K, Harrington M, Mathew NT et al (2012) Randomized, placebo controlled trial of propranolol added to topiramate in chronic migraine. Neurology 78(27):976–984
Bussone G, Diener HC, Pfeil J, Schwalen S (2005) Topiramate 100 mg/day in migraine prevention: a pooled analysis of double-blind randomised controlled trials. Int J Clin Pract 59(8):961–968
Yang CP, Chang MH, Li TC, Hsieh CL, Hwang KL, Chang HH (2013) Predicting prognostic factors in a randomized controlled trial of acupuncture versus topiramate treatment in patients with chronic migraine. Clin J Pain 29(11):982–987
Acknowledgments
We thank Mr. Rakesh Kumar Nigam and Mr. Shakti Kumar for secretarial help.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
There is no conflict of interest to declare.
Ethical approval
This study was approved by Institutional Ethics Committee, SGPGIMS, Lucknow, India.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kalita, J., Laskar, S., Bhoi, S.K. et al. Efficacy of single versus three sessions of high rate repetitive transcranial magnetic stimulation in chronic migraine and tension-type headache. J Neurol 263, 2238–2246 (2016). https://doi.org/10.1007/s00415-016-8257-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-016-8257-2