Abstract
To determine the prevalence of depression, to identify correlated factors for depression, and to explore the impact on the progression or survival of amyotrophic lateral sclerosis (ALS) by depression in a Chinese population. A total of 166 ALS patients were recruited. Diagnosis of depression disorders and the severity of depression were established by using the fourth diagnostic and statistical manual of mental disorders, Hamilton Depression Rating Scale-24 items (HDRS-24) and Beck Depression Inventory (BDI). Major depression was found in 15 patients (9.6 %). The multiple regression analysis showed that a lower ALS Functional Rating Scale-Revised (ALSFRS-R) score was correlated with increasing HDRS scores and BDI scores (P = 0.018 and P = 0.012). No significant difference in the median survival time between ALS patients with and without depression was revealed by Kaplan–Meier analysis (log-rank P = 0.282). Cox hazard model showed that the presence of depression in ALS was unrelated to the survival, while the severity of depression in ALS was correlated with the survival. The presence and severity of depression in ALS did not correlate with the progression of ALS. Major depression in ALS is uncommon. Depression evaluation should be given to ALS patients, especially those with lower ALSFRS-R score. The severity of depression may be associated with the survival; however, depression does not worse the progression of ALS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Amyotrophic lateral sclerosis (ALS), a devastating disease characterized by progressive loss of motor neurons, leading to weakness of bulbar, limb, thoracic and abdominal muscles, is the third common neurodegenerative disease of aging population [1]. With a mean survival about 3.5 years [2], the only evidence-proved effective drug for ALS is riluzole, which may at best prolong survival for up to 6 months [3]. Moreover, numerous non-motor manifestations have been observed in ALS, including cognitive dysfunction, behavioral impairments, and mood disorders [4, 5]. However, the findings of the prevalence of depression, the predisposing factors for depression and the correlation between depression and survival of ALS in previous studies are inconsistent [5–8]. It is hard to state that mood disorders are not really common in ALS patients, as it mainly depends on the different types of assessment that have been used [9]. The prevalence of depression in ALS patients has been reported to be as high as 48 % [10] to 75 % [11] and as low as 9.8 % [12, 13]. An association between depression and physical impairment in ALS has been reported by some studies [6, 14, 15]. However, some studies reported a lack of a correlation between depression and physical impairment [7, 10, 16–18]. Few studies reported the association between depression and survival in ALS [8, 19].
Overall, current evidence on depression in ALS patients is greatly limited to draw a conclusion regarding to the study methods, sample sizes, sample composition and using various assessments for depression. The early and accurate identification of depressive symptoms in ALS can lead to diagnostic awareness and effective therapies to improve the quality of life in both ALS patients and their caregivers. In this context, this study was designed in a large cohort of ALS patients to (1) determine the prevalence of depressive disorder (meeting the fourth diagnostic and statistical manual of mental disorders, DSM-IV) [20] and depressive symptom (that exists but not yet enough to meet the DSM-IV criteria); (2) identify possible predisposing and protective factors associated with depression; (3) determine whether the occurrence and severity of depression associated with the survival or disease progression of ALS.
Methods
Participants
Patients with diagnosis of definite or probable ALS (El Escorial revised criteria) [21] from a large, regional referral ALS clinic of Southwest China, between August 2012 and March 2014, participated in the study. The demographic information was collected and the following measures of detailed neurological examination and psychological morbidity were administered on the same day. The approval for the study was obtained from the Ethics Committee of West China Hospital of Sichuan University. Informed written consent was obtained from all participants prior to being recruited.
The diagnostic delay was defined as the month interval between the date of onset and the date of diagnosis. ALS Functional Rating Scale-Revised (ALSFRS-R) [22] was used to assess bulbar (ALSFRS-R-B), limb (ALSFRS-R-L) and respiratory function (ALSFRS-R-R). Scores ranged from 0 (unable to perform the task) to 4 (no impairment) for each item, resulting in total scores ranging from 0 (the worst) to 48 (the best). Manual Muscle Testing (MMT) is a scored neurologic examination derived from the Medical Research Council scale [23]. The scale is numerical based on the examination of 34 muscles. Each muscle is scored from 0 to 5, with 0 representing complete paralysis and 5 representing normal strength. The final MMT score for each subject is the mean of the scores of all 34 muscles. The mini–mental state examination (MMSE) is used for screening the global cognition in ALS patients.
Diagnosis of depression disorders was established by using the DSM-IV by a trained neurologist. The severity of depression was evaluated using Hamilton Depression Rating Scale—24 items (HDRS-24), with a score of <8 indicating no depression, a score from 8 to 20 corresponding to mild depression, a score from 20 to 35 corresponding to moderate depression, and a score of >35 corresponding to severe depression [24]. For the sake of completeness evaluating depression in ALS, a self-administered scale named Beck Depression Inventory (BDI) was also used. It has thirteen items with a total score less than 4 indicating no depression, 5–13 corresponding to mild depression, 14–20 corresponding to moderate depression, and a total score more than 21 indicated severe depression [25].
All enrolled participants were followed every 3 months by face-to-face interviews or phone calls until the end of the study. The ALSFRS-R score was evaluated during follow-up. Progression rate was assessed by the changes of ALSFRS-R per month (△ALSFRS-R/m) (formula: (ALSFRS-R1 score at baseline—ALSFRS-R2 at the last visit)/month intervals between the two assessments). Survival time was defined as the interval time between the date of onset and the date of death. Tracheotomy was taken as equivalent to death.
Data analysis
All continuous variables presented as mean ± standard deviation, and all categorical variables presented as numbers or percentages. Spearman’s correlations were used to analyze the relationship between depression and clinical features of ALS. Spearman rank correlation coefficient (rs) of ≥0.8 was considered as a very strong correlation, r s = 0.60–0.79 was considered as a strong correlation, r s = 0.4–0.59 was considered as a moderate correlation, r s = 0.20–0.39 was considered as a weak correlation, and r s ≤ 0.19 was considered as a negligible correlation [26]. Comparison of categorical variables, a Chi-square test was performed. The multiple regression analysis was employed to reveal the factors related to depression at study baseline. Depression score was served as dependent variable. Kaplan–Meier curves and log-rank tests were used to compare the survival time between the groups (with and without depression). Cox proportional hazards regression model was hired to determine whether the presence and severity of depression contribute to the survival of ALS independently. In Cox proportional hazards regression model, the other parameters included age of onset, onset region, diagnostic delay, body mass index (BMI), MMT scores, ALSFRS-R scores, and MMSE scores, while the survival status set as dependent variable. The association between the present or the severity of depression and the progression of ALS was conducted by multivariate regression analysis. All statistical tests analyzed by SPSS 17.0 were two-tailed, with statistical significance set as P < 0.05.
Results
A total of 234 patients with probable or definite ALS were identified as potentially eligible participants. Among 234 patients, four patients with frontotemporal dementia, 28 patients with severe dysarthria, and 21 patients with severe hand weakness were excluded due to incomplete assessment. Fifteen patients who refused to participate were also excluded. Finally, a total of 166 ALS patients were included in the analyses. The demographic and disease-specific factors of the enrolled patients and the excluded patients are shown in Table 1. No significant differences in demographic features were observed between the enrolled patients and the excluded patients (Table 1). The age of enrolled patients ranged from 27 to 81 years, with 12.7 % under age 40 and 12.0 % over 70. A total of 13.9 % of the enrolled patients had a graduate degree, 39.8 % of the enrolled patients had received less than high school education. Six patients had a family history of ALS.
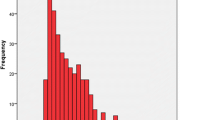
Fifteen patients (9.0 %) at the baseline were diagnosed to have major depression episode (DSM-IV). Based on HDRS-24, 88 patients (53.0 %) had no depression, 62 patients (37.3 %) had mild depression, 12 patients (7.2 %) had moderate depression, and 4 patients (2.4 %) had severe depression. The latter two groups together (9.6 %) are consistent with the presence of a clinically diagnosed major depressive disorder. A total of 128 patients completed the BDI scale. According to the score, 61 patients (47.7 %) had no depression, 49 patients (38.3 %) had mild depression, and 18 patients (14.0 %) had moderate or severe depression. The ALSFRS-R total score and ALSFRS-R-R score were significantly decreased with the severity of depression increasing (Table 2). There were no statistically differences in the general features including sex, age, age of onset, BMI, education level, marriage status, concomitant diseases, residence, disease duration and diagnostic delay, and disease-specific features including onset body region, MMT and MMSE scores among the three patients groups regarding to the severity of depression (Table 2).
In the Spearman analysis, the score of HDRS-24 was negatively weakly correlated with ALSFRS-R, ALSFRS-R-L and ALSFRS-R-R scores (r s = −0.272, −0.192 and −0.168, respectively), but not correlated with the ALSFRS-R-B score (r s = −0.087), indicating that patients with severe depression had lower scores of ALSFRS-R, ALSFRS-R-L and ALSFRS-R-R. The BDI score also was negatively correlated with ALSFRS-R (r s = −0.202, P = 0.022). The multiple regression analysis showed that a lower ALSFRS-R score was correlated with increasing HDRS scores and BDI scores (P = 0.018, 95 %CI −0.740 to −0.072 and P = 0.012, 95 %CI −0.693 to −0.090), whereas, covariates including age of onset, onset body region, sex, disease duration, diagnostic delay, BMI, educational level, MMT and MMSE scores were not associated with the increasing depression.
At the end of the study, 1 patient received tracheotomy, 22 patients departed, 18 of which died from respiratory failure, 3 from difficulty in swallowing and 1 from intracranial hematoma after falling down from stairs. The average follow-up duration between baseline and the last visit was 10.2 ± 5.0 months. The monthly decline of ALSFRS-R was 0.8 ± 0.7. No significant difference in the median survival times between ALS patients with and without depression was revealed by Kaplan–Meier analysis (24.0 vs. 20.5 months, log-rank P = 0.282, Fig. 1). Cox proportional hazard model showed that the presence of depression was unrelated to the survival in ALS (OR = 3.673, 95 % CI = 0.747–18.064, P = 0.109), while ALSFRS-R scores and diagnostic delay were statistically associated with the survival in ALS (OR: 0.752, 95 % CI 0.632–0.894, P = 0.001 and OR: 0.065, 95 % CI 0.013–0.322, P = 0.001, respectively) (Table 3). In addition, Cox proportional hazard model revealed that the severity of depression explored by HDRS and BDI was associated with the survival in ALS (OR = 2.097, 95 % CI = 1.032–4.261, P = 0.041 and OR = 3.108, 95 % CI = 1.464 to 6.600, P = 0.003) (Table 4). After adjusting for age of onset and onset body region, multivariate regression analyses revealed that the presence of depression and the severity of depression were not correlated with the disease progression of ALS (P > 0.05).
Discussion
To the best of our knowledge, this is the largest study to explore the point prevalence of depression and its association with survival and disease progression of ALS in a Chinese population.
In accordance with majority of previous reports [8, 18, 27, 28], approximately 10 % of patients with ALS had major depression diagnosed by means of DSM-IV structured clinical interview, which was slightly higher than that in the general population (4–5 %) [29], yet lower than other relentless diseases such as multiple sclerosis (17–46 %) [30, 31] and carcinoma [32]. Although, ALS was a devastating disease, a noteworthy observation in the current study was that clinically significant depression was neither as prevalent nor as severe as might be expected, which was consistent with an evaluation of 28 studies regarding depression in ALS [33]. It was hard for researchers to figure out whether depression was caused by somatic changes or reactive changes by the diagnosis of ALS [15]. In our study, all participants were non-disclosure of the diagnosis of ALS at the register, which might give some clue that somatic changes were involved more in the occurrence of depression in ALS. Based on the HDRS-24, 47 % of ALS patients had depressive symptom, and according to BDI, 52 % of ALS patients had depressive symptom. The greatly varied differences in the prevalence of depression among the published data (ranged from 9.8 to 75 %), in our view, are particularly attributed to the use of different diagnostic instruments [33, 34].
In the current study, Spearman correlation analysis and the multiple regression analysis revealed that depression was associated with the total score of ALSFRS-R, which was inconsistent with some recent studies which observed no correlation between depression and physical impairment [7, 10, 16, 17]. The correlation between depression and physical impairment was still controversial. Moreover, ALSFRS-R-L and ALSFRS-R-R scores were significantly correlated with depression. The possible explanations for depression related to respiratory dysfunction may be due to physical uncomfort, or increased ALS patients’ awareness of the limited lifespan, or the gradual approaches of death resulting from respiratory insufficiency. Currently available evidence does not allow researchers to differentiate the possible explanations. Further studies with detailed data of patients’ oxygenation status and an exploration of patients’ mood status and thoughts regarding to death approaches were needed.
The relationship between depression and onset body region, sex, diagnostic delay, and bulbar involvement was controversial [5, 6, 14, 35]. Our study found lack of correlation between depression in ALS and other factors such as age of onset, onset body region, sex, disease duration, diagnostic delay, education level, MMT score and MMSE score. Therefore, we recommend that depression should be evaluated in ALS patients with lower ALSFRS-R score, especially in patients with lower ALSFRS-R-L and ALSFRS-R-R scores.
In our study, the presence of depression at baseline was unrelated to the survival or disease progression, which differed ALS from other orphan diseases like carcinoma [27], but the severity of depression at baseline was associated with the survival. These results should be cautiously explained. One study proposed that the depression may be related to ALS progression [36]. The other study found that there was no significant difference in the survival and progression between ALS patients with and without depression [37]. In the limited number of ALS researches regarding depression in a longitudinal way, assessments did not find increased rates of depression over the course of the disease, or in the 3 months prior to death [8]. Our current study was only able to indicate correlation between the severity of depression and survival since mood status was not measured at follow-up visiting. The relationship between depression and survival should be verified in further prospective studies.
The currently available guidelines for treating depression in ALS patients has no or very limited space [38, 39]. According to our results, it’s not necessary to administer psychological and pharmacological intervention to all patients as soon as one was diagnosed with ALS. However, investigation on depression should be given routinely and individually in different stages of ALS, and therapy based on the diagnosis of depression in ALS if necessary.
These findings should be interpreted in light of several study limitations. First of all, previous study recommended to removing physical items when considering a diagnosis of depression in patients with ALS [15]. But, our study didn’t remove the physical items from the scale, which may overestimate the presence of depression in ALS patients. Second, the current study focused on the point prevalence of depression at baseline and its correlation with ALS survival, with no data of mood status or its changes over the course of the disease, although available evidence indicated that depression rate in ALS was not increased when death approaches [8]. This study only used MMSE scale to evaluate the global cognitive deficit. Due to the complexity of cognition, a hierarchical approach might be required using a special screen created for the evaluation of ALS patients or a combination of several cognitive questionnaires. For example, Edinburgh Cognitive And Behavioral ALS Screen is specially designed for ALS [40]. It is an effective within-clinic assessment for ALS that determines the presence, severity and type of cognitive and/or behavioral changes. Sample bias may be concerned in our study, since all the participants were recruited from a single ALS center, which was likely to offer more support and practical assistance to ALS patients thus having impact on mood status than other sites of medical care.
Conclusions
Major depression in ALS is uncommon. Depression evaluation should be given to ALS patients, especially those with lower ALSFRS-R score. The presence of depression in ALS was unrelated to the survival, while the severity of depression may be associated with the survival. Depression does not worse the progression of ALS.
References
Strong MJ (2001) Progress in clinical neurosciences: the evidence for ALS as a multisystems disorder of limited phenotypic expression. Can J Neurol Sci 28(4):283–298
Rowland LP, Shneider NA (2001) Amyotrophic lateral sclerosis. N Engl J Med 344(22):1688–1700
Lacomblez L, Bensimon G, Leigh PN, Guillet P, Meininger V (1996) Dose-ranging study of riluzole in amyotrophic lateral sclerosis. Amyotrophic Lateral Sclerosis/Riluzole Study Group II. Lancet 347(9013):1425–1431
Phukan J, Pender NP, Hardiman O (2007) Cognitive impairment in amyotrophic lateral sclerosis. Lancet Neurol 6(11):994–1003
Atassi N, Cook A, Pineda CM, Yerramilli-Rao P, Pulley D, Cudkowicz M (2011) Depression in amyotrophic lateral sclerosis. Amyotroph Lateral Scler. 12(2):109–112
Oh H, Sin MK, Schepp KG, Choi-Kwon S (2012) Depressive symptoms and functional impairment among amyotrophic lateral sclerosis patients in South Korea. Rehabil Nurs 37(3):136–144
Olsson Ozanne AG, Strang S, Persson LI (2011) Quality of life, anxiety and depression in ALS patients and their next of kin. J Clin Nurs 20(1–2):283–291
Rabkin JG, Albert SM, Del Bene ML, O’Sullivan I, Tider T, Rowland LP, Mitsumoto H (2005) Prevalence of depressive disorders and change over time in late-stage ALS. Neurology 65(1):62–67
Pagnini F, Manzoni GM, Tagliaferri A, Gibbons CJ (2015) Depression and disease progression in amyotrophic lateral sclerosis: a comprehensive meta-regression analysis. J Health Psychol 20(8):1107–1128
McElhiney MC, Rabkin JG, Gordon PH, Goetz R, Mitsumoto H (2009) Prevalence of fatigue and depression in ALS patients and change over time. J Neurol Neurosurg Psychiatry 80(10):1146–1149
Bocker FM, Seibold I, Neundorfer B (1990) Disability in everyday tasks and subjective status of patients with advanced amyotrophic lateral sclerosis. Fortschr Neurol Psychiatr 58(6):224–236
Ferentinos P, Paparrigopoulos T, Rentzos M, Zouvelou V, Alexakis T, Evdokimidis I (2011) Prevalence of major depression in ALS: comparison of a semi-structured interview and four self-report measures. Amyotroph Lateral Scler 12(4):297–302
Trail M, Nelson ND, Van JN, Appel SH, Lai EC (2003) A study comparing patients with amyotrophic lateral sclerosis and their caregivers on measures of quality of life, depression, and their attitudes toward treatment options. J Neurol Sci 209(1–2):79–85
Hillemacher T, Grassel E, Tigges S, Bleich S, Neundorfer B, Kornhuber J, Hecht MJ (2004) Depression and bulbar involvement in amyotrophic lateral sclerosis. Amyotroph Lateral Scler Other Motor Neuron Disord 5(4):245–249
Körner S, Kollewe K, Abdulla S, Zapf A, Dengler R, Petri S (2015) Interaction of physical function, quality of life and depression in amyotrophic lateral sclerosis: characterization of a large patient cohort. BMC Neurol 15:84
Grehl T, Rupp M, Budde P, Tegenthoff M, Fangerau H (2011) Depression and QOL in patients with ALS: how do self-ratings and ratings by relatives differ? Qual Life Res 20(4):569–574
Lule D, Hacker S, Ludolph A, Birbaumer N, Kubler A (2008) Depression and quality of life in patients with amyotrophic lateral sclerosis. Dtsch Arztebl Int 105(23):397–403
Rabkin JG, Wagner GJ, Del Bene M (2000) Resilience and distress among amyotrophic lateral sclerosis patients and caregivers. Psychosom Med 62(2):271–279
McDonald ER, Wiedenfeld SA, Hillel A, Carpenter CL, Walter RA (1994) Survival in amyotrophic lateral sclerosis. The role of psychological factors, Arch Neurol 51(1):17–23
Zimmerman M, McGlinchey JB, Young D, Chelminski I (2006) Diagnosing major depressive disorder I: a psychometric evaluation of the DSM-IV symptom criteria. J Nerv Ment Dis 194(3):158–163
Brooks BR, Miller RG, Swash M, Munsat TL, World Federation Neurology Res G (2000) El Escorial revisited: Revised criteria for the diagnosis of amyotrophic lateral sclerosis. Amyotrophic Lateral Scler Other Motor Neuron Dis 1(5):293–299
Cedarbaum JM, Stambler N, Malta E, Fuller C, Hilt D, Thurmond B, Nakanishi A (1999) The ALSFRS-R: a revised ALS functional rating scale that incorporates assessments of respiratory function. BDNF ALS Study Group (Phase III). J Neurol Sci 169(1–2):13–21
Group GLAS (2003) A comparison of muscle strength testing techniques in amyotrophic lateral sclerosis. Neurology 61(11):1503–1507
Moberg PJ, Lazarus LW, Mesholam RI, Bilker W, Chuy IL, Neyman I, Markvart V (2001) Comparison of the standard and structured interview guide for the Hamilton Depression Rating Scale in depressed geriatric inpatients. Am J Geriatr Psychiatry 9(1):35–40
Beck AT, Rial WY, Rickels K (1974) Short form of depression inventory: cross-validation. Psychol Rep 34(3):1184–1186
Swinscow TD (1976) Statistics at square one: XVIII-Correlation. Br Med J 2(6037):680–681
Ganzini L, Johnston WS, Hoffman WF (1999) Correlates of suffering in amyotrophic lateral sclerosis. Neurology 52(7):1434–1440
Kurt A, Nijboer F, Matuz T, Kubler A (2007) Depression and anxiety in individuals with amyotrophic lateral sclerosis: epidemiology and management. CNS Drugs 21(4):279–291
Narrow WE, Rae DS, Robins LN, Regier DA (2002) Revised prevalence estimates of mental disorders in the United States: using a clinical significance criterion to reconcile 2 surveys’ estimates. Arch Gen Psychiatry 59(2):115–123
Feinstein A, Feinstein K (2001) Depression associated with multiple sclerosis’. Looking beyond diagnosis to symptom expression. J Affect Disord 66(2–3):193–198
Galeazzi GM, Ferrari S, Giaroli G, Mackinnon A, Merelli E, Motti L, Rigatelli M (2005) Psychiatric disorders and depression in multiple sclerosis outpatients: impact of disability and interferon beta therapy. Neurol Sci 26(4):255–262
Frick E, Tyroller M, Panzer M (2007) Anxiety, depression and quality of life of cancer patients undergoing radiation therapy: a cross-sectional study in a community hospital outpatient centre. Eur J Cancer Care (Engl) 16(2):130–136
Averill AJ, Kasarskis EJ, Segerstrom SC (2007) Psychological health in patients with amyotrophic lateral sclerosis. Amyotroph Lateral Scler 8(4):243–254
McLeod JE, Clarke DM (2007) A review of psychosocial aspects of motor neurone disease. J Neurol Sci 258(1–2):4–10
Caga J, Ramsey E, Hogden A, Mioshi E, Kiernan MC (2015) A longer diagnostic interval is a risk for depression in amyotrophic lateral sclerosis. Palliat Support Care 13(4):1019–1024
Pisa FE, Logroscino G, Casetta A, Cecotti L, Verriello L, Bratina A, Sartori A, Lazzarino de Lorenzo L, Eleopra R, Barbone R (2015) The Use of Antidepressant Medication before and after the Diagnosis of Amyotrophic Lateral Sclerosis: a population-based cohort study. Neuroepidemiology 44(2):91–98
Korner S, Kollewe K, Ilsemann J, Muller-Heine A, Dengler R, Krampfl K, Petri S (2013) Prevalence and prognostic impact of comorbidities in amyotrophic lateral sclerosis. Eur J Neurol 20(4):647–654
Miller RG, Jackson CE, Kasarskis EJ, England JD, Forshew D, Johnston W, Kalra S, Katz JS, Mitsumoto H, Rosenfeld J, Shoesmith C, Strong MJ, Woolley SC (2009) Practice parameter update: the care of the patient with amyotrophic lateral sclerosis: drug, nutritional, and respiratory therapies (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 73(15):1218–1226
Andersen PM, Abrahams S, Borasio GD, de Carvalho M, Chio A, Van Damme P, Hardiman O, Kollewe K, Morrison KE, Petri S, Pradat PF, Silani V, Tomik B, Wasner M, Weber M (2012) EFNS guidelines on the clinical management of amyotrophic lateral sclerosis (MALS)—revised report of an EFNS task force. Eur J Neurol 19(3):360–375
Abrahams S, Newton J, Niven E, Foley J, Bak TH (2014) Screening for cognition and behaviour changes in ALS. Amyotrophic Lateral Scler Frontotemporal Degen 15(1–2):9–14
Acknowledgments
The authors thank the patients for their participation in the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declared no conflict of interests.
Additional information
Q. Wei and Z. Zheng contribute to this work equally.
Rights and permissions
About this article
Cite this article
Wei, Q., Zheng, Z., Guo, X. et al. Association between depression and survival in Chinese amyotrophic lateral sclerosis patients. Neurol Sci 37, 557–563 (2016). https://doi.org/10.1007/s10072-015-2472-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-015-2472-y