Abstract
In this study, neuroprotective effect of tamoxifen has been explored in spinal cord injury (SCI) in rats by examining factors influencing IKK/NF-kB pathway in SCI in rats. It has been shown in several studies that IKK/NF-kB signaling pathway plays a key role in pathophysiology of SCI. In this study, three groups of rats (n = 17 each) were selected that included, tamoxifen group (here tamoxifen was injected after SCI in rats), SCI group (here only dimethylsulfoxide was administered after inducing SCI in rats) and sham group (here only laminectomy was performed). The effect of tamoxifen (5 mg/kg) on various factors responsible for activation of IKK/NF-kB signaling pathway including NF-kB p65, phosphorylated I-kBα was studied through Western blotting as well as densitometry. The examination of expression of active caspase-3 and myeloperoxidase activity was also carried out through Western blot analysis and densitometry. A comparison of three groups of rats showed that administration of tamoxifen significantly reduced the expression of NF-kB p65 and phosphorylated I-kBα (P < 0.05) compared to control. It also attenuated the expression of active caspase-3 resulting in the reduction of apoptosis, and infiltration of leukocytes to the injury site was also greatly reduced in the group where tamoxifen was administered. Statistical analysis through SPSS 13.0 software showed a significant decrease in the expression of inflammatory factors in groups where tamoxifen was administered. We conclude that tamoxifen possesses the potential neuroprotective effects that can be explored further for future therapeutic techniques in treating spinal cord injuries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tamoxifen is well-known compound that is used as anti-estrogen (endocrine therapy) in premenopausal and postmenopausal women for the treatment of breast cancer in receptor-positive breast cancer. Different reports regarding other useful effects of tamoxifen from different experimental studies suggest potential neuroprotective roles in spinal cord injury (SCI), brain ischemia, intracerebral hemorrhage and hypoxic ischemia brain injury [1–3].
In experimental ischemic strokes, this compound has been found to be a potent inhibitor of cell swelling anion channels [4, 5]. Tamoxifen is reported to inhibit different pathways which are involved in central nervous system damage along with those amino acids which are released as a result of anion channels creation resulting from swelling of astrocytes [6]. It is also responsible for removing reactive oxygen species and considerably decreasing the synthesis of peroxynitrated protein in ischemia [7, 8]. In mouse and rat microglial cells, it triggers anti-inflammatory response through signaling cascades of lipopolysaccharides-activated proteins [9].
In case of traumatic SCI, several neural structures are affected [10, 11]. Several studies have been performed on SCI, but so far only a few therapies have been reported as pathophysiology of SCI is quite complex. Several approaches have been made to study secondary injuries to alleviate problems concerning with secondary injuries and to help maintain the necessary anatomical structures for functional recovery [12, 13]. In case of secondary injury, inflammatory responses play a major role and are a central player in pathogenesis of SCI [14]. The expression of inflammatory genes and regulation of many cytokines that play a potential role in mediating inflammatory pathways in injuries to central nervous system is mainly regulated by nuclear factor kappa B (NF-kB) family of transcription factors [15, 16]. Therefore, it has been shown that secondary damage in SCI can be controlled to much an extent by inhibiting the activation of NF-kB [17, 18]. It has been shown that a new approach towards neuroprotective effects can be adopted by the use of compounds that are capable of inhibiting biochemical mediators that are involved in secondary degeneration. An example is glutamate amino acid which is normally a physiological transmitter, but can be toxic in case present in high concentration. The increase in glutamate, (an example of excitatory amino acid) due to injury can cause damage to tissues which can be prevented by the use of glutamate receptor antagonists [19]. The prevention of nerve atrophy by the use neurotrophic compounds that result in neuroprotection is also an example of the use of such therapy [20, 21].
Tamoxifen has been reported to attenuate the subarachnoid hemorrhage (SAH) induced activation of TLR4/NF-kB signaling pathway in the cortex region and can potentially influence behavioral recovery and neurological function after SAH [22]. However, the protective effect of tamoxifen in SCI models remains a question mark and an effort has been made in this study to explore the neuroprotective effect of tamoxifen in SCI-induced rat models.
In the current study, we evaluated the effect of tamoxifen on activation of IKK’NF-kB pathway by studying the expression of I-kBα and NF-kB p65. The expression of activated caspase-3 was studied to examine the apoptotic events and myeloperoxidase activity was measured to study the infiltration of inflammatory cells.
Materials and methods
A total of 51 female Sprague–Dawley rats (pathogen-free grade, aged 10–12 weeks, and weighing 200–220 g) were obtained from China-Japan friendship hospital Beijing and all the work carried out was approved by the Ethics committee of China-Japan friendship hospital Beijing.
The rats were divided into three groups all having equal number of animals prior to the operation which were, SCI group (n = 17, SCI + subdural dimethyl sulfoxide injection), tamoxifen group (n = 17, SCI + subdural injection of tamoxifen) and sham group (n = 17, here only laminectomy was performed without SCI). In all cases, SCI was performed according to the previously described reports [25] and induction of injury was made on T12 segment. The NYU impactor was used for creating the SCI and vertebrae lamina was held in a position to withstand momentum from the rod. The rod was dropped from 12.5 mm height for induction of SCI. In sham group, spinal cord was not injured, however, vertical plate at T11–T13 segment was removed.
In tamoxifen group, rats received tamoxifen (Sigma-Aldrich, St Louis, MO, USA) that was dissolved in 2 % dimethylsulfoxide in (1 mg/ml) distilled water and was administered 30 min post-injury by intraperitoneal injection at 5 mg/kg, according to the previously described reports [5, 6]. The injection was administered near the injury site. Rats in SCI group received 2 % dimethylsulfoxide dissolved in distilled water and the same amount of dose as was given to tamoxifen group, but in SCI group tamoxifen was not administered. All the postoperative care procedures were carried out and bladders of rats were emptied manually twice a day.
After 24 h of SCI, animals were given a dose of 10 % chloral hydrate (600 mg/kg) and were anesthetized. Normal saline with 1 U/ml heparin was used to perform intra-cardiac perfusion and dissections of 10 mm injured spinal cord segments were carried out then.
Western blotting was used to examine NF-kB p65, phosphorylated I-kBα and activated caspase-3 according to the previously described techniques [23] with some modifications. Total Protein extraction kit (Applygen Technologies Inc., Beijing, China) was used to isolate total proteins from a 10 mm spinal cord segment containing the injury epicenter. BCA protein assay kit was used to determine protein concentrations according to the manufacturer’s protocol (Applygen Technologies Inc., Beijing, china). Samples were boiled for 5 min after diluting with sample buffer and 50 µg of protein from each sample was loaded on 4–20 % polyacrylamide gel, then it was transferred to polyvinylidene difluoride membrane after separation by electrophoresis. Then, the membrane was incubated with specific primary antibodies after blocking, mouse anti-rat NF-kB p65 monoclonal antibody (1:1,000 Santa Cruz Biotechnology Santa Cruz, CA, USA); monoclonal rabbit anti-reactivated caspase-3 antibody(1:1,000; Cell Signalling Technology, Danvers, MA, USA; monoclonal rabbit anti-rat phosphorylated I-kBα (ser32) antibody (1:500, cell Signalling Technology, Danvers, MA, USA). The visualization of reactive protein bands was carried out using horseradish peroxidase-conjugated anti-rabbit or anti-mouse IgG antibodies (1:2,000; Jackson West Grove, PA, USA), and an ECL Western blotting kit (Applygen Technologies Inc, Beijing, China) and was performed according to manufacturer’s instructions. X-ray film was used to which membranes were exposed for 10 s to 1 min. Actin was used as a loading control and a polyclonal rabbit anti-actin antibody (1:500, Santa Cruz Co., Santa Cruz, CA, USA) was used to detect actin in samples. Optical density (OD) value of each protein band was determined after bands were scanned and digitized using Gel Pro Analyser 4.0 software.
After 24 h of SCI, MPO activity in spinal cord tissues was determined to examine infiltration of inflammatory cells according to previously described studies [18]. Commercially used kits (Nanjing, Jiancheng Co., China) were used to measure the MPO activity; procedures were performed according to manufacturer’s protocol. MPO activity was defined as the amount of enzyme degraded with 1 µmol of peroxidase at 37 °C, expressed as number of units of MPO/mg of proteins.
For statistical analysis, SPSS 13.0 software (SPSS, Chicago, IL, USA) was used. Mean ± SD value expressed the experimental data. One-way analysis of variance was used to analyze the results followed by a Bonferroni post hoc test for multiple comparisons. P value of less than 0.05 was considered significant.
Results
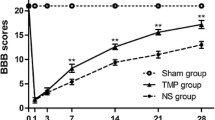
Expression of NF-kB p65
To examine the effect of tamoxifen against IKK/NF-kB pathway in spinal cord after 24 h of inducing SCI, Western blotting was used to study the expression of NF-kB p65 in spinal cord tissues. Comparing all three groups, it was observed that an increase in NF-kB p65 protein occurs in SCI group where dimethylsulfoxide was administered as compared to sham group (P < 0.01), while administration of tamoxifen significantly reduced the expression of NF-kB p65 after SCI in rats under study (Fig. 1).
Tamoxifen was able to affect expression of NF-kB p65 in SCI. a Western blotting showing levels of NF-kB p65 in all groups at 24 h after SCI where β-actin is used as a loading control. b OD values relative to control are shown of the densitometry of Western blots where significant difference in tamoxifen group values is indicated by P B < 0.01 and significant difference in SCI group is indicated by P A < 0.05
Expression of phosphorylated I-kBα
The expression of phosphorylated I-kBα in spinal cord tissues was also studied using Western blotting and it was observed that a significant increase in phosphorylated I-kBα is experienced in SCI group as compared to sham animal (P < 0.01), however, treatment with tamoxifen resulted in significant inhibition of production of phosphorylated I-kBα in spinal cord tissues after induction of injury and administration of tamoxifen (P < 0.05), results are shown in Fig. 2.
Effect of tamoxifen on expression of phosphorylated I-kBα in SCI. a Phosphorylated I-kBα production in spinal cord tissues from all the groups shown in representative Western blots. b Densitometry analysis of Western blots showing optical density (OD) values relative to controls. Significant differences in SCI as compared to sham group are indicated by P A < 0.01 and significant difference in tamoxifen-treated group is shown in the graph by P B < 0.05
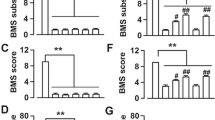
Results showing expression of active caspase-3 in all groups
To study the expression patterns of proteins associated with apoptosis the expression of active caspase-3 in spinal cord tissues after 24 h of inducing SCI Western blotting was used. The analysis showed a significant decrease in the expression of activated caspase-3 in group of rats treated with tamoxifen (P < 0.05), however, the expression remained significantly lower in sham group and significantly increased in SCI group as compared to sham group (P < 0.01), shown in Fig. 3.
Expression of caspase-3 is reduced after treatment with Tamoxifen a Western blot analysis of protein expression in all three groups. b Densitometry of Western blots showing OD values relative to control. Significant reduction in tamoxifen-treated group is indicated by P B < 0.05, while expression remains increased in SCI group as compared to Sham group indicated by P A < 0.01
Results showing MPO activity in all three groups under study
The effect of tamoxifen on infiltration of neutrophiles in SCI was studied where MPO activity in spinal cord tissues was investigated. It was observed that MPO activity was significantly increased in SCI group as compared to sham group after 24 h examination of induction of SCI, however, in case of tamoxifen administration this activity was reduced considerably. It is shown in Fig. 4.
Discussion
Several studies have focused on the neuroprotective effect of tamoxifen in several nerve injury models. In an intracerebral hemorrhage model, tamoxifen was reported to reduce perihematomal brain edema with an improved functional outcome by Xie et al. [2]. Inhibition of inflammatory response and reduction in cell apoptosis after SCI in adult rats was reported by Tian et al. [1].
The role of IKK/NF-kB pathway in secondary inflammation associated with SCI has been reported in several studies [18, 24]. Successful targeting of IKK/NF-kB pathway has been reported to be effective in reducing pathogenesis in SCI [17, 18]. Different compounds from traditional Chinese herbal medicine have been studied and reported for blocking NF-kB and NF-kB gene products in vitro [25]. In this study, we made an effort to determine whether tamoxifen possesses neuroprotective effects in vivo or not. Mechanisms underlying these neuroprotective effects were also studied. It was observed that tamoxifen successfully attenuates the activation of IKK/NF-kB pathway, expression of these factors and infiltration of inflammatory cells.
A major transcriptional regulator of inflammatory genes in SCI is NF-kB that is constituted of various Rel family proteins, p65, p50, p52, RelB and c-Rel. Activation of NF-kB can occur in different ways in which classical conical pathway involves I-kB kinase complex which plays an important role for the activation of innate immunity and inflammation [26]. IKKβ is the main subunit of IKK and it plays a role in activation of NF-kB after phosphorylating I-kB inhibitory proteins [27]. This study showed that expression of I-kBα was significantly reduced in spinal cord tissues in rats after SCI by administering tamoxifen. A decrease in the expression of NF-kB p65 was also observed in rats treated with tamoxifen, therefore, it was concluded that tamoxifen affects IKK/NF-kB canonical pathway in rats after SCI and has potential neuroprotective effects after SCI on rats.
As inflammatory responses are triggered after SCI, in these responses inflammatory cells are responsible for releasing massive proinflammatory mediators along with neurotoxins that result in generation of reactive oxygen and nitrogen species which can cause cellular damage [28, 29]. Among leucocytes neutrophiles are the first invaders of the injury site invading the injured spinal cord [30–32]. To examine the anti-inflammatory effect of tamoxifen the infiltration of leucocytes to injury site was studied using MPO activity. This is an indicator of polymorphonuclear leucocytes accumulation as myeloperoxidase which is a lysosomal protein is stored in azurophilic granules of neutrophiles. It was observed that in rats with SCI a downregulation of neutrophile infiltration occurs where tamoxifen was administered, while in case of SCI where tamoxifen was not administered an increased neutrophile infiltration was observed.
One of the key pathological events in case of SCI is apoptosis where axonal degeneration and demyelination of white matter tracts can result in functional problems of neurons [33–35]. In the process of apoptosis, activation of caspase-3 in many types of cells of central nervous system occurs, therefore, the assessment of expression of caspase-3 is an important indicator of examining the process of apoptosis. The suppression of expression of caspase-3 by tamoxifen in the current study shows that tamoxifen possesses anti-apoptotic properties in case of SCI.
All results in the current study suggest neuroprotective effects of tamoxifen in SCI in vivo and to the best of our knowledge this is the first report of mentioned properties of tamoxifen in vivo. Therefore, further efforts should be made to explore these properties of the potential neuroprotective effects of tamoxifen so that possible therapeutic approach to SCI can be established in future.
Conclusion
The current study suggests that tamoxifen successfully reduces the expression of NF-kB p65 and I-kBα and it can be used as a successful inhibitor of IKK/NF-kB pathway. Moreover, it also attenuates the infiltration of leukocytes as shown by the study of MPO activity and possesses anti-apoptotic properties as it attenuates the active caspase-3.
References
Tian DS, Liu JL, Xie MJ et al (2009) Tamoxifen attenuates inflammatory-mediated damage and improves functional outcome after spinal cord injury in rats. J Neurochem 109:1658–1667
Xie Q, Guan J, Wu G, Xi G, Keep RF, Hua Y (2011) Tamoxifen treatment for intracerebral hemorrhage. Acta Neurochir Suppl 1 11:271–275
Feng Y, Fratkins JD, LeBlanc MH (2004) Treatment with tamoxifen reduces hypoxic–ischemic brain injury in neonatal rats. Eur J Pharmacol 484:65–74
Kimelberg HK, Feustel PJ, Jin Y, Paquette J, Boulos A, Keller RW Jr, Tranmer BI (2000) Acute treatment with tamoxifen reduces ischemic damage following middle cerebral artery occlusion. Neuro Report 11:2675–2679
Kimelberg HK, Jin Y, Charniga C, Feustel PJ (2003) Neuroprotective activity of tamoxifen in permanent focal ischemia. J Neurosurg 99:138–142
Rutledge EM, Aschner M, Kimelberg HK (1998) Pharmacological characterization of swelling-induced D-[3H]aspartate released from primary astrocyte cultures. Am J Physiol 274:C1511–C1520
Wiseman H, Cannon M, Arnstein HR, Halliwell B (1993) Tamoxifen inhibits lipid peroxidation in cardiac microsomes. Comparison with liver microsomes and potential relevance to the cardiovascular benefits associated with cancer prevention and treatment by tamoxifen. Biochem Pharmacol 45:1851–1855
Osuka K, Feustel PJ, Mongin AA, Tranmer BI, Kimelberg HK (2001) Tamoxifen inhibits nitrotyrosine formation after reversible middle cerebral artery occlusion in the rat. J Neurochem 76:1842–1850
Suuronen T, Nuutinen T, Huuskonen J, Ojala J, Thornell A, Salminen A (2005) Anti-inflammatory effect of selective estrogen receptor modulators (SERMs) in microglial cells. Inflamm Res 54:194–203
Dumont RJ, Okonkwo DO, Verma S, Hurlbert RJ, Boulos PT, Ellegala DB, Dumont AS (2001) Acute spinal cord injury, part I: pathophysiologic mechanisms. Clin Neuropharmacol 24:254–264
Kwon BK, Tetzlaff W, Grauer JN, Beiner J, Vaccaro AR (2004) Pathophysiology and pharmacologic treatment of acute spinal cord injury. J Spine 4:451–464
Fehlings MG, Baptiste DC (2005) Current status of clinical trials for acute spinal cord injury. Injury 36(Suppl. 2):B113–B122
Rowland JW, Hawryluk GW, Kwon B, Fehlings MG (2008) Current status of acute spinal cord injury pathophysiology and emerging therapies: promise on the horizon. Neurosurg Focus 25(5):E2
Beattie MS (2004) Inflammation and apoptosis: linked therapeutic targets in spinal cord injury. Trends Mol Med 10:580–583
Hu X, Nesic-Taylor O, Qiu J, Rea HC, Fabian R, Rassin DK, Perez-Polo JR (2005) Activation of nuclear factor-kB signaling pathway by interleukin-1 after hypoxia/ischemia in neonatal rat hippocampus and cortex. J Neurochem 93:26–37
Karin M, Yamamoto Y, Wang QM (2004) The IKK NF-kappa B system: a treasure trove for drug development. Nat Rev Drug Discov 3:17–26
Brambilla R, Bracchi-Ricard V, Hu WH et al (2005) Inhibition of astroglial nuclear factor kB reduces inflammation and improves functional recovery after spinal cord injury. J Exp Med 202:145–156
Han X, Lu M, Wang S, Lv DC (2012) Targeting IKK/NF-kappa B pathway reduces infiltration of inflammatory cells and apoptosis after spinal cord injury in rats. Neurosci Lett 511:28–32
Panter SS, Yum SW, Faden AI (1990) Alteration in extracellular amino acids after traumatic spinal cord injury. Ann Neurol 27:96–99
Blesch A, Tuszynski MH (1997) Robust growth of chronically injured spinal cord axons induced by grafts of genetically modified NGF secreting cells. Exp Neurol 148:444–452
Bregman BS, Broude E, McAtee M, Kelley MS (1998) Transplants and neurotrophic factors prevent atrophy of mature CNS neurons after spinal cord injury. Exp Neurol 149:13–27
Xuebo S, Chengyuan J, Tong H, Zhong W, Gang C (2013) Tamoxifen as an effective neuroprotectant against early brain injury and learning deficits induced by subarachnoid hemorrhage: possible involvement of inflammatory signaling. J Neuroinflamm 10:157
Han X, Wang SY, Zhang Z, Lü DC, Liu HR (2011) BMS-345541 inhibited nuclear factor kappa B expression and improved locomotor function recovery in rats after acute spinal cord injury. Neural Regen Res 6:1775–1779
Beck KD, Nguyen HX, Galvan MD, Salazar DL, Woodruff TM, Anderson AJ (2010) Quantitative analysis of cellular inflammation after traumatic spinal cord injury: evidence for a multiphasic inflammatory response in the acute to chronic environment. Brain 133:433–447
Pandey MK, Sandur SK, Sung B, Sethi G, Kunnumakkara AB, Aggarwal BB (2007) Butein, a tetrahydroxychalcone, inhibits nuclear factor (NF)-kappaBand NF-kappaB-regulated gene expression through direct inhibition of IkappaBalpha kinase beta on cysteine 179 residue. J Biol Chem 282:17340–17350
Niederberger E, Geisslinger G (2008) The IKK-NF-kappa B pathway: a source for novel molecular drug targets in pain therapy. J FASEB 22:3432–3442
Huxford T, Huang DB, Malek S, Ghosh G (1998) The crystal structure of the IkappaBalpha/NF-kappa B complex reveals mechanisms of NF-kappa B inactivation. Cell 95:759–770
Bao F, Liu D (2003) Peroxynitrite generated in the rat spinal cord induces apoptotic cell death and activates caspase-3. Neuroscience 116:59–70
Bao F, Liu D (2004) Hydroxyl radicals generated in the rat spinal cord at the level produced by impact injury induce cell death by necrosis and apoptosis: protection by a metalloporphyrin. Neuroscience 126:285–295
Bethea JR (2000) Spinal cord injury-induced inflammation: a dual-edged sword. Prog Brain Res 128:33–42
Chatzipanteli K, Yanagawa Y, Marcillo AE, Kraydieh S, Yezierski RP, Dietrich WD (2000) Posttraumatic hypothermia reduces polymorphonuclear leukocyte accumulation following spinal cord injury in rats. J Neurotrauma 17:321–332
Trivedi A, Olivas AD, Noble-Haeusslein LJ (2006) Inflammation and spinal cord injury: infiltrating leukocytes as determinants of injury and repair processes. Clin Neurosci Res 6:283–292
Grossman SD, Rosenberg LJ, Wrathall JR (2001) Temporal-spatial pattern of acute neuronal and glial loss after spinal cord contusion. Exp Neurol 168:273–282
Hagg T, Oudega M (2006) Degenerative and spontaneous regenerative processes after spinal cord injury. J Neurotrauma 23:264–280
Jiang SC, Bendjelloul F, Ballerini Iolanda P, D’Alimonte I, Nargi E, Jiang C, Huang XJ, Rathbone MP (2007) Guanosine reduces apoptosis and inflammation associated with restoration of function in rats with acute spinal cord injury. Purinergic Signal 3:411–421
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wei, Hy., Ma, X. Tamoxifen reduces infiltration of inflammatory cells, apoptosis and inhibits IKK/NF-kB pathway after spinal cord injury in rats. Neurol Sci 35, 1763–1768 (2014). https://doi.org/10.1007/s10072-014-1828-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-014-1828-z