Abstract
In recent years research explored different acupuncture stimulation techniques but interest has focused primarily on somatic acupuncture and on a limited number of acupoints. As regards ear Acupuncture (EA) there is still some criticism about the clinical specificity of auricular points/areas representing organs or structures of the body. The aim of this study was to verify through (Functional magnetic resonance imaging) fMRI the hypothesis of EA point specificity using two auricular points having different topographical locations and clinical significance. Six healthy volunteers underwent two experimental fMRI sessions: the first was dedicated to the stimulation of Thumb Auricular Acupoint (TAA) and the second to the stimulation of Brain Stem Auricular Acupoint (BSAA). The stimulation of the needle placed in the TAA of the left ear produced an increase in activation bilaterally in the parietal operculum, region of the secondary somatosensory area SII. Stimulation of the needle placed in the BSAA of the left ear showed a pattern that largely overlapped regions belonging to the pain matrix, as shown to be involved in previous somatic acupuncture studies but with local differences in the left amygdala, anterior cingulate cortex, and cerebellum. The differences in activation patterns between TAA and BSAA stimulation support the specificity of the two acupoints. Moreover, the peculiarity of the regions involved in BSAA stimulation compared to those involved in the pain matrix, is in accordance with the therapeutic indications of this acupoint that include head pain, dizziness and vertigo. Our results provide preliminary evidence on the specificity of two auricular acupoints; further research is warranted by means of fMRI both in healthy volunteers and in patients carrying neurological/psychiatric syndromes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent years an increasing number of studies has been published investigating brain response to acupuncture stimulation. However, even if research explored different stimulation techniques, the interest was focused primarily on somatic acupuncture (SA) and on a limited number of acupoints (i.e. LI 4, ST 36, BL 60, [1]).
Advances in imaging techniques have made it possible to reach a certain consensus regarding the main brain networks involved in SA needle stimulation [2] and have shown the systematic involvement of brain areas such as the somatosensory and association cortices (SI and SII), insula, thalamus, amygdala, hippocampus and cingulate cortex. Taken together, these distributed brain areas belong to the network known as the “pain matrix” [3], but their responses can highlight the dissociation between the sensory-discriminatory aspect of pain and its affective component elicited by nociceptive stimuli [4]. Similarly, it has also been shown that the same regions are involved and modulated in pain anticipation [5], analgesia and placebo conditions [6, 7].
Since one of the main goals of acupuncture is to contribute to pain relief, the assessment of its specific therapeutic effects through the interaction with the pain matrix has a key role in evaluating brain imaging results.
As regards ear acupuncture (EA), despite its worldwide increasing application [8], there is still some criticism and a low level of evidence about the clinical specificity of auricular points/areas representing organs or structures of the body. In particular, scientific evidences of the somatotopic representation of the human body on the outer ear, a basilar concept on which EA is based, are scarce. Only one paper describes the consistent correlation between the stimulation of the auricular thumb area and the cortical activation of the correspondent S1 cortex [9].
The aim of this preliminary study was to highlight the brain correlates of EA and the specificity of two different auricular acupoints [Thumb Auricular Acupoint (TAA) and Brain Stem Auricular Acupoint (BSAA)] having different topographical location and clinical significance.
Materials and methods
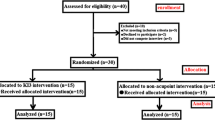
Six healthy volunteers (three male, three female; mean age 43.8 years) underwent two experimental fMRI sessions, spaced 24 h apart. All the participants provided written informed consent according to the Vaud Ethics Committee approval for MR pilot studies. The first session was dedicated to the stimulation of the TAA and the second to the stimulation of the BSAA for a total of four fMRI sessions per subject. We used titanium semi-permanent needles (ASP, Sedatelec, France) to stimulate the two acupoints. Each experiment was organized in a block- design fashion, with an alternation of four active and four rest blocks, each of them lasting 30 s. The first session consisted of three fMRI sessions. The active phase involved: flexion–extension of the left thumb, passive stimulation of the left thumb, and mechanical stimulation of the needle inserted in the TAA of the left ear. The TAA (Fig. 1, point A) was selected replicating the historic experiment performed by Paul Nogier and René Bourdiol [10]. We applied a nociceptive stimulation through a dynamometric clamp calibrated at 2 kg/cm2 to the left thumb for 60 s. The pain evoked during stimulation had to be maintained in each volunteer on a threshold basis of 5 on a Numeric Rating Scale (NRS) of pain ranging from 0 = no pain to 10 = worst pain. One minute after the nociceptive stimulation was stopped, one point in the somatotopic area of the thumb in the ear became hyperalgesic at palpation using a pressure probe of maximal 250 gr pressure (Pain Pressure Test—PPT) [8]. This point corresponded to the TAA in which the needle was inserted.
The second session was dedicated to the stimulation of BSAA and involved one fMRI experiment. The active block consisted in the mechanical stimulation of the needle in the BSAA of the left ear. The brain stem point naogan of the Chinese standardized auricular map corresponds exactly to the landmark of the notch between the antitragus and the antihelix [11] (Fig. 1, point B). This point was therefore identified at inspection and marked with ink without performing any PPT.
In both, sessions participants were asked to rate the pain they were experiencing through the NRS in four occasions: right after needle insertion, at 120 and 180 s after insertion, and after the fMRI to evaluate the pain felt during the mechanical stimulation of the ASP.
Image acquisition and processing
MRI protocol was performed on a Siemens 3T Tim Trio scanner and included a sagittal T1-weighted gradient-echo sequence (MPRAGE, 160 contiguous slices, 1 mm isotropic voxel, TR = 2300 ms, TE = 2.98 ms, FoV 256 mm) and the fMRI acquisition. Functional scans were acquired with an EPI sequence (TR = 3,000 ms, TE = 30 ms, flip angle = 90°, FoV 256 mm). The 28 axial slices (matrix size 128*128 with 4 mm slice thickness) were aligned with the anterior commissure–posterior commissure line. During each experiment, we collected 10 volumes for each block, for a total of 80 images. Magnetic resonance imaging data were pre-processed and analyzed using Statistical Parametric Mapping (SPM8, Wellcome Department of Imaging Neuroscience, London, England; http://www.fil.ion.ucl.ac.uk). Functional images were corrected for motion along the experiment by the mean of rigid-body transformations and then co-registered to the high-resolution T1w acquisitions. The anatomical images were then normalized to the MNI T1 template and the normalization parameters were applied to the functional images, which were finally smoothed with a 6 mm Gaussian kernel. All the pre-processing steps mentioned minimized the non-task-related variability, and thus the source of error within the acquired fMRI time series. Single-subject statistics were performed according to the General Linear Model and group analyses were performed modelling within-subject variability as fixed-effects. Contrasts of interest were thresholded for peak height at p = 0.05 (family-wise error (FWE) corrected), with an extent threshold (k) of 50 voxels. The limitation of modelling intra-subject variability as fixed effect implies that the results described should be considered descriptive thus providing valid inference only about the specific sample used [12].
Results
Numeric Rating Scale pain scores decreased from a mean value of 4.6 ± 2.4 and of 5.1 ± 2.5, for TAA and BSAA, respectively, immediately after needle insertion, to 0.8 ± 1.1 and to 0.8 ± 0.7 after 120 s, and to 0 for both needles after 180 s. The mean value reported by subjects during the fMRI session was 3.6 ± 3.9 for TAA and 0.3 ± 0.5 for BSAA.
Functional MRI of voluntary movement of the left thumb revealed extensive activation of the right motor, right primary and secondary somatosensory (M1, SI and SII) cortices with a maximal activity in the precentral gyrus. Gentle touch showed a similar pattern in SI and SII cortices.
These first two experiments served as the basis for defining the volumes of interest for the detection of the effects of TAA stimulation. The applied mask included all sensory motor areas of the thumb (bilateral primary and secondary somatosensory cortices, primary motor cortex, supplementary motor area, and the cerebellum). The mask was created by thresholding the group result of the motor and touch paradigms (p < 0.05 FWE corrected) and by adding the same region mirrored to the other hemisphere. By applying the mask thus defined, activations of the TAA stimulation could be easily compared to the brain regions involved in either the voluntary movement or in gentle touch in both hemispheres.
As depicted in Fig. 2, the stimulation of the needle placed in the TAA of the left ear produced a focal increase in activation bilaterally in the parietal operculum, region of the secondary somatosensory area SII (clusters’ centre of gravity: x, y, z = − 53, −26, −24 and 62, −18, 18 in MNI coordinates).
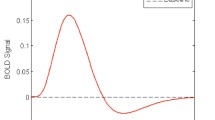
Stimulation of the needle placed in the BSAA of the left ear showed a significant and extensive pattern of increase and decrease activation compared to rest (Fig. 3, top row). Maximum intensity increase was reached in the left anterior insula (center of gravity of the cluster in the MNI 345 space x, y, z = −40, 8, −2) although the involvement of this region was bilateral (x, y, z = 38, 13, −2, Fig. 3, bottom part). A larger cluster included the left posterior insula (x, y, z = −36,−18,−2), extending to the precentral and inferior frontal gyri (x, y, z = −57, 0, 7). The bilateral involvement of postcentral (x, y, z = −58, 19, 17) and supramarginal gyri (x, y, z = −57, 29, 24) showed predominance in the left hemisphere. Moreover, we evidenced a bilateral increase of the BOLD signal in the thalamus (x, y, z = 8,−12,7 and −8, −19, 7), in the left amygdala (x, y, z = −26, −6, −18), and in the cerebellum (Lobule 4 and 5 bilaterally and lobule 6 with a left predominance).
Decreased activity compared to rest was found in the medial frontal gyrus (x, y, z = 8, 48, −6) extending to the subgenual anterior cingulate cortex (x, y, z = 9, 34, 0), in the caudate (x, y, z = −5, 17, 0 and 6, 15, 0), in the superior frontal gyrus bilaterally (x, y, z = −14, 44, 32 and 13, 35, 31) and in the right orbitofrontal cortex (x, y, z = 35, 48, −9).
It should be mentioned that activation of the brain due to the touching of the ear was removed from these results by excluding the region commonly activated in both experiments, and that the pattern of deep activations found during BSAA stimulation was absent in TAA activation (without the mask restriction).
Linear correlation analysis between the BOLD signal and NRS score of each subject at needle insertion did not show any statistically significant relations.
Discussion
Our preliminary study achieved two main results, giving new evidence of the specificity of EA. We studied two acupoints located on distant parts of the ear and having different clinical significance. First, we showed that stimulation of the TAA selectively activates the secondary somatosensory area bilaterally. Instead, the stimulation of the BSAA, in accordance with its therapeutic effect, mostly activates cortical and limbic regions that are part of the pain matrix.
The thumb point was identified with PPT which is a reliable and reproducible method used by acupuncturists to identify one or more ear acupoints related to ailments and dysfunctions in the body. It should be remarked that the representation of the human body on the auricle is probably “homunculus-like” and auricular diagnosis relies on the identification of more or less larger areas which are proportional to innervation and functionality of the corresponding structure. In this respect, from the diagnostic point of view the thumb probably has a larger representation than the other fingers of the hand. Therefore, the identification and the treatment of the most tender point within this area may give the best therapeutic effect.
Whereas the TAA has the same indication, i.e. pain, overall on different auricular maps, the BSAA has a very different clinical significance according to Western and Chinese auricular maps. In Western maps it is considered as the atlas (C1) point, whereas according to Chinese standardized maps it holds the name of brain stem point naogan and is indicated for Ménière’s disease, epilepsy, brain trauma, allergic dermatitis and headache. According to Romoli [8] this point seems to be active in insomnia, tension-type headache, depression, dizziness, vertigo and postural disorders with chronic cervical and lumbar pain. It is therefore interesting that the stimulation of this point may activate areas of the pain matrix involved in the processing of the affective-cognitive components of pain perception. Literature indicates that activity in regions belonging to the pain matrix are downregulated and upregulated in response to pain [4]. More specifically, the caudal part of the Anterior Cingulate Cortex (ACC) generally shows increase in BOLD response during pain while activity in the amygdala is generally downregulated after a noxious stimulus. In contrast to this and in apparent discrepancy with results on somatic acupuncture [1, 2, 13], we found an increase in BOLD response in the left amygdala and failed to find any significant activation in the caudal ACC. A possible explanation of our findings may rely on the fact that none of our subjects experienced pain during needle stimulation, so no adaptive strategies to pain were needed (see. “Results” on NRS pain scores). Furthermore, in light of the well-known function of the amygdala in processing the affective component of pain and in analgesia, these changes of activation may be due to the therapeutic effects characteristic of BSAA.
A further significant result is the increase of BOLD response found in the cerebellum. Vertigo, dizziness, ataxia or postural problems are symptoms related to a dysfunction of the vestibular system [14]. The activations found in the insula, extending to its posterior part in the left hemisphere, in the temporo-parietal cortex and the cerebellum, support the interaction of the acupoint stimulation with the vestibular network, in accordance with the mentioned additional therapeutic indications of BSAA.
The activation pattern found during BSAA stimulation, although involving symmetrical regions, show a clear predominance in the left hemisphere. This finding is in accordance with the hypothesis that auricular acupoints mainly project in the hemisphere homolateral to the stimulated ear.
The results of our pilot study show that specificity of auricular acupoints can be assessed by fMRI and that brain responses for the two acupoints tested (TAA, BSAA) might be linked to their respective therapeutic indications. The present study provide a basis for supporting the systematic investigation of other auricular points, especially areas of the outer ear, such as the tragus, antitragus and ear lobe which are supposed to be correlated with different parts of the central nervous system.
Abbreviations
- EA:
-
Ear acupuncture
- SA:
-
Somatic acupuncture
- TAA:
-
Thumb auricular acupoint
- BSAA:
-
Brain stem auricular acupoint
- fMRI:
-
Functional magnetic resonance imaging
References
Huang W, Pach D, Napadow V, Park K, Long X, Neumann J, Maeda Y, Nierhaus T, Liang F, Witt CM (2012) Characterizing acupuncture stimuli using brain imaging with FMRI—a systematic review and meta-analysis of the literature. PLoS One 7(4):e32960
Chae Y, Chang DS, Lee SH, Jung WM, Lee IS, Jackson S, Kong J, Lee H, Park HJ, Lee H, Wallraven C (2013) Inserting needles into the body: a meta-analysis of brain activity associated with acupuncture needle stimulation. J Pain 14:215–222
Ingvar M (1999) Pain and functional imaging. Philos Trans R Soc Lond B Biol Sci 354:1347–1358
Petrovic P, Ingvar M (2002) Imaging cognitive modulation of pain processing. Pain 95:1–5
Wager TD, Rilling JK, Smith EE, Sokolik A, Casey KL, Davidson RJ, Kosslyn SM, Rose RM, Cohen JD (2004) Placebo-induced changes in FMRI in the anticipation and experience of pain. Science 303:1162–1167
Petrovic P, Kalso E, Petersson KM, Ingvar M (2002) Placebo and opioid analgesia—imaging a shared neuronal network. Science 295:1737–1740
Tracey I, Mantyh PW (2007) The cerebral signature for pain perception and its modulation. Neuron 55:377–391
Romoli M (2010) Auricular Acupuncture Diagnosis. Churchill-Livingstone, Edinburgh
Alimi D, Geissmann A, Gardeur D (2002) Auricular acupuncture stimulation measured on functional magnetic resonance imaging. Med Acup 13:18–21
Bourdiol RJ (1982) Elements of auriculotherapy. Maisonneuve
Technical Supervise Bureau of State (1993) The nomenclature and location of ear acupuncture points. Chinese Standard Publishing House, Beijing
Friston KJ, Holmes AP, Price CJ, Buchel C, Worsley KJ (1999) Multisubject fMRI studies and conjunction analyses. Neuroimage 10:385–396
Cho ZH, Oleson TD, Alimi D, Niemtzow RC (2002) Acupuncture: the search for biologic evidence with functional magnetic resonance imaging and positron emission tomography techniques. J Altern Complement Med 8:399–401
Dieterich M, Brandt T (2008) Functional brain imaging of peripheral and central vestibular disorders. Brain 131:2538–2552
Acknowledgments
This work was supported by the Centre d’Imagerie Biomédicale (CIBM) of the University of Lausanne (UNIL), the Swiss Federal Institute of Technology Lausanne (EPFL), the University of Geneva (UniGe), the Centre Hospitalier Universitaire Vaudois (CHUV), the Hôpitaux Universitaires de Genève (HUG), and the Leenaards and Jeantet Foundations.
Conflict of interest
All the authors certify that there is no actual or potential conflict of interest in relation to this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Romoli, M., Allais, G., Airola, G. et al. Ear acupuncture and fMRI: a pilot study for assessing the specificity of auricular points. Neurol Sci 35 (Suppl 1), 189–193 (2014). https://doi.org/10.1007/s10072-014-1768-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-014-1768-7