Summary
Twenty years ago the hypothesis was introduced that acupuncture stimulation may activate specific areas of the brain. However only recently this diagnostic procedure has become more and more appealing for investigating some crucial aspects of acupuncture, such as the comparison between “verum” and “sham” acupuncture, the intensity of stimulation (with or without deqi effect), the differences between points located on the same meridian or on different meridians. Most studies of the literature suggest that acupuncture can modulate the activity of the brain, both with activating and deactivating specific areas.
With regard to ear acupuncture it is not clear to us why in the same period only three fMRI studies have been published applying this technique, one in 2002 and two in 2014. In the first study Dr. David Alimi demonstrated with a Block Design that auricular stimulation of the thumb point activated the somesthetic area S1 contralaterally in 6 subjects and bilaterally in 3 subjects. In the second study, performed by Romoli and coll., for the first time the specificity of auricular points was explored, choosing two points (thumb and brain stem) which are topographically distant from each other and have different therapeutic indications. In the same year a second study was organized by Dr. Alimi and Dr. Bahr the purpose of which was to evaluate the differences stimulating the knee point according to Nogier-Bahr or according to the current Chinese auricular map. The aim of this article is to promote further investigations with fMRI on a series of fundamental or particularly active points regulating the neuroendocrine and vegetative functions such as Nogier’s Zero point, Shenmen, Endocrine, Occiput etc.
Zusammenfassung
Vor 20 Jahren stellte man die Hypothese auf, dass die Akupunkturstimulation spezifische Areale des Gehirns aktivieren könnte. In den letzten Jahren wurden der Vergleich zwischen „verum“ und „sham“ Akupunktur, die Stimulationsintensität (mit und ohne deqi Effekt), die Unterschiede zwischen Punkten desselben Meridians und Punkten verschiedener Meridiane erforscht. Die meisten Studien zeigen entweder Aktivierung oder Deaktivierung spezifischer Hirnareale.
In Bezug auf die Ohrakupunktur verstehen wir nicht, warum im selben Zeitraum nur drei fMRI Studien, mit der Applikation dieser Technik, veröffentlicht wurden, eine in 2002 und zwei in 2014. In der ersten Studie von 2002 bewies Dr. David Alimi mit einem Block Design, dass die Stimulation des Daumenpunktes an 6 Testpersonen die kontralaterale und bei 3 Testpersonen bilateral die somatosensorische Zone S1 aktiviert hat. In der zweiten Studie, von Romoli und Kollegen, wurde zum ersten Mal die Spezifizität zweier Ohrpunkte erforscht (Daumenpunkt und Hirnstamm – 25), die topographisch voneinander entfernt sind und verschiedene therapeutische Indikationen haben. Im selben Jahr wurde eine zweite Studie von Dr. Alimi und Dr. Bahr durchgeführt, um die Unterschiede der Stimulation des Kniepunktes nach Nogier-Bahr und nach der chinesischen Ohrakupunkturkarte zu bewerten. Wir möchten, unter Ausnutzung des fMRI, die Erforschung wichtiger, besonders aktiver, neuro-endokrin und vegetativ regulierender Akupunkturpunkte fördern, wie Nogier’s Nullpunkt, Shenmen – 55, Endokrinum – 22, Polster – 29 usw.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The direct relationship between neural activity and the fMRI response is not yet understood. What fMRI is able to measure are the differences in resonances of the brain tissues based on the BOLD (Blood-Oxygen-Level-Dependent) SIGNAL. This signal reflects the hemodynamic change during activation of the brain; that is when blood flow increases, oxygen increases and deoxyhemoglobin decreases. Consequently this mechanism leads to an increase in fMRI signal. The BOLD signal is not measured from individual neurons but rather from small regions (2-3 mm3) of the brain called voxels (voxel = combination of volume and pixel). Therefore the BOLD effect is indicative of the group activity of the neurons located in the voxel. Because the signal is based on blood flow, it is delayed in time from the onset of neural activity due to the period it takes for blood to flow into and out of the voxel. The peak of the BOLD signal, 4-6 seconds after the onset of neural activity, returns to baseline or even to sub-baseline levels around 8-12 seconds after onset. If there is no additional neural activity the BOLD signal returns, approximately after 20 seconds, to baseline levels. This signal dynamic is called also Hemodynamic Response Function (HRF) (Fig. 1).
If we have to test a hypothesis, for example about the effect of acupuncture stimulation we need a Block Design where the stimulus is applied for a period of time (from 10 sec. to 120–180 sec.) followed by absence of stimuli for the same period.The peak BOLD signal from a block design is much larger and is more suitable and sensitive for measuring the selectivity for the probed stimulus (Fig. 2).
The Block Design, comparing several activity periods over an equal number of rest periods, generates a color coded statistical map of the relevant difference between brain areas with and without BOLD effect (see figure 3).
Acupuncture and fMRI
Twenty years have passed since Yoshida’s historical paper in which the future applications of fMRI for studying the mechanisms of acupuncture were emphasized [1]. The number of publications has grown exponentially in recent years and the leading countries are in order Mainland China, US, UK, Korea and Germany. The best systematic review and meta-analysis on acupuncture and fMRI was performed by Huang and coll. in 2012 [2]. 149 papers (1999-2009) were included for descriptive analysis and 34 were eligible for the meta-analysis. The following aspects were considered by the authors:
-
1.
Differences between “verum” and “sham” acupuncture,
-
2.
differences due to various methods of acupuncture manipulation (manual, electrical, with/without deqi effect)
-
3.
differences between patients and healthy subjects,
-
4.
differences between different acupuncture points (AP). As regards the first aspects 53 studies investigated different modalities such as
-
a.
Placebo needle (the Streitberger needle, with a blunt tip, pricking the skin without penetration) (4 studies),
-
b.
needling at non-acupuncture points in close proximity to AP (25 studies),
-
c.
needling at non-acupuncture points distant to AP (6 studies),
-
d.
cutaneous stimulation at the same AP or at sham points (18 studies, with contradictory results).
-
a.
64 % of the 25 studies comparing AP to non-AP showed that the first modality was associated with a higher activation of some brain areas (somatosensory, motor, basal ganglia, cerebellum, limbic system and prefrontal cortex). As regarding the fourth aspect, differences between different AP, this was a “hot” theme investigated in 76 studies addressing 37 AP, among them LI 4, ST 36, PC 6, LR 3 and GB 34 for their wide applicability and frequent use in clinical practice. If we consider in Huang’s review the descriptive level map of 18 AP located along 9 meridians we can see that the brain maps of each point differ considerably from each other. If indeed we compare the effects of the stimulation of some fundamental and often used points in the practice, such as SP 6, PC 6, ST 36, LR 3 and LI 4, with other points on the same meridian, we can see that the induced brain activity (both as activation and deactivation) is significantly higher (Fig. 3).
In the discussion of the article, Huang and coll. said that published results on acupuncture and fMRI were heterogeneous and that more high quality studies with more transparent methodology were needed to improve the consistency amongst different studies. From a descriptive perspective, however, most studies suggested that acupuncture can modulate the activity within specific areas and the evidence-based meta-analyses confirmed some of these results:
-
1.
“verum” acupuncture versus “sham” tends to be associated with more activation in the basal ganglia, brain stem, cerebellum and insula; with more deactivation in the limbic areas such as amygdala and hippocampus,
-
2.
a greater intensity of acupuncture stimulation seems to give a higher brain activation,
-
3.
a low frequency of electric stimulation tends to activate a broader range of brain areas than the stimulation at high frequencies,
-
4.
patients respond seemingly to acupuncture with a more robust fMRI activation than healthy subjects.
Ear Acupuncture and fMRI
Compared to the 149 articles included by Huang in his review on acupuncture and fMRI, three studies on ear acupuncture applying this kind of imaging in the period of 2002-2014 are really a very low number. Let us examine them.
In the year 2002 Dr. David Alimi performed a research at the center of Neuroradiology of Basel (Prof. Geissmann) on ten subjects (5 male, 5 female; age 18-52) [3]. The procedure was the following: The somatotopic representation of the right thumb on the ear was searched out by inducing a nociceptive stimulation of the thumb with a dynamometric clamp calibrated at 2 kg/cm2. The thumb point on the ear was identified by electrical detection using the device PointoSelect DT+, Schwa-medico, Germany. A Block Design was then performed and the following five recording sequences (30 seconds and 30 seconds rest) were carried out:
-
1.
At rest,
-
2.
during tactile stimulation of the right thumb at a frequency of 2 Hz,
-
3.
during tactile stimulation of the thumb’s auricular site previously located,
-
4.
after the insertion of 3 gold needles to a depth of 3 mm into the right thumb’s auricular site,
-
5.
during mechanical acupuncture stimulation at a 2 Hz frequency of the same gold needles with a 30° lateral inclination (needles were stitched into the right thumb’s auricular site).
In all subjects an overlapping activation of the primary somatosensory area S1 was obtained both with tactile and acupuncture stimulation; in 6 subjects the activation was contralateral, in 3 subjects bilateral.
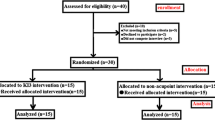
The aim of our study was to verify through fMRI the hypothesis of ear acupuncture point specificity, using two auricular points having different topographical locations, different clinical significance and being identified with different diagnostic methods [4] (Fig. 4).
Six healthy volunteers (three male, three female; mean age 43.8 years) underwent two experimental fMRI sessions, spaced 24 h apart.The first session was dedicated to the stimulation of the left thumb point. The historic experiment of Nogier-Bourdiol was replicated, as Alimi did previously, applying a dynamometric clamp calibrated at 2 kg/cm2 to the left thumb for 60 sec. One minute after the nociceptive stimulation one sensitive point was detected with Sedatelec’s probe of maximal 250 gr pressure. A Block Design was performed for the thumb point alternating five active and five rest blocks for each of them lasting 10 seconds. The following four recording sequences were carried out:
-
1.
At rest
-
2.
flexion-extension of the left thumb,
-
3.
tactile stimulation of the left thumb,
-
4.
mechanical stimulation of the needle (ASP titanium needle – Sedatelec) inserted in the left thumb point.
The second session, 24 h later, was dedicated to the stimulation of the left brain stem (naogan) point which corresponds to the Chinese standardized map (1992–2008) exactly to the landmark of the notch between the antitragus and the antihelix. This point was therefore identified at inspection and marked with ink without performing any further detection. The active block consisted in the mechanical stimulation of the ASP titanium in the brain stem point. Pain experienced at the insertion of the ASP was rated, through Numeric Rating Scale (NRS) of pain ranging from 0 = no pain to 10 = worst pain, on four occasions: after needle insertion, 120 and 180 sec. after insertion, after mechanical stimulation (Tab. 1).
Tactile stimulation of the left thumb showed a similar activation pattern in S1 and S2. As depicted in figure 5 A, the thumb auricular point stimulation produced a focal increase in activation bilaterally in the parietal operculum, the region of the secondary somatosensory area S2. The naogao point stimulation showed a significant and extensive pattern of increased and decreased activation compared to rest (Fig. 5 B, top row) of cortical and limbic regions that are part of the “pain matrix” involved in the processing of the affective-cognitive components of pain perception. The clear predominance of activation in the left hemisphere is discussed at the end of this article (see Discussion, page 17). It should be mentioned that the pattern of deep activations found during the brain stem point stimulation was absent in the thumb point activation. Linear correlation analysis between the BOLD signal and NRS score of each subject after needle insertion and after mechanical stimulation did not show statistically significant relations.
The results of our first study show that specificity of auricular points can be assessed by fMRI and that brain responses for the two AP tested might be linked to their respective therapeutic indications. The present study provides a basis for supporting the systematic investigation of other auricular points, especially areas of the outer ear, such as the tragus, antitragus and ear lobe which are supposed to be correlated with different parts of the central nervous system.
A few months later a third study was published about the stimulation of the auricular areas of the knee according to the French-German and Chinese localizations [5]. Nine right-handed and one left-handed healthy volunteers, 5 men and 5 women, aged 26-72 years, took part in this research. A Block Design was performed for the right knee point alternating active and rest blocks for each of them lasting 30 seconds. The following four recording sequences were carried out:
-
1.
At rest,
-
2.
cutaneous stimulation of the right knee,
-
3.
mechanical stimulation, either with copper needles or cryonics needles, of the point of the knee according to Nogier-Bahr or to Chinese localization.
The conclusion of this study was that the Chinese area covers in all cases the area of skin activation of the knee, but is piecemeal, incomplete, too vague and less specific than the French-German area.
Finally Romoli and coll. have a second study in progress. The research questions are the followings:
-
1.
Is there also a specificity of auricular points/zones located nearby, such as the representation of the fingers and the toes on the current standardized Chinese map [6] (Fig. 6)?
-
2.
does the stimulation of these points activate the corresponding somatosensory areas of the cortex?
-
3.
does the stimulation activate the ipsilateral/contralateral/bilateral hemispheres?
We are currently studying right-handed healthy volunteers, aged 25-30. The auricular sites are previously located with the „palpeur“ of 250 gr. on the right ear, and marked, one minute after mechanical nociceptive stimulation in random sequence of the right thumb and right hallux. As soon as one point loses its sensitivity, the other point is detected. All subjects were blinded about the investigation protocol and no one had previous experience with auriculotherapy. A Block Design (10 sec. alternated with 10 sec. of no stimulation) was then performed and the following five recording sequences were carried out:
-
1.
At rest,
-
2.
during tactile stimulation of the right thumb (frequency of 1 Hz),
-
3.
during tactile stimulation of the right hallux (frequency of 1 Hz),
-
4.
during needle stimulation of the auricular site of the right thumb (frequency of 1 Hz),
-
5.
during needle stimulation of the auricular site of the right hallux (frequency of 1 Hz).
The preliminary results of this second study (a group of 15 subjects is foreseen) allow the following considerations:
-
_ The specificity of auricular points seems confirmed also for points located close to each other on the auricle (Fig. 6, 7),
-
_ the auricular stimulation activates predominantly the ipsilateral hemisphere or both hemispheres.
We may therefore suppose the implication in auriculotherapy of other neural circuits besides those “classically” involved in the somatosensorial stimulation.
Discussion
Our preliminary observations that auricular stimulations evoke a significantly higher activation of the ipsilateral hemisphere cannot easily be explained and raise several further questions. It is well known that the system of somatosensory afferents carrying stimuli originated at cutaneous level projects itself to the contralateral hemisphere. This happens because there is a decussation of the afferent fibers in the brain stem or in the medulla, according to the different sensations transmitted, tactile, nociceptive, vibrational, thermic etc. Why a cutaneous stimulation of a zone of the body such as the auricle should activate the brain bilaterally and even prevalently the ipsilateral hemisphere, it is not clear. Similarly it is not clear why therapists commonly treat the ear ipsilateral to the site of lesion, for example the left ear in case of nociceptive pain of the left shoulder. In this case, following strictly the “classical” notions of neurophysiology we should stimulate the contralateral ear, what less frequently happens in the practice. Only hypotheses can therefore be forwarded: At first we may suppose, how proposed by some neurophysiologists and anatomists, that the auricular stimulation can activate some subcortical structures such as the brainstem, which is unfortunately a difficult region to be investigated with fMRI. A second hypothesis, not necessarily unlinked with the first, is that auricular stimulation may activate several systems and not only the somatosensory one how it is commonly considered. The fact that diagnostically relevant auricular points for example, in a similar pattern to points located on acupuncture meridians, show a lower electrical resistance let us think about the important implication of the Vegetative Nervous System (VNS) in regulating the electrical properties of the skin. It is therefore possible that autonomic nervous pathways could be involved, through their hypothalamic connections, in the bilateral cortical projection of the auricular stimulation. We need however further studies on a larger number of subjects before we can support with a higher probability that auricular stimulation may be associated with this kind of cerebral activation. Independently from the side of cortical activation, our preliminary results show that there is a fair overlapping between the tactile stimulation of the thumb and the hallux and the stimulation of the corresponding auricular points.
Conclusions
fMRI seems an interesting method for studying the specificity of auricular points. Besides the points related to pain syndromes located in different parts of the body it would be interesting to investigate a series of fundamental or particularly active points regulating the neuroendocrine and VNS functions such as Nogier’s Zero point, Shenmen, Endocrine, Occiput etc.

M. Romoli
References
Yoshida, T, Tanaka, C, Umeda, M et al.: Non-invasive measurement of brain activity using functional MRI: toward the study of brain response to acupuncture stimulation. Am J Chin Med 23(3-4), 1995: 319–25
Huang, W, Pach, D, Napadow, V, Witt, C et al.: Characterizing acupuncture stimuli using brain imaging with fMRI - A systematic review and meta-analysis of the literature. PLoS ONE 4, 2012: 1–19 (168 references)
Alimi, D, Geissmann, A, Gardeur, D: Auricular acupuncture stimulation measured on fMRI imaging. Med Acup 2, 2002: 18–21
Romoli, M, Allais, G, Airola, G, Fornari, E et al.: Ear acupuncture and fMRI: a pilot study for assessing the specificity of auricular points. Neurol Sci 35 (Suppl), 2014: S189–S193
Alimi, D, Geissmann, A, Gardeur, D, Bahr, F: Study in fMRI of the stimulation of the auricular areas of the knee as the French-German and Chinese localizations. The Journal of Radiology. Photon 125, 2014:133–141
Technical Supervise Bureau of State: The nomenclature and location of ear acupuncture points. Chinese Standard Publishing House 1993 - 2008 Beijing
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Romoli, M., Leombruni, S., Morese, R. et al. EAR ACUPUNCTURE AND FMRI. Akupunkt Aurikulomed 41, 12–18 (2015). https://doi.org/10.1007/s15009-015-5316-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15009-015-5316-1