Abstract
White matter hyperintensities (WMH) are common in stroke. The influence of WMH on health-related quality of life (HRQoL) following a lacunar stroke is unknown. This study evaluated the impact of WMH on HRQoL in acute lacunar stroke. A cohort of 160 patients with acute lacunar stroke admitted to the stroke unit of a university-affiliated regional hospital in Hong Kong was recruited. Three months after the index stroke, a research assistant administered the Short Form-36 (SF-36) to assess HRQoL. The severity of WMH was evaluated with magnetic resonance imaging (MRI). In univariate analysis, the severity of deep WMH (DWMH) negatively correlated with patients’ vitality (VT; p < 0.05), social function (SF; p < 0.001), role-emotional (RE; p < 0.01), mental health (MH; p < 0.01), and mental component summary (MCS; p < 0.001) scores of HRQoL. DWMH was independently associated with all of the above five SF-36 scores (p < 0.05) in linear regression analysis. These findings suggest that DWMH has a significant impact on the HRQoL of stroke survivors. The importance of DWMH in the long-term HRQoL in lacunar stroke warrants further investigation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lacunar stroke accounts for 25 % of all ischemic strokes [1]. Lacunes are caused by occlusion of a single, deep penetrating artery. Lacunar stroke is associated with milder neurological deficits [1]. The short term survival rate is higher and the recurrence rate is lower in lacunar strokes than in non-lacunar strokes [2].
Patients with stroke have been shown to have poor HRQoL [3]. Correlates of poor HRQoL 1 month to 3 years after stroke include older age [4, 5], female sex [6], being single or widowed [6], a high degree of neurological deficit [7], cognitive impairment [8], and depression [9]. Patients with lacunar stroke may have better HRQoL than other stroke patients [4].
White matter hyperintensities (WMHs) are areas of increased signal intensity that become apparent particularly on T2-weighted MR [10]. They are thought to reflect underlying cerebrovascular disease. Neuropathological studies show that WMHs characterize arteriosclerosis, ischaemia, incomplete infarction, and infarction with necrosis [11]. WMHs are common in ischaemic stroke [12] and have a direct effect on various outcome measures, such as cognitive impairment [13], depression [14], and functional outcome [15], thereby resulting in poorer HRQoL. White matter lesions adversely affect HRQoL in patients with asymptomatic atherosclerosis [16] and multiple sclerosis [17]. There seems to be no association between the MRI correlates of WMH and HRQoL in ischemic stroke [18]. One study revealed an association between WMH and both the physical and mental aspects of HRQoL [19] in ischemic stroke. To the best of our knowledge, no study has specifically examined the radiological correlates of HRQoL in lacunar stroke, and there are no data on the impact of WMH on the HRQoL of lacunar stroke patients. Hence, the effect of WMH on HRQoL in lacunar stroke remains unknown.
Aims and/or hypothesis
This study set out to examine whether the severity or location of WMH contributes to HRQoL in acute lacunar stroke survivors.
Methods
Subjects
Of the 2,085 patients admitted with first-ever or recurrent stroke to the Acute Stroke Unit (ASU) of the Prince of Wales Hospital (PWH)—a university-affiliated general hospital serving a population of 800,000 in Hong Kong—from May 2005 to May 2007, 740 received an MRI examination. Due to limited access to MRI machines, MRI is generally reserved for stroke patients with stable neurological conditions. Compared to patients who did not receive an MRI examination, those with an MRI were younger (67.4 ±12.1 vs. 74.7 ±12.0; p < 0.001), more likely to be men (58.5 vs. 45.5 %; p < 0.001), and had less severe stroke as reflected by a lower National Institutes of Health Stroke Scale (NIHSS) score (5.5 ±4.3 vs. 10.9 ±9.8, p < 0.001).
One hundred and 60 patients who received an MRI entered the study. The inclusion criteria were: (1) Chinese ethnicity; (2) age 18 or above; (3) well-documented (clinical presentation and CT scan of the brain) first or recurrent acute lacunar stroke occurring within the 7 days prior to admission. Lacunar stroke was defined as at least one symptomatic infarction (diameter 2–15 mm) in the internal capsule, thalamus, basal ganglia, coronal radiate, centrum ovale, or infratentorial region confirmed by brain MRI; patients with any cortical and subcortical non-lacunar infarct (diameter >15 mm) were excluded; (4) Cantonese dialect as the primary language; and (5) willingness to give consent. The exclusion criteria included (1) transient ischemic attack, cerebral hemorrhage, subdural hematoma, or subarachnoid hemorrhage; (2) history of a central nervous system (CNS) disease other than stroke, such as tumor, trauma, hydrocephalus, or Parkinson’s disease; (3) severe cognitive impairment, as defined by a Mini-Mental State Examination (MMSE) [20] score of <19; (4) aphasia; (5) loss to follow-up; (6) physical frailty; (7) severe auditory or visual impairment; and (8) deceased or recurrent stroke prior to assessment.
The study protocol was approved by the Clinical Research Ethics Committee of the Chinese University of Hong Kong. All participants signed a consent form.
Collection of demographic and clinical data
During the acute stage, a research nurse collected subjects’ demographic data (age, sex, and education level in terms of school years) and assessed their stroke severity using the NIHSS [21].
Assessment of HRQoL
Three months after the onset of the index stroke, a trained research assistant, who was blind to the subjects’ radiological data, assessed all subjects with the Chinese (Hong Kong) version of the Short Form-36 (SF-36) [22], a valid and reliable instrument for measuring HRQoL in stroke [23]. The SF-36 focuses on subjective perceptions of health. It contains eight subscales that cover general health (GH), mental health (MH), role limitations due to emotional problems (RE), role limitations due to physical problems (RP), social functions (SF), vitality (VT), bodily pain (BP), and physical functioning (PF). The subscale scores range from 0 to 100, with higher values representing better functions. The SF-36 has two composite scores: the physical component (PCS) and mental component (MCS) summary scores [24]. The internal consistency of the SF-36 subscales is >0.70 [23, 24] and its test–retest reliability is 0.77 [25] in stroke. The SF-36 also has moderate to strong correlations with the Burden of Stroke Scale [26] and EuroQol [27].
The research assistant also administered the 15-item version of the Barthel Index (BI) [28], Geriatric Depression Scale (GDS) [29] and the MMSE to assess participants’ physical functioning, depressive symptoms and cognitive functioning, respectively. The GDS and MMSE scores range from 0 to 15 and 0 to 30, respectively. A higher GDS score indicates more severe depressive symptoms, whereas a lower MMSE score represents poorer global cognitive functioning.
MRI study
MRI was performed with a 1.5-T system (Sonata, Siemens Medical, Erlangen, Germany) within 7 days of admission. Diffusion weighted imaging (DWI) (TR/TE/excitation = 180/122/4, matrix = 128 × 128, field of view (FOV) = 230 mm, slice thickness/gap = 5 mm/1 mm, echo planar imaging (EPI) factor = 90, acquisition time = 55 s) with three orthogonally applied gradients (b values of 1,000, 500, and 0) was used. Other sequences included axial gradient echo (GRE) (TR/TE/excitation = 350/30/2, flip angle of 30°, slice thickness/gap = 5 mm/0.5 mm, FOV = 230 mm, matrix = 256 × 256, time of acquisition = 5 min, 4 s), axial spin echo (SE) T1-weighted (TR/TE/excitation = 425/14/2, FOV = 230 mm, slice thickness/gap = 5 mm/0.5 mm, matrix = 256 × 256, time of acquisition = 4 min, 28 s), turbo spin echo (TSE), proton density (PD), T2-weighted (TR/TE/excitation = 2,500/13-120/1, turbo factor = 5–15, FOV = 230 mm, slice thickness/gap = 5 mm/0.5 mm, matrix = 256 × 256, time of acquisition = 3 min, 30 s), and axial flair (fluid attenuated inversion recovery) (TR/TE/TI/excitation = 9,000/117/2,500/2, turbo factor = 31, FOV = 230 mm, slice thickness/gap = 5 mm/1 mm, matrix = 256 × 256, time of acquisition = 3 min, 20 s) sequences.
A neurologist (YKC), who was blind to the results of the other assessments, evaluated the MRIs for the following:
-
1)
Brain infarcts. Lesions approaching the signal characteristics of cerebrospinal fluid on the T1-weighted images and measuring over 3 mm in diameter were regarded as brain infarcts [30]. Both the number and volume of infarcts were measured. The total area of acute infarcts was measured with manual outlines of all areas with restricted water diffusion that were identified on the DWI with b values of 1,000. Their total volume was calculated by multiplying the total area by the sum of the slice thickness and gap. Inter- and intra-rater reliability tests were performed on 20 participants, with good agreement found (volume of acute infarcts: inter-rater κ = 0.93, intra-rater κ = 0.96; number of infarcts: inter-rater κ = 0.89, intra-rater κ = 0.94).
-
2)
WMH. The extent of WMH was graded using a modified version of Fazekas’ scale [31], which scores periventricular and deep WMH (PVWMH and DWMH) as mild, moderate, or severe [32]. The WMH was scored on the basis of the PD images. The inter- and intra-rater weighted kappas for the WMH were 0.85 and 0.90, respectively.
Statistical analysis
Descriptive data are presented as proportions or means, as appropriate. The correlation between the participants’ demographic and clinical (age, sex, education, and NIHSS, MMSE, and GDS scores) and radiological (number and volume of infarcts, and severity of WMH) characteristics and the SF-36 domain and summary scores were examined using Spearman’s correlation, except for the correlations between age and the SF-36 scores, which were examined with Pearson’s correlation because not all of the other variables were normally distributed. Both the unadjusted and Bonferroni-adjusted p values were computed. Variables with an unadjusted p < 0.05 were entered into different multivariate stepwise linear regression models to determine the partial correlations of the predictors of the SF-36 domain and summary scores. Two types of regression models were constructed. In the predictive models, only pre-index stroke factors, namely age, sex and education, marital status, previous stroke were considered. In the associative models, post-index stroke factors were also considered, including the NIHSS, MMSE, and GDS scores. Finally, age, sex, education years, number of old infarcts and two white matter intensity indicators were entered into the predictive model; age, sex, education years, GDS, MMSE, number of old infarcts and two white matter intensity indicators were entered into the associative model. All statistical tests were performed using SPSS for Windows (release 14.0; SPSS Inc., Chicago, IL, USA).
Results
The study sample of 160 subjects (Fig. 1) had the following characteristics: 61.9 % were male, 78.1 % were married and their mean age and education level were (mean ±standard deviation) 66.7 ±11.6 and 5.1 ±4.6 years, respectively; 99.8 % of the MRIs were obtained within 1 week of the index stroke. The mean DWMH and PVWMH Fazekas’ scores were 1.4 ±0.8 and 1.3 ±0.9, respectively. Twenty-three patients (14.4 %) scored 0; 83 (51.9 %) scored 1; 35 (21.9 %) scored 2; and 19 (11.9 %) scored 3 in the DWMH subscale, whereas 16 patients (10.0 %) scored 0; 83 (51.9 %) scored 1; 42 (26.3 %) scored 2; and 19 (11.9 %) scored 3 in the PVWMH subscale.
The psychiatric, social, and HRQoL assessments took place 14.6 ±2.5 weeks after the index stroke. The mean BI, MMSE, GDS, and NIHSS scores were 19.1 ±1.4, 23.2 ±3.0, 5.1 ±3.9, and 4.5 ±3.0, respectively. The PF, RP, BP, GH, VT, SF, RE, and MH subscales and PCS and MCS summary scores were 72.8 ±26.7, 60.0 ±41.4, 74.8 ±20.2, 51.7 ±21.1, 64.1 ±22.0, 90.4 ±15.4, 81.6 ±34.6, 73.6 ±18.6, 55.8 ±10.2, and 54.9 ±10.2, respectively.
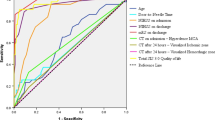
Univariate analyses revealed that female sex, depressive symptoms (GDS), and cognitive function (MMSE) were correlated with all eight subscales and the two summary scores (PCS and MCS; Table 1). Age, education, neurological deficits, physical functioning and cognitive function were also related to some, but not all, subscale and summary scores.
The severity of DWMH was negatively correlated with the VT, SF, RE, MH, and MCS scores, whereas the severity of PVWMH and number of old infarcts were negatively correlated with the SF and MH scores, respectively. After Bonferroni adjustment, only the correlations between the severity of DWMH and SF and MCS remained significant, whereas those between the severity of DWMH and RE and MH were of borderline significance (Table 2).
Predictive models were constructed for the VT, SF, RE, MH and MCS scores (Table 3), in which age, sex and education were entered if they were significant in the univariate analysis. The severity of DWMH was independently associated with these five scores (p < 0.05). In the subsequent associative model, BI, GDS and MMSE scores were also entered, and severity of DWMH remained associated with SF and MCS scores.
Discussion
To the best of our knowledge, this was the first study to examine the impact of WMH on HRQoL in lacunar stroke. The main finding is that DWMH is correlated with HRQoL in lacunar stroke survivors. The study sample comprised a cohort of stroke patients and the radiological findings were examined against the background of several clinical and psychosocial correlates of HRQoL (Table 4).
In this study, DMWH was associated with the mental aspect of HRQoL. No previous study has specifically considered the radiological correlates of HRQoL in lacunar stroke. Moon et al. [18] examined the MRI correlates of HRQoL in a small sample (n = 69) of ischemic stroke and did not find any association between DWMH and HRQoL. Another study revealed an association between WMH and both the physical (PF, RP, and PCS scores) and mental aspects of HRQoL (SF and RE scores) [19] in ischemic stroke.
WMH has a direct effect on cognitive impairment, depression, and functional outcome, thereby resulting in poorer HRQoL. Well-established white matter disease or subtle changes in white matter connectivity may lead to cognitive impairment in stroke [13]. WMH is also related to poor functional outcome in stroke [12, 15]. Finally, WMH is associated with depression in ischemic stroke [14, 33]. In the present study, only two SF-36 scores remained associated with DWMH after adjusting for depressive symptoms, a fact that suggests depression may be part of the link between DWMH and HRQoL.
If WMH does have a direct effect on HRQoL, then their location would be expected to play a part. Indeed, our findings suggest that only DWMH, and not PVWMH, are independent correlates of HRQoL. It has been suggested that DWMH is reflective of underlying vascular disease, whereas PVWMH is most strongly related to age [11]. Previous studies reported that only DWMH was associated with depression in stroke [14, 33]. Similarly, only DWMH predicted poor executive function in patients with mild cognitive impairment [34].
This study has several limitations. The assessment of HRQoL was made only once, at the 3-month follow-up. Hence, the causality of the relationship between the MRI findings and long-term HRQoL remains unknown. Patients without an MRI and those with more severe stroke resulting in prolonged hospitalization and physical frailty were excluded. Another limitation is that the SF-36 is a generic scale with a questionable validity in stroke [35]. Stroke-specific measures, such as the Stroke-Specific Quality of Life Scale [36], may have produced more valid information and should be used in future studies.
Conclusion
In conclusion, the results suggest that DWMH has an impact on the HRQoL of lacunar stroke survivors. The importance of DWMH in the long-term HRQoL in lacunar stroke warrants further investigation. In addition, the use of newer techniques such as diffusion tensor imaging should aid in better identification of white matter pathology.
References
Petty GW, Brown RDJ, Whisnant JP, Sicks JD, O’Fallon WM, Wiebers DO (2000) Ischemic stroke subtypes: a population-based study of functional outcome, survival, and recurrence. Stroke 31:1062–1068
Sacco S, Marini C, Totaro R, Russo T, Cerone D, Carolei A (2006) A population-based study of the incidence and prognosis of lacunar stroke. Neurology 66:1335–1338
de Haan RJ, Limburg M, Van der Meulen JNP, Jacobs HM, Aaronson NK (1995) Quality of life after stroke. Impact of stroke type and lesion location. Stroke 26:402–408
Kauhanen ML, Korpelainen JT, Nieminen P, Sotaniemi KA, Myllyla VV (2000) Domains and determinants of quality of life after stroke caused by brain infarction. Arch Phys Med Rehabil 81:1541–1546
Gray LJ, Sprigg N, Bath PM, Boysen G, De Deyn PP, Leys D et al (2007) Sex differences in quality of life in stroke survivors: data from the Tinzaparin in Acute Ischaemic Stroke Trial (TAIST). Stroke 38:2960–2964
Kim P, Warren S, Madil H, Hadley M (1999) Quality of life of stroke survivors. Qual Life Res 8:293–301
Jonkman EJ, Weerd AW, Virjens NLH (1998) Quality of life after a first ischemic stroke. Long-term developments and correlations with changes in neurological deficit, mood and cognitive impairment. Acta Neurol Scand 98:169–175
Patel MD, McKevitt C, Lawrence E, Rudd AG, Wolfe CD (2007) Clinical determinants of long-term quality of life after stroke. Age Ageing 36:316–322
Robinson-Smith G, Johnston MV, Allen J (2000) Self-care, quality of life, and depression after stroke. Arch Phys Med Rehabil 81:460–464
Herrmann LL, Le Masurier M, Ebmeier KP (2008) White matter hyperintensities in late life depression: a systematic review. J Neurol Neurosurg Psychiatry 79:619–624
Thomas AJ, O’Brien JT, Davis S, Ballard C, Barber R, Kalaria RN et al (2002) Ischemic basis for deep white matter hyperintensities in major depression: a neuropathological study. Arch Gen Psychiatry 59:785–792
Kissela B, Lindsell CJ, Kleindorfer D, Alwell K, Moomaw CJ, Woo D et al (2009) Clinical prediction of functional outcome after ischemic stroke: the surprising importance of periventricular white matter disease and race. Stroke 40:530–536
Gottesman RF, Hillis AE (2010) Predictors and assessment of cognitive dysfunction resulting from ischaemic stroke. Lancet Neurol 9:895–905
Tang WK, Chen YK, Lu JY, Chu WC, Mok VC, Ungvari GS et al (2010) White matter hyperintensities in post-stroke depression: a case control study. J Neurol Neurosurg Psychiatry 81:1312–1315
Liou LM, Chen CF, Guo YC, Cheng HL, Lee HL, Hsu JS et al (2010) Cerebral white matter hyperintensities predict functional stroke outcome. Cerebrovasc Dis 29:22–27
Grool AM, van der Graaf Y, Witkamp TD, Vincken KL, Mali WP, Geerlings MI (2011) Progression of white matter lesion volume and health-related quality of life in patients with symptomatic atherosclerotic disease: The SMART-MR Study. J Aging Res 2011:280630
Mowry EM, Beheshtian A, Waubant E, Goodin DS, Cree BA, Qualley P et al (2009) Quality of life in multiple sclerosis is associated with lesion burden and brain volume measures. Neurology 72:1760–1765
Moon YS, Kim SJ, Kim HC, Won MH, Kim DH (2004) Correlates of quality of life after stroke. J Neurol Sci 224:37–41
Tang WK, Chen YK, Lu J, Ahuja AT, Chu WC, Mok VC et al (2011) Cerebral microbleeds and quality of life in acute ischemic stroke. Neurol Sci 32:449–454
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Brott T, Adams H Jr, Olinger C, Marler JR, Barsan WG, Biller J et al (1989) Measurements of acute cerebral infarction: a clinical examination scale. Stroke 20:864–870
Lam CL, Gandek B, Ren XS, Chan MS (1998) Tests of scaling assumptions and construct validity of the Chinese (HK) version of the SF-36 Health Survey. J Clin Epidemiol 51:1139–1147
Anderson C, Laubscher S, Burns R (1996) Validation of the Short Form 36 (SF-36) health survey questionnaire among stroke patients. Stroke 27:1812–1816
Ware JE, Kosinski M, Gandek B (1993, 2000) SF-36® Health Survey: Manual & Interpretation Guide. QualityMetric Incorporated, Lincoln
Dorman P, Slattery J, Farrell B, Dennis M, Sandercock P (1998) Qualitative comparison of the reliability of health status assessments with the EuroQol and SF-36 questionnaires after stroke. United Kingdom Collaborators in the International Stroke Trial. Stroke 29:63–68
Doyle PJ, McNeil MR, Bost JE, Ross KB, Wambaugh JL, Hula WD, Mikolic JM (2007) The Burden of Stroke Scale (BOSS) provided valid, reliable, and responsive score estimates of functioning and well-being during the first year of recovery from stroke. Qual Life Res 16:1389–1398
Dorman PJ, Dennis M, Sandercock P (1999) How do scores on the EuroQol relate to scores on the SF-36 after stroke? Stroke 30:2146–2151
Mahoney F, Barthel D (1965) Functional evaluation: the Barthel Index. Md Med J 14:61–65
Lim PP, Ng LL, Chiam PC, Ong PS, Ngui FT, Sahadevan S (2000) Validation and comparison of three brief depression scales in an elderly Chinese population. Int J Geriatr Psychiatry 15:824–830
Jokinen H, Kalska H, Mäntylä R, Pohjasvaara T, Ylikoski R, Hietanen M et al (2006) Cognitive profile of subcortical ischaemic vascular disease. J Neurol Neurosurg Psychiatry 77:28–33
Firbank MJ, O’Brien JT, Pakrasi S, Pantoni L, Simoni M, Erkinjuntti T et al (2005) White matter hyperintensities and depression—preliminary results from the LADIS study. Int J Geriatr Psychiatry 20:674–679
Baezner H, Blahak C, Poggesi A, Pantoni L, Inzitari D, Chabriat H et al (2008) Association of gait and balance disorders with age-related white matter changes: the LADIS study. Neurology 70:935–942
Kim JT, Park MS, Yoon GJ, Jung HJ, Choi KH, Nam TS et al (2011) White matter hyperintensity as a factor associated with delayed mood disorders in patients with acute ischemic stroke. Eur Neurol 66:343–349
Delano-Wood L, Abeles N, Sacco JM, Wierenga CE, Horne NR, Bozoki A (2008) Regional white matter pathology in mild cognitive impairment: differential influence of lesion type on neuropsychological functioning. Stroke 39:794–799
Hobart JC, Williams LS, Moran K, Thompson AJ (2002) Quality of life measurement after stroke: uses and abuses of the SF-36. Stroke 33:1348–1356
Mok VC, Lam WW, Fan YH, Wong A, Ng PW, Tsoi TH et al (2009) Effects of statins on the progression of cerebral white matter lesion: post hoc analysis of the ROCAS (Regression of Cerebral Artery Stenosis) study. J Neurol 256:750–757
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tang, W.K., Liang, H.J., Chen, Y.K. et al. White matter hyperintensities and quality of life in acute lacunar stroke. Neurol Sci 34, 1347–1353 (2013). https://doi.org/10.1007/s10072-012-1267-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-012-1267-7