Abstract
This study evaluated the impact of cerebral microbleeds (CMBs) on the health-related quality of life (HRQoL) in 458 Chinese patients with first or recurrent acute ischemic stroke. HRQoL was assessed with the Short Form-36 (SF-36). Univariate analysis showed the presence of lobar CMBs to be negatively correlated with patients’ physical functioning (PF; p < 0.01), social function (SF; p < 0.01), and role-emotional (RE; p < 0.05) scores. Subsequent linear regression analysis revealed lobar CMBs to be independently associated with the PF and SF scores (p < 0.05). The limitations of this study include the exclusion of patients with more severe stroke, the lack of longitudinal assessments, the use of a generic rather than stroke-specific HRQoL scale, and the less than optimal sensitivity of the CMB measurement. The study findings suggest that CMBs have a significant impact on the HRQoL of stroke survivors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cerebral microbleeds (CMBs) are primarily a radiological construct (small MRI signal voids) indicative of specific underlying microscopic pathological changes, i.e., perivascular collections of hemosiderin deposits that indicate prior micro-hemorrhages [1]. Histopathological analyses of CMBs generally reveal two types of vascular pathological changes: hypertensive vasculopathy and cerebral amyloid angiopathy. The distribution of CMBs is different in these two disorders: lobar CMBs are associated with cerebral amyloid angiopathy, whereas deep CMBs are associated with hypertensive vasculopathy [1, 2].
The prevailing view is that microbleeds are clinically silent [3]. However, recent histopathological data have revealed that CMBs are not only circumscribed hemosiderin deposits, but also affect the surrounding gliosis and cause frank necrosis or microinfarctions, which suggests that they may be of clinical importance [4]. Recent evidence also suggests that CMBs may be an important factor in cognitive impairments in subcortical vascular dementia [5], where they are associated with cognitive dysfunction, particularly executive dysfunction [6]. CMBs are common in ischemic stroke [7], and they may predict the recurrence of stroke [8] and the emergence of emotional lability [9]. These microbleeds are also associated with factors that may affect health-related quality of life (HRQoL) in stroke, including advanced small artery disease of the brain [3], leukoaraiosis [10], and recurrent stroke [8].
Patients with stroke have been shown to have poor HRQoL [11]. The correlates of poor HRQoL 1 month to 3 years after stroke include an older age [10, 11], the female sex [12], being single or widowed [13], a lack of social support [14], a high degree of neurological deficit [15], cognitive impairment [16], and depression [17].
Data on the impact of infarcts and other radiological findings on HRQoL are limited, although large lesion volumes [18] have been found to predict poor HRQoL following stroke [19]. To date, only one study has examined the role that acute infarct location and white matter lesions (WMLs) play in HRQoL, with no correlation found between either lesion location or WMLs and HRQoL [19].
To the best of our knowledge, no data have been published on the impact of CMBs on the HRQoL of stroke patients, and hence their effect on HRQoL in stroke remains unknown. This study set out to examine whether the presence or location of CMBs contributes to HRQoL in acute ischemic stroke survivors.
Materials and methods
Subjects
Of the 2,337 patients admitted with first-ever or recurrent stroke to the Acute Stroke Unit (ASU) of the Prince of Wales Hospital (PWH)—a university-affiliated general hospital serving a population of 800,000 in Hong Kong—from December 2004 to May 2007, 874 received an MRI examination. Due to limited access to an MRI machine, MRI is generally reserved for stroke patients with stable neurological conditions. Compared to patients who did not receive an MRI examination, those who did had a lower mean age (67.8 + 12.1 vs. 74.5 + 12.0; p < 0.001) and less severe stroke, as reflected by a lower National Institutes of Health Stroke Scale (NIHSS) score (5.6 + 4.6 vs. 10.6 + 9.8, p < 0.001), and were more likely to be men (58.8 vs. 46.6%; p < 0.001). Four hundred and fifty-eight (52.2%) patients who had received an MRI were recruited for the study. The inclusion criteria were (1) Chinese ethnicity; (2) aged 18 or above; (3) well-documented (clinical presentation and CT scan of the brain) first or recurrent acute stroke occurring within the 7 days prior to admission; (4) Cantonese dialect as the primary language; and (5) ability and willingness to give consent. The exclusion criteria included: (1) transient ischemic attack, cerebral hemorrhage, subdural hematoma, or subarachnoid hemorrhage; (2) history of a central nervous system (CNS) disease other than stroke, such as tumor, trauma, hydrocephalus, or Parkinson’s disease; (3) severe cognitive impairment, as defined by a Mini-Mental State Examination (MMSE) [20] score of <19; (4) aphasia; and (5) medical conditions that would preclude follow-up 3 months after the index stroke, such as recurrent stroke, prolonged hospitalization (>3 months), and physical frailty.
The study protocol was approved by the Clinical Research Ethics Committee of the Chinese University of Hong Kong. All participants signed a consent form.
Collection of demographic and clinical data
A research nurse collected subjects’ demographic data (age, sex, and educational level in terms of school years) and assessed their stroke severity using the NIHSS [21].
Assessment of HRQoL
Three months after the onset of the index stroke, a trained research assistant, who was blind to the subjects’ radiological data, assessed all participants in a research clinic with the Chinese (Hong Kong) version of the Short Form-36 (SF-36) [22], a valid and reliable instrument for measuring HRQoL in stroke [23]. The SF-36 focuses on subjective perceptions of health. It contains eight subscales that cover general health (GH), mental health (MH), role limitations due to emotional problems (RE), role limitations due to physical problems (RP), social functions (SF), vitality (VT), bodily pain (BP), and physical functioning (PF). The subscale scores range from 0 to 100, with higher values representing better functions. The SF-36 has two composite scores: the physical component (PCS) and mental component (MCS) summary scores.
The research assistant also administered the 15-item version of the Geriatric Depression Scale (GDS) [24], the MMSE, and the Lubben Social Network Scale (LSNS) [25] to assess participants’ depressive symptoms, cognitive functioning, and degree of social support, respectively. The GDS and MMSE scores range from 0 to 15 and 0 to 30, respectively. A higher GDS score indicates more severe depressive symptoms, whereas a lower MMSE score represents poorer global cognitive functioning. The LSNS is a composite social network scale that was specifically designed for use in the elderly [26]. It measures the level of social support that patients receive and their degree of social interaction with relatives and friends. The maximum score is 50, with a higher score indicating better social support.
Radiological examination
MRI was performed with a 1.5 T system (Sonata, Siemens Medical, Erlangen, Germany) within 7 days of admission. Diffusion weighted imaging (DWI) (TR/TE/excitation = 180/122/4, matrix = 128 × 128, field of view (FOV) = 230 mm, slice thickness/gap = 5 mm/1 mm, echo planar imaging (EPI) factor = 90, acquisition time = 55 s) with three orthogonally applied gradients (b values of 1,000, 500, and 0) was used. Other sequences included axial gradient echo (GRE) (TR/TE/excitation = 350/30/2, flip angle of 30°, slice thickness/gap = 5 mm/0.5 mm, FOV = 230 mm, matrix = 256 × 256, time of acquisition = 5 min, 4 s), axial spin echo (SE) T1-weighted (TR/TE/excitation = 425/14/2, FOV = 230 mm, slice thickness/gap = 5 mm/0.5 mm, matrix = 256 × 256, time of acquisition = 4 min, 28 s), turbo spin echo (TSE), proton density (PD), T2-weighted (TR/TE/excitation = 2500/13-120/1, turbo factor = 5–15, FOV = 230 mm, slice thickness/gap = 5 mm/0.5 mm, matrix = 256 × 256, time of acquisition = 3 min, 30 s), and axial flair (fluid attenuated inversion recovery) (TR/TE/TI/excitation = 9000/117/2500/2, turbo factor = 31, FOV = 230 mm, slice thickness/gap = 5 mm/1 mm, matrix = 256 × 256, time of acquisition = 3 min, 20 s) sequences.
A neurologist (YKC), who was blind to the results of the other assessments, evaluated the MRIs for the following.
-
1.
Brain infarcts Lesions approaching the signal characteristics of cerebrospinal fluid on the T1-weighted images and measuring over 3 mm in diameter were regarded as brain infarcts [27]. Both the number and size of infarcts were measured. The total area of acute infarcts was measured with manual outlines of all areas with restricted water diffusion that were identified on the DWI with b values of 1,000. Their total volume was calculated by multiplying the total area by the sum of the slice thickness and gap. Inter- and intra-rater reliability tests were performed on 20 participants, with good agreement found (volume of acute infarcts: inter-rater kappa = 0.93, intra-rater kappa = 0.96; number of infarcts: inter-rater kappa = 0.89, intra-rater kappa = 0.94).
-
2.
CMBs CMBs were defined as small (2–10 mm) hypointense lesions on the T2*-weighted GRE sequence, but symmetric basal ganglia calcification and flow void artifacts of the pial blood vessels were excluded [28]. The CMB locations were divided into lobar (cortex and sub-cortical white matter), deep (caudate, lentiform, thalamus, internal, and external capsule), and posterior fossa (brainstem and cerebellum) groups [29]. The number of CMBs in each region was also recorded. Intra-rater reliability tests of the CMB measurements were performed on 30 participants, with good agreement found [presence of CMBs: intra-rater kappa = 0.85; number of CMBs: intra-rater intra-class correlation (ICC) = 0.95].
-
3.
WMLs The extent of WMLs was graded using a modified version of Fazekas’ scale [30], which scores deep and subcortical WMLs as mild, moderate, or severe [31]. The WMLs were scored on the basis of the PD images. The inter- and intra-rater weighted kappas for the WMLs were 0.85 and 0.90, respectively.
Statistical analysis
Descriptive data are presented as proportions or means, as appropriate. The correlation between the participants’ clinical (age, sex, education, NIHSS, MMSE, and GDS scores) and radiological (number and volume of infarcts, presence of CMBs, and severity of WMLs) characteristics and the SF-36 domain and summary scores were examined using Spearman’s correlation, except for the correlations between age and the SF-36 scores, which were examined with Pearson’s correlation because not all of the other variables were normally distributed. Both the unadjusted and Bonferroni-adjusted p values were computed. Variables with an unadjusted p < 0.05 in these analyses were entered into different multivariate stepwise linear regression models to determine the partial correlations of the predictors of the SF-36 domain and summary scores. All statistical tests were performed using SPSS for Windows (Release 14.0; SPSS Inc., Chicago, IL, USA).
Results
The study sample (n = 458) had the following characteristics: 74.5% were married, and their mean age and educational level were 66.2 + 11.9 and 5.2 + 4.5 years, respectively; 99.8% of the MRIs were obtained within 1 week of the stroke. The mean number and volume of acute infarcts were 1.1 + 1.7 and 3.0 + 9.3 ml, respectively. CMBs were found in 111 (24.2%) participants, and the mean number of CMBs was 5.6 + 8.7. A significant correlation was found between the volume of acute infarcts and the presence of CMBs (rho = 0.269, p < 0.001).
The psychiatric, social, and HRQoL assessments took place 14.6 + 2.0 weeks after the index stroke. The mean MMSE, GDS, LSNS, and NIHSS scores were 25.9 + 3.3, 5.0 + 3.7, 30.4 + 8.0, and 4.7 + 3.4, respectively. The PF, RP, BP, GH, VT, SF, RE, and MH subscale scores were 71.6 ± 27.9, 58.1 ± 41.4, 77.5 ± 24.6, 49.8 ± 20.6, 64.6 ± 21.3, 89.9 ± 15.6, 80.0 ± 35.0, and 73.5 ± 19.4, respectively.
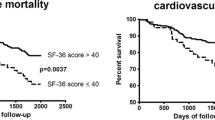
Univariate analyses revealed that the female sex, education, neurological deficits (NIHSS), depressive symptoms (GDS), and cognitive function (MMSE) were correlated with all eight subscale and two summary scores (PCS and MCS; Table 1). The presence of lobar CMBs was negatively correlated with the PF, SF, RE, and PCS scores. After Bonferroni adjustment, the correlation between lobar CMBs and PF remained significant, whereas those between lobar CMBs and SF and RE became borderline and nonsignificant, respectively. Deep CMBs were also negatively correlated with the SF and RE scores, whereas posterior fossa CMBs were negatively correlated with the RP score. The severity of WMLs was correlated with four of the SF-36 subscale scores and the PCS score, whereas the number of old infarcts was correlated with the PF and RP scores of the SF-36 (Table 2).
Linear regression analysis was performed for the PF, SF, RE, RP, PCS, and MCS scores (Table 3), and the presence of lobar CMBs was found to be independently associated with the PF and SF scores (p < 0.05).
Discussion
To the best of our knowledge, this study was the first to examine the impact of CMBs on the HRQoL of stroke patients. The results show that lobar CMBs are correlated with HRQoL in stroke survivors. The study sample comprised a large cohort of stroke patients, and the radiological findings were examined against the background of several clinical and psychosocial correlates of HRQoL.
In addition to being a marker of underlying vascular disease, CMBs may also have a direct effect on neurological function, cognition, psychiatric morbidity, and disability, thereby resulting in poorer HRQoL. A higher number of baseline CMBs was associated with the greater risk of cognitive impairment, functional dependence, and death in a 3-year prospective study of patients with lobar hemorrhages [32]. CMBs have also been associated with executive function impairment in patients with ischemic stroke [6]. Finally, CMBs are known to be an independent correlate of emotional liability in stroke [9].
If CMBs do have a direct effect on HRQoL, then their location would be expected to play a part. Indeed, our findings suggest that only lobar, not deep or posterior fossa, CMBs are independent correlates of HRQoL. This finding also suggests that the CMBs associated with cerebral amyloid angiopathy, which has a lobar distribution, may have a greater impact on HRQoL in stroke. The importance of CMB location has been reported previously in studies of the effects of frontal lobe and basal ganglia CMBs on executive function [6] and thalamic CMBs on emotional liability [9].
The current study has several limitations. The assessment of PSD was made only once, at the 3-month follow-up. Hence, the causality of the relationship between the MRI findings and the long-term HRQoL remains unknown. Moreover, patients who did not receive an MRI examination and those with more severe stroke resulting in prolonged hospitalization and physical frailty were excluded. Another limitation is that the SF-36 is a generic scale, and some investigators have questioned its validity in stroke [33]. Stroke-specific measures, such as the Stroke-Specific Quality of Life Scale, may have produced more valid information and should be used in future studies. Finally, the CMBs were measured in GRE with a slice thickness of 5 mm, which is less sensitive than thin-section susceptibility-weighted imaging [34].
In summary, the results of this study suggest that lobar CMBs have an impact on the HRQoL of stroke survivors. The importance of CMBs to other short- and long-term outcome measures in stroke warrants further investigation.
References
Greenberg SM, Vernooij MWV, Cordonnier C, Viswanathan A, Al-Shahi Salman R, Warach S, Launer LJ, Van Buchem M, Breteler MM (2009) Cerebral microbleeds: a guide to detection and interpretation. Lancet Neurol 8:165–174
Knudsen KA, Rosand J, Karluk D, Greenberg SM (2001) Clinical diagnosis of cerebral amyloid angiopathy: validation of the Boston criteria. Neurology 56:537–539
Kato H, Izumiyama M, Izumiyama K, Takahashi A, Itoyama Y (2002) Silent cerebral microbleeds on T2*-weighted MRI: correlation with stroke subtype, stroke recurrence, and leukoaraiosis. Stroke 33:1536–1540
Tanaka A, Ueno Y, Nakayama Y, Takano K, Takebayashi S (1999) Small chronic hemorrhages and ischemic lesions in association with spontaneous intracerebral hematomas. Stroke 30:1637–1642
Won SS, Hwa LB, Kim EJ, Chin J, Sun Cho Y, Yoon U, Na DL (2007) Clinical significance of microbleeds in subcortical vascular dementia. Stroke 38:1949–1951
Werring DJ, Frazer DW, Coward LJ, Losseff NA, Watt H, Cipolotti L, Brown MM, Jäger HR (2004) Cognitive dysfunction in patients with cerebral microbleeds on T2*-weighted gradient-echo MRI. Brain 127:2265–2275
Werring DJ, Coward LJ, Losseff NA, Jäger HR, Brown MM (2005) Cerebral microbleeds are common in ischemic stroke but rare in TIA. Neurology 65:1914–1918
Naka H, Nomura E, Takahashi T, Wakabayashi S, Mimori Y, Kajikawa H, Kohriyama T, Matsumoto M (2006) Combinations of the presence or absence of cerebral microbleeds and advanced white matter hyperintensity as predictors of subsequent stroke types. Am J Neuroradiol 27:830–835
Tang WK, Chen YK, Lu JY, Mok V, Xiang Y, Ungvari GS, Ahuja AT, Wong KS (2009) Microbleeds and Post-stroke Emotional Incontinence. J Neurol Neurosurg Psychiatry 10:1082–1086
Gao T, Wang Y, Zhang Z (2008) Silent cerebral microbleeds on susceptibility-weighted imaging of patients with ischemic stroke and leukoaraiosis. Neurol Res 30:272–276
Kauhanen ML, Korpelainen JT, Nieminen P, Sotaniemi KA, Myllyla VV (2000) Domains and determinants of quality of life after stroke caused by brain infarction. Arch Phys Med Rehabil 81:1541–1546
Gray LJ, Sprigg N, Bath PM, Boysen G, De Deyn PP, Leys D, O’Neill D, Ringelstein EB, TAIST Investigators (2007) Sex differences in quality of life in stroke survivors: data from the Tinzaparin in Acute Ischaemic Stroke Trial (TAIST). Stroke 38:2960–2964
Kim P, Warren S, Madil H, Hadley M (1999) Quality of life of stroke survivors. Qual Life Res 8:293–301
Lynch EB, Butt Z, Heinemann A, Victorson D, Nowinski CJ, Perez L, Cella D (2009) A qualitative study of quality of life after stroke: the importance of social relationships. J Rehabil Med 40:518–523
Jonkman EJ, Weerd AW, Virjens NLH (1998) Quality of life after a first ischemic stroke. Long-term developments and correlations with changes in neurological deficit, mood and cognitive impairment. Acta Neurol Scand 175:169–175
Patel MD, McKevitt C, Lawrence E, Rudd AG, Wolfe CD (2007) Clinical determinants of long-term quality of life after stroke. Age Ageing 36:316–322
Robinson-Smith G, Johnston MV, Allen J (2000) Self-care, quality of life, and depression after stroke. Arch Phys Med Rehabil 81:460–464
Schiemanck SK, Post MW, Kwakkel G, Witkamp TD, Kappelle LJ, Prevo AJ (2005) Ischemic lesion volume correlates with long-term functional outcome and quality of life of middle cerebral artery stroke survivors. Restor Neurol Neurosci 23:257–263
Moon YS, Kim SJ, Kim HC, Won MH, Kim DH (2004) Correlates of quality of life after stroke. J Neurol Sci 224:37–41
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Brott T, Adams HP Jr, Olinger CP (1989) Measurement of acute cerebral infarctions: a clinical examination scale. Stroke 20:864–870
Lam CL, Gandek B, Ren XS, Chan MS (1998) Tests of scaling assumptions and construct validity of the Chinese (HK) version of the SF-36 Health Survey. J Clin Epidemiol 51:1139–1147
Anderson C, Laubscher S, Burns R (1996) Validation of the Short Form 36 (SF-36) health survey questionnaire among stroke patients. Stroke 27:1812–1816
Lim PP, Ng LL, Chiam PC, Ong PS, Ngui FT, Sahadevan S (2000) Validation and comparison of three brief depression scales in an elderly Chinese population. Int J Geriatr Psychiatry 15:824–830
Lubben JE (1998) Assessing social network among elderly populations. Fam Community Health 11:42–52
Chi I, Boey KW (1994) A mental health and social support study of the old-old in Hong Kong. Resource Paper Series No. 22. Department of Social Work and Social Administration, the University of Hong Kong
Jokinen H, Kalska H, Mäntylä R, Pohjasvaara T, Ylikoski R, Hietanen M, Salonen O, Kaste M, Erkinjuntti T (2006) Cognitive profile of subcortical ischaemic vascular disease. J Neurol Neurosurg Psychiatry 77:28–33
Dichgans M, Holtmannspotter M, Herzog J, Peters N, Bergmann M, Yousry TA (2002) Cerebral microbleeds in CADASIL: a gradient-echo magnetic resonance imaging and autopsy study. Stroke 33:67–71
Cordonnier C, Potter GM, Jackson CA, Doubal F, Keir S, Sudlow CL, Wardlaw JM, Al-Shahi Salman R (2009) Improving Interrater Agreement about Brain Microbleeds. Development of the Brain Observer MicroBleed Scale (BOMBS). Stroke 40:94–99
Firbank MJ, O’Brien JT, Pakrasi S, Pantoni L, Simoni M, Erkinjuntti T, Wallin A, Wahlund LO, van Straaten I, Inzitari D (2005) White matter hyperintensities and depression—preliminary results from the LADIS study. Int J Geriatr Psychiatry 20:674–679
Baezner H, Blahak C, Poggesi A, Pantoni L, Inzitari D, Chabriat H, Erkinjuntti T, Fazekas F, Ferro JM, Langhorne P, O’Brien J, Scheltens P, Visser MC, Wahlund LO, Waldemar G, Wallin A, Hennerici MG, LADIS Study Group (2008) Association of gait and balance disorders with age-related white matter changes: the LADIS study. Neurology 70:935–942
Greenberg SM, Eng JA, Ning M, Smith EE, Rosand J (2004) Hemorrhage burden predicts recurrent intracerebral hemorrhage after lobar hemorrhage. Stroke 35:1415–1420
Hobart JC, Williams LS, Moran K, Thompson AJ (2002) Quality of life measurement after stroke: uses and abuses of the SF-36. Stroke 33:1348–1356
Nandigam RN, Viswanathan A, Delgado P, Skehan M, Smith EE, Rosand J, Greenberg SM, Dickerson BC (2009) MR imaging detection of cerebral microbleeds: effect of susceptibility-weighted imaging, section thickness, and field strength. AJNR 30:338–343
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tang, W.K., Chen, Y.K., Lu, J. et al. Cerebral microbleeds and quality of life in acute ischemic stroke. Neurol Sci 32, 449–454 (2011). https://doi.org/10.1007/s10072-011-0571-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-011-0571-y