Abstract
A 67-year-old man complained of a transient blurring of vision in his right visual field lasting 30 min followed by headache. Two weeks later, the visual disturbance changed its pattern; it was described as the occurrence of brown round-shaped images in the right visual field spinning and turning for few seconds. This evolution from visual aura to visual seizures, with video-EEG correlation, supports the hypothesis of modification in threshold of cortical hyperexcitability from migraine to epilepsy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Migraine and epilepsy represent two distinct paroxysmal neurological conditions characterized by peculiar clinical features and a comorbidity. Their possible relationship was advanced since nineteenth century, but the mechanisms underlying this association are still not clear. A neural hyperexcitability due to ionic channels alterations should be the shared pathophysiological mechanism [1]. It has been hypothesized that the occipital cortex in migraineurs presents a low excitation threshold, which may trigger the seizure. Cortical spreading depression (CSD), a phenomenon due to abnormal activation of neuronal occipital cortex, originally demonstrated by Aristides Leão in 1944, is reputed to be the neurophysiological correlate of visual aura [2]. This consists in a short-lasting depolarization wave moving across the cortex at a rate of 3–5 mm/min. The neuronal excitation along the front of progression is immediately followed by synchronous and prolonged nerve cell depression which correlates with a dramatic failure of brain ion homeostasis, efflux of excitatory amino acids from nerve cells and enhanced energy metabolism. The result of such activities is a reduction of the brain perfusion [2, 3]. Functional neuroimaging studies have provided that the visual aura in migraineurs is correlated with CSD-like phenomena in occipital lobe [4, 5]. Moreover, migraine-like headache is not uncommon following a seizure, the latter rarely appears during or after a migraine attack. Nevertheless, the occurrence of an epileptic seizure during or shortly after the resolution of a migraine aura is a well-known phenomenon, called “migralepsy” [6, 7], and its diagnostic criteria appears in the second edition of the International Classification of Headache Disorders (ICHD-II). A recent review of cases of “migralepsy” puts the light on the absence of ictal EEG recording during the first phase of migraine triggered seizure attack and on the lack of accuracy in the current ICHD-II criteria [8].
Case report
A 67-year-old man suffered since his twenties from infrequent bifrontal throbbing headache attacks, associated with nausea, phono-, photo-, and osmophobia, usually lasting 1–2 days and responding fairly to NSAIDs. The frequency of these migraine without aura attacks decreased over the years reaching the average frequency of three or four attacks per year. These attacks were never preceded by visual disturbance or other symptoms fulfilling the ICHD-II criteria for typical aura symptoms (coded 1.2.1).
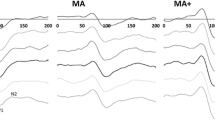
He complained of a transient blurring of vision in his right visual field, which gradually developed in about 10 min and lasted 30 min fulfilling the criteria for typical visual aura. A moderate, pulsating, left fronto-temporal pain associated with phonophobia, photophobia and nausea followed the resolution of the visual deficit, and disappeared in a few hours. Neurological evaluation revealed the presence of a restricted right lateral homonymous visual field; no sensitive or motor deficit was detected. Meanwhile, episodes with the same features, formally fulfilling ICHD-II diagnostic criteria for migraine with aura, persisted with a mean frequency of 1–2/day. A cerebral CT performed 2 weeks after the first visual symptom documented the presence of a hypodense lesion in the left occipital lobe; a cerebral MR with gadolinium showed a contrast-enhanced infiltrating lesion in the left occipital lobe. During hospitalization, the visual disturbance changed its pattern. It was described as a round-shaped image in the right visual field, lasting 30–40 min which sometimes suddenly spun and turned every 2–3 s for 10–20 s. A headache attack with the usual features occurred at the resolution of the visual disturbance. The patient underwent a prolonged video-EEG registration. The interictal EEG showed slow activity in the left parietal and occipital region; there was no activation with intermittent photic stimulation or hyperventilation. In concomitance with the visual disorder, bursts of slow theta and delta waves appeared in the left parietal and occipital region, with appearance of sharp waves, and rhythmic theta, and delta waves when the visual hallucination spun and turned (Fig. 1). The patient never had diplopia, no sensation of ocular movement and the video-EEG registration excluded deviation of the eyes, eyelids or palpebral jerks during the visual disturbance. He underwent to the surgical resection of the lesion, with the definitive diagnosis of glioblastoma multiforme.
Discussion
According to ICHD-II, this case cannot be diagnosed as a “pure” migraine with aura since the neurological examination was not normal and an underlying structural lesion was documented. It becomes a case of symptomatic visual aura with the initial clinical features that resemble typical aura symptoms in migraine. Typical migraine-like visual aura have been reported to occur with a variety of cerebral lesions; however, not all patients with migraine-like visual phenomena can be correctly diagnosed using clinical criteria alone [9].
The evolution from visual aura to visual seizures in our patient with an organic pathology involving the occipital lobe supports the hypothesis of some common pathophysiological mechanisms in migraine and epilepsy. The hypothetical common pathogenesis of these two neurological diseases is still based only on assumptions. Many studies have supported the hypothesis of a cortical hyperexcitability as the main pathological mechanism [1]. The abnormal neuronal excitability in the cerebral cortex could be sustained by different factors, such as alteration of ion channels, reduction of levels of magnesium, increased release of excitatory neurotransmitters [3]. All these elements may account for the propensity to develop both migraine and epilepsy in the same individual. Evidence suggests that co-morbid migraine is associated with a worse prognosis of epilepsy; in a prospective study it was found that epilepsy-migraine patients had a longer duration of the disease and a lower response to antiepileptic treatment than patients with epilepsy without migraine [10].
The interictal EEGs of many migraine patients contain mild slow abnormalities, involving the parieto-occipital regions. These slow activity should increase even more just before the headache attack in the same patients. Bjørk and co-workers [11] found that delta activity was increased even before pain onset on the affected side in migraineurs. Furthermore, alpha rhythm changes were observed along the migraine cycle, correlated with increasing disease and attack duration [12]. These findings may suggest that migraineurs present a slight brain dysfunction between attacks which would be in line with the hypothesis that the accumulated abnormalities modify the physiology of the visual cortex or the brainstem. EEG is not useful in migraine diagnosis with the exception of situations in which seizure disorders are to be excluded, such as migraine-triggered seizure and in patients with recurrent episodes of atypical aura (i.e. aura with brief duration or with sudden appearance of neurological symptom), or high frequency aura. Recently, Parisi and co-workers [13] described a case of atypical childhood occipital epilepsy “Gastaut type” whose first generalized tonic–clonic seizure was preceded by migraine without aura and followed by migraine-like headache which lasted for 3 days; occipital status epilepticus occurred during the migraine attack with electroclinical resolution after intravenous administration of 10 mg diazepam. In our case we did not administer diazepam because we wanted to see the spontaneous resolution of the visual disturbance, lasting about 30 min.
During the initial visual disturbance of our patient, clinically classifiable as typical aura, the EEG showed slow waves in the left temporal posterior derivation. Subsequently the EEG showed burst of sharp waves and rhythmic delta waves when the image suddenly turned (Fig. 1 ). The observations in this patient with initially migraine without aura and the event of occipital organic lesion provoke the continuum of expression of related pathology with increasing threshold like migraine with aura and occipital seizures.
Recent imaging studies in migraine without aura also point to the presence of silent cortical spreading depression as an underlying mechanism in migraine without aura [14]. Based on the clinical observation, migraine with aura vary for duration, frequency and severity of aura symptoms from patients to patients and also within the same patient in different attacks. Considering that the CSD is an all-or-nothing event and not a multigradient event, a clinical expression threshold was proposed to clarify why patients suffering from migraine have aura or not; depending on the patient sensitivity, the pathological process in migraine would be translated into symptoms [15, 16].
Conclusion
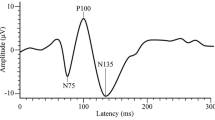
We assume that a clinical threshold modification happened in our patient, from an history of migraine without aura where we had a silent CSD, to attacks of migraine with aura where the CSD has a clinical expression; the subsequent appearance of a seizure was a further modification of the clinical expression threshold of CSD (Fig. 2). Although this is a symptomatic case, we assume that it can represent what occurs during an attack of migraine-triggered seizure. We would therefore stress recording of ictal EEG in patients with migraine-triggered seizure for a better knowledge of this clinical condition and for a better knowledge of the overlap between migraine and epilepsy.
References
Dainese F, Paladin F (2009) Genetic determinants of the migraine-epilepsy association. In: Avanzini G, Noebels J (eds) Genetics of epilepsy and genetic epilepsies. John Libbey Eurotext, Montrouge, pp 89–98
Somjen GG (2001) Mechanisms of spreading depression and hypoxic spreading depression-like depolarization. Physiol Rev 81:1065–1096
Welch KM (2005) Brain hyperexcitability: the basis for antiepileptic drugs in migraine prevention. Headache 45(Suppl 1):25–32
Bowyer SM, Aurora KS, Moran JE, Tepley N, Welch KM (2001) Magnetoencephalographic fields from patients with spontaneous and induced migraine aura. Ann Neurol 50:582–587
Hadjikhani N, Sanchez Del Rio M, Wu O, Schwartz D, Bakker D, Fischl B, Kwong KK, Cutrer FM, Rosen BR, Tootell RB, Sorensen AG, Moskowitz MA (2001) Mechanisms of migraine aura revealed by functional MRI in human visual cortex. Proc Natl Acad Sci U S A 98:4687–4692
Headache Classification Subcommittee of the International Headache Society (2004) The international classification of headache disorders, 2nd edn. Cephalalgia 24(Suppl 1):1–160
Maggioni F, Mampreso E, Ruffatti S, Viaro F, Lunardelli V, Zanchin G (2008) Migralepsy: is the current definition too narrow? Headache 48:1129–1132
Sances G, Guaschino E, Perucca P, Allena M, Ghiotto N, Manni R (2009) Migralepsy: a call for a revision of the definition. Epilepsia 50:2487–2496
Shams PN, Plant GT (2011) Migraine-like visual aura due to focal cerebral lesions: case series and review. Surv Ophthalmol 56(2):135–161
Velioğlu SK, Boz C, Özmenoğlu M (2005) The impact of migraine on epilepsy: a prospective prognosis study. Cephalalgia 25:528–535
Bjørk MH, Stovner LJ, Engstrøm M, Stjern M, Hagen K, Sand T (2009) Interictal quantitative EEG in migraine: a blinded controlled study. J Headache Pain 10:331–339
Bjørk MH, Stovner LJ, Nilsen BM, Stjern M, Hagen K, Sand T (2009) The occipital alpha rhythm related to the “migraine cycle” and headache burden: a blinded, controlled longitudinal study. Clin Neurophysiol 120:464–471
Parisi P, Kasteleijn-Nolst Trenité DG, Piccioli M, Pelliccia A, Luchetti A, Buttinelli C, Villa MP (2007) A case with atypical childhood occipital epilepsy “Gastaut type”: an ictal migraine manifestation with a good response to intravenous diazepam. Epilepsia 48:2181–2186
Sanchez-del-Rio M, Reuter U, Moskowitz MA (2006) New insights into migraine pathophysiology. Curr Opin Neurol 19:294–298
Vincent MB, Hadjikhani N (2007) Migraine aura and related phenomena: beyond scotomata and scintillations. Cephalalgia 27:1368–1377
Parisi P (2009) Why is migraine rarely, and not usually, the sole ictal epileptic manifestation? Seizure 18:309–312
Acknowledgments
We thank Mrs. Boriana S. Gagaouzova for editing and review of the manuscript.
Conflict of interest
None of the authors has any conflict of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dainese, F., Mainardi, F., Zanchin, G. et al. From migraine to epilepsy: a threshold mechanism?. Neurol Sci 33, 915–918 (2012). https://doi.org/10.1007/s10072-011-0851-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-011-0851-6