Abstract
Ataxia with vitamin E deficiency (AVED) is a rare autosomal recessive neurodegenerative disease, due to mutations in TTPA gene (Arita et al. in Biochem J 306(Pt. 2):437–443, 1995; Hentati et al. in Ann Neurol 39:295–300, 1996), which encodes for α-TTP, a cytosolic liver protein that is presumed to function in the intracellular transport of α-tocopherol. This disease is characterized clinically by symptoms with often striking resemblance to those of Friedreich ataxia. The neurological symptoms include ataxia, dysarthria, hyporeflexia, and decreased vibration sense, sometimes associated with cardiomyopathy and retinitis pigmentosa (Mariotti et al. in Neurol Sci 25:130–137, 2004). Vitamin E supplementation improves symptoms and prevents disease progress (Doria-Lamba et al. in Eur J Pediatr 165(7):494–495, 2006). Over 20 mutations have been identified in patients with AVED. In the present paper we summarize the recent findings on molecular genetic of this disease including the list of the known mutations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction and clinical symptoms
Ataxia with isolated vitamin E deficiency (AVED; MIM# 277460) is a rare autosomal recessive neurodegenerative disease, due to the defect of α-TTP, an intracellular cytosolic protein that bounds specifically to α-tocopherol [25].
The clinical phenotype resembles Friedreich’s ataxia, although Friedreich’s ataxia is more often accompanied by cardiomyopathy and impaired glucose metabolism [28]. Several features are shared with Friedreich ataxia, including cerebellar ataxia, loss of deep tendon reflexes, vibratory-sense disturbances, dysarthria, muscle weakness, and Babinski sign [16]. However, cardiomyopathy is significantly rarer in AVED than in Friedreich ataxia, whereas head titubation and dystonia appeared to be specific to AVED [10]. Generally, there is no scoliosis or foot deformity. Magnetic resonance imaging (MRI) of brain and nerve conduction are normal in most of cases (Fogel et al. 2007). The concomitant presence of specific neurological symptoms and very low levels of plasma vitamin E, in the absence of other clinical conditions commonly associated with fat malabsorption, can guide the differential diagnosis [2]. The disease can be diagnosed by clinical features associated with low levels of vitamin E of serum. Genetic diagnosis is possible but not necessary [8].
The phenotype of AVED also resembles abetalipoproteinemia since clinical signs in both diseases are caused by vitamin E deficiency. However, unlike AVED, vitamin E deficiency in abetalipoproteinemia is due to a gastrointestinal lipid uptake syndrome that leads to severe diarrhea. Patients have a very low serum vitamin E level (<3 mg/L; reference values 3–15 mg/L), with a normal intestinal fat absorption mechanism and no signs of abetalipoproteinemia. Since 1981, familial isolated vitamin E deficiency has been described [9], and despite the small number of cases initially reported, phenotypic variability appeared very great, ranging from severe Friedreich-like ataxia presentation (AVED) to mild neurological impairment and very late disease onset [36].
The treatment is supplementation with vitamin E up to 800 mg/day [29]. The administration of vitamin E supplements has resulted in cessation of the progression of the neurologic symptoms and signs in most patients and in a melioration of established neurologic abnormalities in some of them [18]. In other cases, there has been no improvement. The extent of recovery clearly is related to when the therapy is begun: the more advanced the deficit, the more limited the response to therapy [14]. It suggests that a prompt genetic characterization of AVED may prompt an early effective treatment of the disease. Hence, early diagnosis of vitamin E deficiency may provide considerable improvement in the quality of AVED patient’s life [41].
Molecular genetics
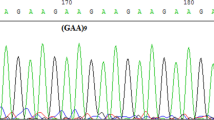
AVED is caused by mutations in the α-tocopherol transport protein (α-TTP) gene, which is located at chromosome 8q13 [33]. The gene consists of five exons.
α-TTP is able to selectively bind α-tocopherol (the most active vitamin E isomer) to the very-low-density lipoproteins (VLDLs) in the liver, which are released in the blood circulation. α-TTP is a cytosolic liver protein that is presumed to function in the intracellular transport of α-tocopherol [52]. The pathogenic basis of such ataxias at this time appears to involve two broad types of processes: free-radical injury and defects of DNA single- or double-strand break repair [24].
Vitamin E is a fat-soluble antioxidant that prevents lipid oxidation in the membranes. There are various forms of vitamin E, such as α-, β-, γ- and δ-tocopherol. α-tocopherol is regarded as the most biologically effective. Vitamin E is absorbed in the small intestine and transported in chylomicrons to the liver. In the liver α-tocopherol is incorporated into nascent VLDLs, which then enter the circulation.
Patients with AVED have a mutation of α-TTP gene and therefore cannot include α-tocopherol in the VLDL [17]. The lipid concentrations in their peripheral blood are normal, but vitamin E levels are very low. Because of this low level, the scavenging function fails and neurodegeneration appears most prominently in cerebellum and peripheral nerves. The connection between these pathological findings and vitamin E is not known in detail, but oxidative stress is likely to play a major role [22].
TTPA gene mutations analysis
Table 1 shows the different mutations described until now.
Using rat α-TTP to screen a liver cDNA library, followed by PCR, Arita et al. [4] cloned full-length human α-TTP. The deduced 278-amino acid protein has a calculated molecular mass of 31.7 kD and shares 94% identity with rat α-TTP [40]. Northern blot analysis of several human tissues detected a 4.5-kb α-TTP transcript in liver only TTPA gene in the chromosome 8q13.1–q13.3 region [6].
Today mutations on each exon have been described. The most frequent mutations of the TTPA gene is the 744delA in exon 5 and the 513insTT mutation in exon 3. In North-African populations, the most frequent mutation responsible for the disease is the 744delA mutation, while in AVED families of North European origin the 513insTT mutation has been often identified [26]. In Italian patients, these two mutations account for approximately 80% of the TTPA mutated alleles. Biochemical characterization of TTPA missense mutations has been reported for six missense mutations. These studies indicated that TTPA mutations (R59W, E141K, and R221W) associated with a severe early-onset AVED exhibit a clear impairment in both binding and transfer activity of TTPA, while the variants associated with the milder late-onset form of the disease (H101Q, A120T, R192H) show biochemical properties similar to the wild-type protein. For other mutations, the possible implication for AVED has been hypothesized on the basis of the crystal structure of the human TTPA protein [30]. The severity of the disease clearly can be modulated by different, nongenetic factors including the amount of vitamin E in the daily diet and the time of initiation and dosage of vitamin E supplementation, once the biochemical diagnosis has been made [5]. However, the phenotype associated with the semiconservative missense mutations (R192H, A120T, and H101Q) appears to be milder than that seen in the majority of cases [12]. The partial loss of function associated with mutations R192H and H101Q is corroborated by the results of previous studies, which used deuterated forms of α-tocopherol stereoisomers (RRR and SRR) [46]. In the study of the function of the hepatic α-TTP in normal humans, a marked preference for the RRR stereoisomer over the SSR form of α-tocopherol was found. The ability to discriminate between the isomers also was demonstrated in perfused monkey livers in vitro. Patients with R192H or H101Q mutations were still able to preferentially incorporate the natural RRR stereoisomer into VLDL, to a lesser extent than normal subjects, and were labeled “discriminators”. These patients contrasted with other patients who had a complete loss of the capacity to preferentially incorporate the natural α-tocopherol stereoisomer into VLDL (labeled “nondiscriminators”). In these patients, the mutations have been characterized, and they are homozygous for severe truncating mutations (530AGrGTAAGT, 744delA, 486delT, and R134X). Interestingly, they all are associated with a severe, early-onset form of the disease [31]. All other truncating mutations and the nonconservative missense mutations (R59W, E141K, and R221W) also seemed to be associated with the severe form of the disease, suggesting that they also result in complete loss of function, although the patients were not studied for their ability to discriminate between RRR and SRR isomers of α-tocopherol [15, 23]
References
Angelini L, Erba A, Mariotti C, Gellera C, Ciano C, Nardocci N (2002) Myoclonic dystonia as unique presentation of isolated vitamin E deficiency in a young patient. Mov Disord 17(3):612–614
Anheim M, Fleury M, Monga B, Laugel V, Chaigne D, Rodier G, Ginglinger E, Boulay C, Courtois S, Drouot N, Fritsch M, Delaunoy JP, Stoppa-Lyonnet D, Tranchant C, Koenig M (2010) Epidemiological, clinical, paraclinical and molecular study of a cohort of 102 patients affected with autosomal recessive progressive cerebellar ataxia from Alsace, Eastern France: implications for clinical management. Neurogenetics 11(1):1–12 (Epub 2009 May 14)
Aparicio JM, Belanger Quintana A, Suarez L, Mayo D, Benitez J, Diaz M, Escobar H (2001) Ataxia with isolated vitamin E deficiency: case report and review of the literature. J Pediatr Gastroenterol Nutr 33:206–210
Arita M, Sato Y, Miyata A, Tanabe T, Takahashi E, Kayden HJ, Arai H, Inoue K (1995) Human alpha-tocopherol transfer protein: cDNA cloning, expression and chromosomal localization. Biochem J 306(Pt. 2):437–443
Bellayou H, Dehbi H, Bourezgui M, Slassi I, Nadifi S (2009) Ataxia with vitamin E deficiency (AVED): an example of the contribution of research in molecular genetic to counselling in Morocco. Pathol Biol (Paris) 57(5):425–426 (Epub 2008 Nov 26)
Ben Hamida C, Doerflinger N, Belal S, Linder C, Reutenauer L, Dib C, Gyapay G, Vignal A, Le Paslier D, Cohen D et al (1993) Localization of Friedreich ataxia phenotype with selective vitamin E deficiency to chromosome 8q by homozygosity mapping. Nat Genet 5:195–200
Benomar A, Yahyaoui M, Meggouh F, Bouhouche A, Boutchich M, Bouslam N, Zaim A, Schmitt M, Belaidi H, Ouazzani R, Chkili T, Koenig M (2002) Clinical comparison between AVED patients with 744 del A mutation and Friedreich ataxia with GAA expansion in 15 Moroccan families. J Neurol Sci 198:25–29
Bouhlal Y, Zouari M, Kefi M, Ben Hamida C, Hentati F, Amouri R (2008) Autosomal recessive ataxia caused by three distinct gene defects in a single consanguineous family. J Neurogenet 22(2):139–148
Burck U, Goebel HH, Kuhlendahl HD, Meier C, Goebel KM (1981) Neuromyopathy and vitamin E deficiency in man. Neuropediatrics 12:267–278
Cavalier L, Ouahchi K, Kayden HJ, Di Donato S, Reutenauer L, Mandel JL, Koenig M (1998) Ataxia with isolated vitamin E deficiency: heterogeneity of mutations and phenotypic variability in a large number of families. Am J Hum Genet 62:301–310
Cellini E, Piacentini S, Nacmias B, Forleo P, Tedde A, Bagnoli S, Ciantelli M, Sorbi S (2002) A family with spinocerebellar ataxia type 8 expansion and vitamin E deficiency ataxia. Arch Neurol 59:1952–1953
Di Donato S, Gallera C, Mariotti C (2001) The complex clinical and genetic classification of inherited ataxias II. Autosomal recessiva atraxias. Neurol Sci 22(3):219–228 (review)
Doria-Lamba L, De Grandis E, Cristiani E, Fiocchi I, Montaldi L, Grosso P, Gellera C (2006) Efficacious vitamin E treatment in a child with ataxia with isolated vitamin E deficiency. Eur J Pediatr 165(7):494–495 (Epub 2006 Feb 21)
Eggermont E (2006) Recent advances in vitamin E metabolism and deficiency. Eur J Pediatr 165(7):429–434 (Epub 2006 Feb 21, review)
Fernández-Burriel M, Martínez-Rubio D, Lupo V, Pérez-Colosía V, Piñán-López E, Palau F, Espinós C (2008) A novel delins mutation in the alpha-TTP gene in a family segregating ataxia with isolated vitamin E deficiency. Pediatr Res 64(3):262–264
Fogel BL, Perlman S (2007) Clinical features and molecular genetics of autosomal recessive cerebellar ataxias. Lancet Neurol 6(3):245–257 (review)
Gabsi S, Gouider-Khouja N, Belal S, Fki M, Kefi M, Turki I, Ben Hamida M, Kayden H, Mebazaa R, Hentati F (2001) Effect of vitamin E supplementation in patients with ataxia with vitamin E deficiency. Eur J Neurol 8:477–481
Gohil K, Azzi A (2008) Reply to drug insight: antioxidant therapy in inherited ataxias. Nat Clin Pract Neurol 4(7):E1; author reply E2
Gotoda T, Arita M, Arai H, Inoue K, Yokota T, Fukuo Y, Yazaki Y, Yamada N (1995) Adult-onset spinocerebellar dysfunction caused by a mutation in the gene for the alpha-tocopherol-transfer protein. N Engl J Med 333:1313–1318
Hentati A, Deng HX, Hung WY, Nayer M, Ahmed MS, He X, Tim R, Stumpf DA, Siddique T (1996) Human alpha-tocopherol transfer protein: gene structure and mutations in familial vitamin E deficiency. Ann Neurol 39:295–300
Hoshino M, Masuda N, Ito Y, Murata M, Goto J, Sakurai M, Kanazawa I (1999) Ataxia with isolated vitamin E protei deficiency: a Japanese family carrying a novel mutation in the alpha-tocopherol transfer n gene. Ann Neurol 45(6):809–812
Kara B, Uzümcü A, Uyguner O, Rosti RO, Koçbaş A, Ozmen M, Kayserili H (2008) Ataxia with vitamin E deficiency associated with deafness. Turk J Pediatr 50(5):471–475
Koht J, Bjørnarå KA, Jørum E, Tallaksen CM (2009) Ataxia with vitamin E deficiency in southeast Norway, case report. Acta Neurol Scand Suppl (189):42–45
Koenig M, Mandel JL (1997) Deciphering the cause of Friedreich ataxia. Curr Opin Neurobiol 7(5):689–694
Manor D, Morley S (2007) The alpha-tocopherol transfer protein. Vitam Horm 76:45–65
Mariotti C, Gellera C, Rimoldi M, Mineri R, Uziel G, Zorzi G, Pareyson D, Piccolo G, Gambi D, Piacentini S, Squitieri F, Capra R, Castellotti B, Di Donato S (2004) Ataxia with isolated vitamin E deficiency: neurological phenotype, clinical follow-up and novel mutations in TTPA gene in Italian families. Neurol Sci. 25:130–137
Martinello F, Fardin P, Ottina M, Ricchieri GL, Koening M, Cavalier L, Trevisan CP (1998) Supplemental therapy in isolated vitamin E deficiency improves the peripheral neuropathy and prevents the progression of ataxia. J Neurol Sci 156:177–179
Marzouki N, Benomar A, Yahyaoui M, Birouk N, Elouazzani M, Chkili T, Benlemlih M (2005) Vitamin E deficiency ataxia with (744 del A) mutation on alpha-TTP gene: genetic and clinical peculiarities in Moroccan patients. Eur J Med Genet. 48:21–28
Meydani SN, Meydani M, Blumberg JB et al (1998) Assessment of the safety of supplementation with different amounts of vitamin E in healthy older adults. Am J Clin Nutr 68:311–318
Min KC, Kovall RA, Hendrickson WA (2003) Crystal structure of human alpha-tocopherol transfer protein bound to its ligand: implications for ataxia with vitamin E deficiency. Proc Natl Acad Sci USA 100:14713–14718
Min CK (2007) Structure and function of alpha-tocopherol transfer protein: implications for vitamin E metabolism and AVED. Vitam Horm 76:23–43 (review)
Morley S, Cross V, Cecchini M, Nava P, Atkinson J, Manor D (2006) Utility of a fluorescent vitamin E analogue as a probe for tocopherol transfer protein activity. Biochemistry 45(4):1075–1081
Ouahchi K, Arita M, Kayden H, Hentati F, Ben Hamida M, Sokol R, Arai H, Inoue K, Mandel JL, Koenig M (1995) Ataxia with isolated vitamin E deficiency is caused by mutations in the alpha-tocopherol transfer protein. Nat Genet 9:141–145
Palau F, Espinós C (2006) Autosomal recessive cerebellar ataxias. Orphanet J Rare Dis 1:47
Pang J, Kiyosawa M, Seko Y, Yokota T, Harino S, Suzuki J (2001) Clinicopathological report of retinitis pigmentosa with vitamin E deficiency caused by mutation of the alpha-tocopherol transfer protein gene. Jpn J Ophthalmol 45(6):672–676
Ponten SC, Kwee ML, Wolters E Ch, Zijlmans JC (2007) First case of ataxia with isolated vitamin E deficiency in the Netherland. Parkinsonism Relat Disord 13(5):315–316 (Epub 2006 Oct 16)
Qian J, Atkinson J, Manor D (2006) Biochemical consequences of heritable mutations in the alpha-tocopherol transfer protein. Biochemistry 45(27):8236–8242
Ricciarelli R, Argellati F, Pronzato MA, Domenicotti C (2007) Vitamin E and neurodegenerative diseases. Mol Aspects Med 28(5–6):591–606 (Epub 2007 Jan 11, review)
Roubertie A, Biolsi B, Rivier F, Humbertclaude V, Cheminal R, Echenne B (2003) Ataxia with vitamin E deficiency and severe dystonia: report of a case. Brain Dev 25(6):442–445
Sato Y, Arai H, Miyata A, Tokita S, Yamamoto K, Tanabe T, Inoue K (1993) Primary structure of alpha-tocopherol transfer protein from rat liver. Homology with cellular retinaldehyde-binding protein. J Biol Chem. 268:17705–17710
Schuelke M, Mayatepek E, Inter M et al (1999) Treatment of ataxia in isolated vitamin E deficiency caused by α-tocopherol transfer protein deficiency. J Pediatr 134:240–244
Schuelke M, Finckh B, Sistermans EA, Ausems MG, Hübner C, von Moers A (2000) Ataxia with vitamin E deficiency: biochemical effects of malcompliance with vitamin E therapy. Neurology 55(10):1584–1586
Shimohata T, Date H, Ishiguro H, Suzuki T, Takano H, Tanaka H, Tsuji S, Hirota K (1998) Ataxia with isolated vitamin E deficiency and retinitis pigmentosa. Ann Neurol 43:273
Sokol RJ, Kayden HJ, Bettis DB, Traber MG, Neville H, Ringel S et al (1988) Isolated vitamin E deficiency in the absence of fat malabsorption familial and sporadic cases: characterization and investigation of causes. J Lab Clin Med 111:548–559
Tamaru Y, Hirano M, Kusaka H, Ito H, Imai T, Ueno S (1997) alpha-Tocopherol transfer protein gene: exon skipping of all transcripts causes ataxia. Neurology 49(2):584–588
Traber MG (1997) Regulation of human plasma vitamin E. Adv Pharmacol 38:49–63 (review)
Usuki F, Maruyama K (2000) Ataxia caused by mutations in the alpha-tocopherol transfer protein gene. J Neurol Neurosurg Psychiatry 69:254–256
Yokota T, Wada Y, Furukawa T, Tsukagoshi H, Uchihara T, Watabiki S (1987) Adult-onset spinocerebellar syndrome with idiopathic vitamin E deficiency. Ann Neurol 22:84–87
Yokota T, Shiojiri T, Gotoda T, Arai H (1996) Retinitis pigmentosa and ataxia caused by a mutation in the gene for the α-tocopherol transfer protein. N Engl J Med 335:1770–1771
Yokota T, Shiojiri T, Gotoda T (1997) Friedreich-like ataxia with retinitis pigmentosa caused by the His101Gln mutation of α-tocopherol transfer protein gene. Ann Neurol 41:826–832
Yokota T, Uchihara T, Kumagai J, Shiojiri T, Pang JJ, Arita M (2000) Postmortem study of ataxia with retinitis pigmentosa by mutation of the a-tocopherol transfer protein gene. J Neurol Neurosurg Psychiatry 68(4):521–525
Zingg JM (2007) Vitamin E: an overview of major research directions. Mol Aspects Med 28(5–6):400–422 (Epub 2007 Jun 2)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Di Donato, I., Bianchi, S. & Federico, A. Ataxia with vitamin E deficiency: update of molecular diagnosis. Neurol Sci 31, 511–515 (2010). https://doi.org/10.1007/s10072-010-0261-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-010-0261-1