Abstract
While Friedreich's ataxia (FRDA) and ataxia telangiectasia (AT) are known to be the two most frequent forms of autosomal recessive cerebellar ataxia (ARCA), knowledge on the other forms of ARCA has been obtained only recently, and they appear to be rarer. Little is known about the epidemiological features and the relative frequency of the ARCAs and only few data are available about the comparative features of ARCAs. We prospectively studied 102 suspected ARCA cases from Eastern France (including 95 from the Alsace region) between 2002 and 2008. The diagnostic procedure was based on a sequential strategic scheme. We examined the clinical, paraclinical and molecular features of the large cohort of patients and compared features and epidemiology according to molecular diagnosis. A molecular diagnosis could be established for 57 patients; 36 were affected with FRDA, seven with ataxia plus oculomotor apraxia type 2 (AOA2), four with AT, three with ataxia plus oculomotor apraxia type 1 (AOA1), three with Marinesco–Sjögren syndrome, two with autosomal recessive spastic ataxia of Charlevoix–Saguenay (ARSACS), one with ataxia with vitamin E deficiency (AVED) and one with autosomal recessive cerebellar ataxia type 2 (ARCA2). The group of patients with no identified mutation had a significantly lower spinocerebellar degeneration functional score corrected for disease duration (SDFS/DD ratio; p = 0.002) and comprised a significantly higher proportion of cases with onset after 20 years (p < 0.01). Extensor plantar reflexes were rarer and cerebellar atrophy was more frequent in the group of patients with a known non-Friedreich ARCA compared to all other patients (p < 0.0001 and p = 0.0003, respectively). Lower limb areflexia and electroneuromyographic evidences of peripheral neuropathy were more frequent in the Friedreich ataxia group than in the group with a known non-Friedreich ataxia and were more frequent in the later group than in the group with no identified mutation (p = 0.0001 and p = 0.01, respectively). The overall prevalence of ARCA in Alsace is 1/19,000. We can infer the prevalence of FRDA in Alsace to be 1/50,000 and infer that AT is approximately eight times less frequent than FRDA. MSS, AOA2 and ARSACS appear only slightly less frequent than AT. Despite the broad variability of severity, Friedreich ataxia patients are clinically distinct from the other forms of ARCA. Patients with no identified mutation have more often a pure cerebellar degenerative disease or a spastic ataxia phenotype. It appears that ARCA cases can be divided into two major groups of different prognosis, an early-onset group with a highly probable genetic cause and an adult-onset group with better prognosis for which a genetic cause is more difficult to prove but not excluded. ARCAs are rare, early-disabling and genetically heterogeneous diseases dominated by FRDA. Several of the recently identified ARCAs, such as AVED, ARSACS, AOA1, AOA2 and MSS, have a prevalence close to AT and should be searched for extensively irrespective of ethnic origins. The strategic scheme is a useful tool for the diagnosis of ARCAs in clinical practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Autosomal recessive cerebellar ataxias (ARCAs) are a heterogeneous group of inherited neurodegenerative disorders that affect the cerebellum, the spinocerebellar tract and/or the sensory tracts of the spinal cord. They are characterised by prominent progressive cerebellar ataxia in association with other neurological or extra-neurological signs. In the past 15 years, there has been extensive progress in the knowledge of ARCA [1, 2], with more than ten genes identified. Friedreich's ataxia (FRDA) and ataxia telangiectasia (AT) were reported to be the two most frequent forms of ARCA [3–6]. The other forms of ARCA are rarer [1]. Several pathological pathways appear to be shared by different ARCAs, such as defect in DNA break repair [AT, ataxia with oculomotor apraxia type 1 (AOA1), ataxia with oculomotor apraxia type 2 (AOA2), ataxia telangiectasia-like disorder (ATLD) and spinocerebellar ataxia with axonal neuropathy (SCAN1)] [5, 7–12] or defective mitochondrial homeostasis [(FRDA, sensory ataxic neuropathy with dysarthria and ophthalmoplegia (SANDO), infantile onset spinocerebellar ataxia (IOSCA), ARCA type 2 (ARCA2)] [13–16]. Drugs have been reported to have potential efficacy in treating some ARCA such as alpha-tocopherol in ataxia with vitamin E deficiency (AVED) [16–22] or idebenone in FRDA [23–25]. Despite the recent progress, little is known about the epidemiological features and the relative frequency of the ARCA [6, 26–34]. Moreover, only few data are available about the comparative features of ARCA. We prospectively studied all cases of suspected recessively inherited ARCA in Alsace, Eastern France between 2002 and 2008 in order to examine the clinical, paraclinical and molecular features of a large cohort of patients and to compare features and epidemiology according to molecular diagnosis.
Materials and methods
From 2002 to 2008, we prospectively included in our study all patients, irrespective of their ethnic origin, affected with suspected ARCA and who were referred to the Departments of Neurology or Pediatrics of the two major Alsace regional hospitals, Strasbourg and Mulhouse. A detailed phenotype was obtained following complete clinical examination and laboratory, imaging, electrophysiological and molecular investigations.
Inclusion criteria for suspected ARCA were: predominant cerebellar ataxia and onset before the age of 60 years (because FRDA may occur until this age). Particularly suggestive of autosomal recessive inheritance were the presence of similar cases in the sibship and/or consanguineous union of the parents. All patients with suspected ARCA who were referred to one of the local centres were included in the cohort. Exclusion criteria were: congenital ataxia or ataxia associated with prominent cerebral involvement or leucoencephalopathy, other identified aetiologies (multiple sclerosis, multiple system atrophy, virus, drug intoxication, paraneoplastic syndrome…) and knowledge of dominant inheritance in the family.
According to published criteria and our clinical experience [1–6, 8, 10, 11, 13, 16, 37, 38, 47, 48], we used a diagnostic procedure based on a strategic scheme that sequentially integrates clinical, laboratory (including the FRDA GAA expansion test), imaging, electrophysiological and finally sequencing data (Fig. 3).The following clinical items were noted: date of birth, origin, family history, age at onset of the disease, disability stage [spinocerebellar degeneration functional score (SDFS)] from 0 (no cerebellar sign) to 7 (bedridden), pyramidal signs, motor deficiency, deep tendon reflexes, vibratory sense, visual acuity, movement disorders, oculomotor features including oculomotor apraxia (OMA) [35], foot deformities or scoliosis and mental retardation. Laboratory investigations included (Table 1): vitamin E, alpha-foetoprotein, glycaemia, phytanic acid, cholesterol, triglyceride, albumin, lipoproteins, protein electrophoresis, lactic acid, creatin kinase, acanthocytes, amino acidemia and very long-chain fatty acids of the serum, urinary oligosaccharides, leukocytic enzymes, lysosomal enzymes, karyotype, cerebrospinal fluid analysis, skin biopsy and muscle and/or nerve biopsy. Imaging investigations consisted of cerebral tomodensitometry and/or cerebral magnetic resonance imaging and echocardiography. Electrophysiological investigations included electroneuromyography, electroencephalography, oculography, sensory evoked potentials and visual evoked potentials. Genetic analysis included (Table 1): FRDA [4], AVED [16, 18], AOA1 [10, 36], AOA2 [8], AT [5], Marinesco–Sjögren syndrome (MSS) [37], autosomal recessive spastic ataxia of Charlevoix–Saguenay (ARSACS) [38], ATLD [11], recessive ataxia associated with coenzyme Q10 deficiency (ARCA2) [13], dominant spinocerebellar ataxias (SCAs 1, 2, 3, 6, 7 and 17) [39, 40], dentato-rubro-pallido-luysian atrophy [41, 42], Huntington disease [43] and choreoacanthocytosis (ChAc) [44]. Except for the expansion disease genes, all other genes (AOA1, AOA2, AVED, AT, MRE11, ARSACS, ARCA2, MSS and ChAc) were tested by sequencing of all coding exons
Statistical analysis
Patients’ data were collected in a computerised database and analysed using the statistical software package Statistical Analysis System (SAS) for Windows, release 9.1.3 (SAS Institute, Cary, NC, USA). Categorical variables were analysed with the chi-square test and Yates' correction or Fisher's exact test when necessary. Non-parametric statistical methods were used for analysis, as most analysed quantitative variables could not meet the assumption of normality. Such variables are presented as the median (Q1:25th–Q3:75th percentiles), whilst categorical variables are presented as frequencies (percentage of patients).
We used Wilcoxon rank-sum test (two groups) and Kruskal–Wallis test (more than two groups) for all comparisons of quantitative variables across groups. Spearman correlation coefficients were computed in order to assess the strength of linear relationship between two quantitative variables. Three groups were compared: FRDA patients (group 1), non-FRDA patients with a genetically established diagnosis (group 2) and patients without a diagnosis (group 3). The “spinocerebellar degeneration functional score/duration of the disease” (SDFS/DD) ratio was used in this study to evaluate the severity of the disease progression, but is not yet validated. All of the statistical tests were two-sided, and statistical significance was inferred when p < =0.05.
Results
One hundred and two patients were included in our study (Table 2). The mean age at onset of the disease was 16.1 years ±13.4 SD, mean age at last examination was 32.8 years ±15.6 SD, mean disease follow-up was 16.7 ±11.9 SD, and mean SDFS/DD ratio was 0.45 ± 0.42 SD. Forty-nine per cent of patients were women. The disability stage at last examination was 6/7 (i.e. wheelchair-bound) in 34% of patients and 3/7 (i.e. able to walk without help, but not able to run) in 29%. We compared three groups of patients: FRDA patients (n = 36, group 1), patients with another diagnosis (including four AT, seven AOA2, three AOA1, three MSS, two ARSACS, one AVED and one ARCA2, n = 21, group 2) and patients without diagnosis (n = 45, group 3). The 45 patients of group 3 were not tested for all disease genes, but only for the strongly suspected or compatible genes (Table 1 and Fig. 3): All patients from group 3 were tested for FRDA; 25 were tested for AOA1, 12 for AOA2, three for AT, two for ARSACS, one for MSS, 11 for ARCA2 and two for MRE11.
The mean, median, standard deviation, minimum, maximum, Q1 and Q3 of the age at onset, disease duration and SDFS/DD score in each group and for each type of diagnosis are presented in Fig. 1 and Table 3. For the FRDA patients (36 patients including 30 treated with idebenone), the size of the shorter GAA repeat expansion extended from 0.4 up to 3.6 kb (mean, 1.95), whereas the size of the larger GAA repeat expansion extended from 0.5 up to 4.6 kb (mean, 2.8). The size of the shorter GAA repeat expansion was negatively correlated with the age at onset (r = −0.7, p < 0.0001) as well as associated with scoliosis (p = 0.02), pes cavus (p = 0.03), loss of deep tendon reflexes (p < 0.05) and low vibration sense (p = 0.01), but not with electroneurographic evidences of polyneuropathy. No significant association was found between the size of the shorter GAA repeat expansion and the occurrence of cardiomyopathy, diabetes, extensor plantar reflexes, movement disorders or the SDFS/DD ratio at last examination. The proportion of non-FRDA ARCA for which a genetic diagnosis could be established was higher for cases with a disease onset before 20 years of age (42%) than for cases with later onset (0%; χ 2 = 9.86, p = 0.001). As a result, age at onset was lower in group 2 (median = 8.0 years, Q1 = 2, Q3 = 15) than in groups 1 (median = 13.5 years, Q1 = 10, Q3 = 21) and 3 (median = 14 years, Q1 = 7, Q3 = 25, p = 0.01; Fig. 1 and Table 4). Inversely, the SDFS/DD ratio was significantly lower in group 3 (median = 0.20, Q1 = 0.13, Q3 = 0.43) than in groups 1 (median = 0.52, Q1 = 0.32, Q3 = 0.75) and 2 (median = 0.38, Q1 = 0.27, Q3 = 0.60, p = 0.002), suggesting that prognosis of ARCA is better when a genetic cause has not been identified despite appropriate investigations (Table 4). Extensor plantar reflexes were rarer in group 2 (27.8%) than in groups 1 (93.8%) and 3 (78.0%; χ 2 = 26.6, p < 0.0001). Lower-limb areflexia and electroneuromyographic evidences of peripheral neuropathy were more frequent in group 1 (83.9% and 86.4%, respectively) than in group 2 (63.2% and 69.2%, respectively) and in group 2 than in group 3 (34.2% and 48.6%, respectively; χ 2 = 18.2, p = 0.0001 and χ 2 = 8.57, p = 0.01, respectively). Similar results were found regarding axonal neuropathy (χ 2 = 9.84, p < 0.01), but no difference was found between the three groups with respect to demyelinating neuropathy. Pure sensory neuropathy was more frequent in group 1 (55%) than in groups 2 (7.7%) and 3 (14.3%; χ 2 = 13.82, p = 0.001). Pure motor neuropathy was identified in only one patient of group 3 and never in the other groups (Table 4). Interestingly, movement disorders were not uncommon and were noted in 32.5% of the 102 patients, including tremor (16.7%), myoclonus (7.8%), dystonia (12.8%), chorea (5.9%) and tics (2.9%), without any difference between the three groups of patients. Magnetic resonance imaging (MRI) cerebellar atrophy was more frequent in group 2 (86.7%) than in group 3 (68.4%) and in group 3 than in group 1 (15.4%; χ 2 = 16.55, p = 0.0003). No difference was found regarding diffuse cerebrospinal atrophy and pons atrophy. Brain MRI in FRDA was consistent with spinal cord atrophy. Repeated MRI during the course of FRDA allowed detecting the onset of a progressive mild cerebellar atrophy (Fig. 2). A moderate cerebellar atrophy similar to that encountered in FRDA was found in our AVED. MRI of ARSACS showed a predominantly vermian cerebellar atrophy as well as linear hypointensities on T2 and T2 fluid-attenuated inversion recovery-weighted images in the pons (Fig. 2), as described by Martin et al. [45]. Cerebellar atrophy was marked in AT, AOA1 and AOA2 patients (Fig. 2).
Brain magnetic resonance imaging (MRI) of patients at different times of disease duration. a–h Sagittal T1-weighted MRI, i axial T2-weighted brain MRI. a Patient 16 affected with FRDA since 1 year. No cerebellar atrophy. b Patient 16 affected with FRDA since 10 years. Mild cerebellar atrophy and moderate cervical spinal atrophy. c Patient 16 affected with FRDA since 20 years. Moderate cerebellar atrophy and marked cervical spinal atrophy. d Patient 85 affected with AT since 6 months. Severe diffuse cerebellar atrophy. e Patient 8 affected with AOA1 since 6 years. Severe diffuse cerebellar atrophy. f Patient 20 affected with AOA2 since 15 years. Marked diffuse cerebellar atrophy. g Patient 25 affected with AVED since 19 years. Moderate cerebellar atrophy. h Patient 45 affected with ARSACS since 27 years. Marked cerebellar atrophy mainly located on anterior upper part of the cerebellum. i Patient 45 affected with ARSACS since 27 years. Linear bilateral hypointensities in the pons are indicated by arrows
Obviously, cardiomyopathy and diabetes were more frequent in group 1 (61% and 26%, respectively) than in the other groups (χ 2 = 25.39, p < 0.0001 and χ 2 = 6.72, p = 0.03, respectively). Elevated AFP and elevated CK were more frequent in group 2 than in groups 1 and 3 (χ 2 = 17.00, p = 0.0003 and χ 2 = 7.45, p = 0.02, respectively; Table 4). The higher incidence of elevated serum AFP levels in group 2 was accounted by the AT and AOA2 patients, even though one FRDA patient and three patients of group 3 also had elevated AFP levels. AT was clinically excluded and AOA2 was molecularly excluded in these three patients. The only patients who had low serum albumin or vitamin E levels were affected with AOA1 and AVED, respectively. The patients affected with juvenile cataract (onset between 4 and 6 years of age) had MSS, whilst one patient from group 3 had congenital cataract and another had adolescent onset cataract. Fundus examination revealed prominent retinal myelinated fibres in the two patients affected with ARSACS.
In group 2, we report four cases of AT including the following mutations: patient 83, c.3712_3716del5 (exon 27) leading to p.Leu1238Stop and c.7327C>T (exon 52) leading to p.Arg2443Stop; patient 85, c.3802delG (exon 28) responsible for p.Val1268Stop and c.8624A>G (exon 61) leading to p.Asn2875Ser; patient 86, c.782delC (exon 9) responsible for p.Thr261Ilefs15Stop and c.6203T>C (exon 45) leading to p.Leu2068Ser. The AVED case in this study bears a new homozygous mutation, 552+3A>T, that affects the donor splice site of exon 3. The three patients (65, 72 and 73) affected with MSS were reported by Anttonen et al. [37] (families M16 and M11 in this reference). The three patients with AOA1, the seven patients with AOA2 and the two patients with ARSACS were reported in [46–48], respectively. We describe in group 2 a patient affected with ARCA2 due to the following heterozygous compound mutations in ADCK3: c.993C>T (exon 8) and c.1645G>A (exon 14) leading to skipping of exon 14 (p.Lys314_Glu360del) and p.Gly549Ser, respectively [13]. The patient had progressive cerebellar ataxia which appeared at 2 years of age and is associated with dysarthria, bilateral sensorineural deafness, brisk reflexes in the lower limbs, mental retardation (intellectual quotient, 54) and pes cavus. Scale for Assessment and Rating Ataxia (SARA) score was 13/40, SDFS was 3/7 at 30 years of age, adiadoscore was moderately altered, Ashworth score was 1, ambulatory score was 0 and PATA test score was 11. Fundus, electroencephalogram, electromyogram, brain computer tomography and laboratory examinations, including serum lactate, were normal.
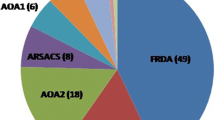
For epidemiological purposes, we considered only the 95 patients living in the main recruiting administrative region, Alsace (Table 2), since we had a bias in the recruitment of the rare AOA1 and AOA2 forms from the neighbouring Lorraine region (AOA1 and AOA2 patients from this region were referred to the Strasbourg Neurology Department at the time of gene identification of these two disorders in Strasbourg [47, 48]. The overall prevalence of ARCA in Alsace is 1/19,000 (95 patients out of 1,800,000 individuals) or 5.3/100,000. Distribution of each type of ARCA among the Alsatian patients is presented in Fig. 3. As expected, FRDA and AT are the most and second most frequent ARCAs, respectively. We can infer the prevalence of FRDA in Alsace to be 1/50,000 (36 cases out of 1,800,000 individuals) and infer that AT is approximately eight times less frequent than FRDA. MSS, AOA2 and ARSACS appeared to be only slightly less frequent than AT.
Algorithm for ARCA diagnostic procedure in clinical practice. The frequent signs are signs observed in several ARCAs and may orientate the diagnostic procedure, whereas the specific signs may discriminate a precise diagnosis. FRDA Friedreich ataxia, CTX cerebrotendinous xanthomatosis. Since detection of the FRDA GAA expansion is a simple molecular test that has broad implication for the diagnosis of ARCA, it was included in the early laboratory tests. Paraclinical tests include tests that, in practice, require longer delay for completion. SEP somesthesic evoked potentials, EMG electromyography, CSF cerebrospinal fluid. Asterisk indicates a biomarker that is always altered in the specified ARCA
Discussion
Few comparative epidemiological data are available for the different forms of ARCA, mostly due to the recent availability of the corresponding molecular tests. We report here a prospective multicentric study of a large cohort of ARCA from Alsace, Eastern France, which allowed inferring directly the prevalence of the most frequent forms of ARCA. We found that the overall prevalence of ARCA in Alsace is 1 in 19,000 or 5.3/100,000. The difference with the recent estimate of 2.2/100,000 for ARCA prevalence in the Oslo County [26] may reflect a real difference between the two regions or may be due in part to the fact that some of our presumed ARCA patients without a molecular diagnosis do not have an inherited form of ataxia. We found that the prevalence of FRDA is 1/50,000 in Alsace, a figure in good agreement with the frequency of carriers in the general population (1/90) [49, 50] that predicts an incidence of 1/32,400. The difference between prevalence and incidence is readily accounted by the presymptomatic individuals and the shorter life expectancy of the most severe FRDA cases. The prevalence in Alsace appears higher than in the Padua province, Italy where a prevalence of 6/1,000,000 (1/170,000) has been reported [28]. The higher prevalence of FRDA in the upper Rhine valley may explain why it was first recognised there by Nicholaus Friedreich in 1863. AT incidence is estimated between 1/40,000 and 1/100,000 in the USA [6], whilst it was very low in the Padua study, as was AVED incidence [28]. Our study is the first comparative epidemiological study of FRDA, AT, AVED, AOA1, AOA2, ARSACS, ARCA2 and MSS. It confirms that AT is the second most prevalent ARCA, though with a prevalence of 1/450,000 (or 2.2/1,000.000), a figure closer to the Padua prevalence. AOA2 has been suspected to be the second most frequent cause of ARCA in adults, after FRDA [31]. Despite a very broad confidence interval, our study suggests a prevalence of 1/900,000, a figure in agreement with the prevalence of AOA2 in the neighbouring Lorraine region [five patients (two families) out of 2,400,000 inhabitants].
A molecular diagnosis was established in 56% of our patients, representing eight distinct forms of ARCA. Our strategic scheme therefore appears to be effective for the clinical practice when ARCA is suspected. For practical reasons, including cost and hurdles to sequence large genes (such as ATM and SETX which contain 66 and 24 exons, respectively) or scarcity of some ARCAs such as ATLD and IOSCA, it is not effective to sequence all genes in all non-FRDA patients. We believe that our sequential scheme reasonably minimises the risk to miss rare atypical presentations. No differential diagnosis was identified in our series possibly due to the selection criteria that excluded patients with white matter changes.
A third of the patients of this study were wheelchair-bound after a median disease duration of 14 years and less than a third could still walk without assistance. However, for most of the patients, the age at which ambulation was lost was not available. The SDFS at last examination, even when corrected by disease duration, is probably not sufficient to discriminate for disease progression between the different ARCAs. Further studies using SARA [51, 52], Friedreich Ataxia Rating Scale [53], International Cooperative Ataxia Rating Scale [53] or Composite Cerebellar Functional Severity score [54] would be needed in the future. For clinical comparisons, we defined three patient groups for practical purposes. The FRDA group, which accounts for one third of the patients, is a well-defined group by itself. Group 3 consists of patients that share a negative exhaustive aetiologic investigation, and group 2 is the smallest and most heterogeneous group that comprises the patients affected by a rare form of ARCA. Despite these somewhat arbitrary criteria, it appears that the three groups are clinically distinct from each other. Group 2 consists of early-onset, severe ataxic patients, whilst group 3 mostly consists of adult-onset ataxia patients with a milder disease. Group 1 is intermediate between groups 2 and 3 due to the broad clinical variability seen in FRDA, which correlates with the smaller GAA expansion [our series included six cases of late-onset (>26 years) FRDA (LOFA)]. In group 2, AOA1 has a broad distribution of age at onset which correlates with previously reported heterogeneous phenotypes [48], whereas the distribution of age at onset for AOA2 is very narrow due to a homogeneous phenotype [47].
The three groups are also distinct when compared for clinical features. Group 2 shares features of cerebellar involvement (with cerebellar atrophy on MRI) frequently associated with OMA and peripheral neuropathy, and only occasionally with pyramidal signs, whilst group 3 also shares features of cerebellar involvement but frequently associated with pyramidal signs and less often with peripheral neuropathy (Table 4). Group 3 therefore seems to represent forms of pure cerebellar degenerative disease or of spastic ataxia phenotype. Despite a large variability in severity, group 1 stands by itself, in accordance with the classical clinical criteria for FRDA (primary spinal cord involvement, sensory neuropathy and extensor plantar reflexes). Cerebellar atrophy is not a common feature of FRDA [34, 55], but was suggested to be more frequent in LOFA [56]. However, no cerebellar atrophy was found in our four LOFA patients who underwent brain MRI. As expected, cardiomyopathy and diabetes were more frequent in group 1 with 61% and 26%, respectively, which is close to the 63% and 32% previously reported [3]. The occurrence of pes cavus and scoliosis was correlated with the size of the shorter GAA expansion, as were loss of deep tendon reflexes and low vibratory sense. However, electroneurographic evidences of polyneuropathy were not correlated with the size of the smaller expansion, probably because the majority of FRDA patients with infraclinical neuropathy already have electric signs upon recording.
After exclusion of the FRDA cases, which is now performed as a first diagnostic step in a clinical settings [2], it appears that ARCA cases can be divided into two major groups of different prognosis, an early-onset group with a highly probable genetic cause and an adult-onset group with a better prognosis and for which a genetic cause is more difficult to prove but not excluded. In our series, all non-FRDA patients with onset of the disease after 20 years of age remained undiagnosed. The recent successful attempts to identify an ARCA cause to adult-onset cases [57, 58, 59] are likely to change the diagnostic strategies in the future.
Eight types of ARCA are represented in our series, which underlines the genotypic heterogeneity of the ARCAs, including the recently described ARCA2 [13]. ARSACS, for which two cases were included in this study, is most frequently described in the region of Charlevoix–Saguenay, Quebec, but has also been reported elsewhere [47, 60–63]. Head tremor, reported in nearly 30% of AVED patients, lead in our case to investigate for vitamin E levels and to make the diagnosis of AVED for the patient reported in this study. Thus, movement disorders, affecting nearly a third of the patients in our series, may be helpful for diagnostic strategy. Elevated low-density lipoprotein (LDL) cholesterol was not helpful to discriminate for AOA1 due to the frequency of this laboratory finding, whilst hypoalbuminemia was a more accurate AOA1 marker, although it is known to occur late in the course of the disease.
In conclusion, ARCAs are rare, early-disabling and genetically heterogeneous diseases dominated by FRDA. Several of the recently identified ARCAs, such as AVED, ARSACS, AOA1, AOA2 and MSS, have a prevalence close to AT and should be searched extensively, irrespective of ethnic origins. Our strategic scheme, including biomarkers such as AFP, serum vitamin E and albumin, as well as MRI investigations appeared to be very useful for the diagnosis of these forms of ARCA.
References
Koenig M (2003) Rare forms of autosomal recessive neurodegenerative ataxia. Semin Pediatr Neurol 10(3):183–192
Fogel BL, Perlman S (2007) Clinical features and molecular genetics of autosomal recessive cerebellar ataxias. Lancet Neurol 6(3):245–257
Durr A, Cossee M, Agid Y, Campuzano V, Mignard C, Penet C et al (1996) Clinical and genetic abnormalities in patients with Friedreich's ataxia. N Engl J Med 335(16):1169–1175
Campuzano V, Montermini L, Molto MD, Pianese L, Cossee M, Cavalcanti F et al (1996) Friedreich's ataxia: autosomal recessive disease caused by an intronic GAA triplet repeat expansion. Science 271(5254):1423–1427. doi:10.1126/science.271.5254.1423
Savitsky K, Bar-Shira A, Gilad S, Rotman G, Ziv Y, Vanagaite L et al (1995) A single ataxia telangiectasia gene with a product similar to PI-3 kinase. Science 268(5218):1749–1753. doi:10.1126/science.7792600
Chun HH, Gatti RA (2004) Ataxia–telangiectasia, an evolving phenotype. DNA Repair (Amst) 3(8–9):1187–1196. doi:10.1016/j.dnarep.2004.04.010
Caldecott KW (2008 Aug) Single-strand break repair and genetic disease. Nat Rev 9(8):619–631
Moreira MC, Klur S, Watanabe M, Nemeth AH, Le Ber I, Moniz JC et al (2004) Senataxin, the ortholog of a yeast RNA helicase, is mutant in ataxia–ocular apraxia 2. Nat Genet 36(3):225–227. doi:10.1038/ng1303
Takashima H, Boerkoel CF, John J, Saifi GM, Salih MA, Armstrong D et al (2002) Mutation of TDP1, encoding a topoisomerase I-dependent DNA damage repair enzyme, in spinocerebellar ataxia with axonal neuropathy. Nat Genet 32(2):267–272. doi:10.1038/ng987
Moreira MC, Barbot C, Tachi N, Kozuka N, Uchida E, Gibson T et al (2001) The gene mutated in ataxia–ocular apraxia 1 encodes the new HIT/Zn-finger protein aprataxin. Nat Genet 29(2):189–193. doi:10.1038/ng1001-189
Stewart GS, Maser RS, Stankovic T, Bressan DA, Kaplan MI, Jaspers NG et al (1999) The DNA double-strand break repair gene hMRE11 is mutated in individuals with an ataxia–telangiectasia-like disorder. Cell 99(6):577–587. doi:10.1016/S0092-8674(00)81547-0
Suraweera A, Becherel OJ, Chen P, Rundle N, Woods R, Nakamura J et al (2007) Senataxin, defective in ataxia oculomotor apraxia type 2, is involved in the defense against oxidative DNA damage. J Cell Biol 177(6):969–979. doi:10.1083/jcb.200701042
Lagier-Tourenne C, Tazir M, Lopez LC, Quinzii CM, Assoum M, Drouot N et al (2008) ADCK3, an ancestral kinase, is mutated in a form of recessive ataxia associated with coenzyme Q10 deficiency. Am J Hum Genet 82(3):661–672. doi:10.1016/j.ajhg.2007.12.024
Mollet J, Delahodde A, Serre V, Chretien D, Schlemmer D, Lombes A et al (2008) CABC1 gene mutations cause ubiquinone deficiency with cerebellar ataxia and seizures. Am J Hum Genet 82(3):623–630. doi:10.1016/j.ajhg.2007.12.022
Puccio H, Koenig M (2002) Friedreich ataxia: a paradigm for mitochondrial diseases. Curr Opin Genet Dev 12(3):272–277. doi:10.1016/S0959-437X(02)00298-8
Ben Hamida C, Doerflinger N, Belal S, Linder C, Reutenauer L, Dib C et al (1993) Localization of Friedreich ataxia phenotype with selective vitamin E deficiency to chromosome 8q by homozygosity mapping. Nat Genet 5(2):195–200. doi:10.1038/ng1093-195
Gabsi S, Gouider-Khouja N, Belal S, Fki M, Kefi M, Turki I et al (2001) Effect of vitamin E supplementation in patients with ataxia with vitamin E deficiency. Eur J Neurol 8(5):477–481. doi:10.1046/j.1468-1331.2001.00273.x http://www.ncbi.nlm.nih.gov/sites/entrez?cmd=Retrieve&db=PubMed&list_uids=11554913&dopt=Abstract
Ouahchi K, Arita M, Kayden H, Hentati F, Ben Hamida M, Sokol R et al (1995) Ataxia with isolated vitamin E deficiency is caused by mutations in the alpha-tocopherol transfer protein. Nat Genet 9(2):141–145. doi:10.1038/ng0295-141 http://www.ncbi.nlm.nih.gov/sites/entrez?cmd=Retrieve&db=PubMed&list_uids=7719340&dopt=Abstract
Martinello F, Fardin P, Ottina M, Ricchieri GL, Koenig M, Cavalier L et al (1998) Supplemental therapy in isolated vitamin E deficiency improves the peripheral neuropathy and prevents the progression of ataxia. J Neurol Sci 156(2):177–179. doi:10.1016/S0022-510X(98)00038-0 http://www.ncbi.nlm.nih.gov/sites/entrez?cmd=Retrieve&db=PubMed&list_uids=9588854&dopt=Abstract
Kohlschutter A, Hubner C, Jansen W, Lindner SG (1988) A treatable familial neuromyopathy with vitamin E deficiency, normal absorption, and evidence of increased consumption of vitamin E. J Inherit Metab Dis 11(Suppl 2):149–152. doi:10.1007/BF01804221 http://www.ncbi.nlm.nih.gov/sites/entrez?cmd=Retrieve&db=PubMed&list_uids=3141695&dopt=Abstract
Kayden HJ (1993) The neurologic syndrome of vitamin E deficiency: a significant cause of ataxia. Neurology 43(11):2167–2169 http://www.ncbi.nlm.nih.gov/sites/entrez?cmd=Retrieve&db=PubMed&list_uids=8232922&dopt=Abstract
Cavalier L, Ouahchi K, Kayden HJ, Di Donato S, Reutenauer L, Mandel JL et al (1998) Ataxia with isolated vitamin E deficiency: heterogeneity of mutations and phenotypic variability in a large number of families. Am J Hum Genet 62(2):301–310. doi:10.1086/301699 http://www.ncbi.nlm.nih.gov/sites/entrez?cmd=Retrieve&db=PubMed&list_uids=9463307&dopt=Abstract
Rustin P, von Kleist-Retzow JC, Chantrel-Groussard K, Sidi D, Munnich A, Rotig A (1999) Effect of idebenone on cardiomyopathy in Friedreich's ataxia: a preliminary study. Lancet 354(9177):477–479. doi:10.1016/S0140-6736(99)01341-0 http://www.ncbi.nlm.nih.gov/sites/entrez?cmd=Retrieve&db=PubMed&list_uids=10465173&dopt=Abstract
Di Prospero NA, Baker A, Jeffries N, Fischbeck KH (2007) Neurological effects of high-dose idebenone in patients with Friedreich's ataxia: a randomised, placebo-controlled trial. Lancet Neurol 6(10):878–886. doi:10.1016/S1474-4422(07)70220-X http://www.ncbi.nlm.nih.gov/sites/entrez?cmd=Retrieve&db=PubMed&list_uids=17826341&dopt=Abstract
Hausse AO, Aggoun Y, Bonnet D, Sidi D, Munnich A, Rotig A et al (2002) Idebenone and reduced cardiac hypertrophy in Friedreich's ataxia. Heart 87(4):346–349. doi:10.1136/heart.87.4.346
Koht J, Tallaksen CM (2007) Cerebellar ataxia in the eastern and southern parts of Norway. Acta Neurol Scand 187:76–79. doi:10.1111/j.1600-0404.2007.00853.x
Nishizawa M (2001) Hereditary ataxias—overview. Rinsho shinkeigaku (Clin Neurol) 41(12):1114–1116
Zortea M, Armani M, Pastorello E, Nunez GF, Lombardi S, Tonello S et al (2004) Prevalence of inherited ataxias in the province of Padua, Italy. Neuroepidemiology 23(6):275–280. doi:10.1159/000080092
Rasmussen A, Gomez M, Alonso E, Bidichandani SI (2006) Clinical heterogeneity of recessive ataxia in the Mexican population. J Neurol Neurosurg Psychiatry 77(12):1370–1372. doi:10.1136/jnnp.2006.090449
Rotig A, Sidi D, Munnich A, Rustin P (2002) Molecular insights into Friedreich's ataxia and antioxidant-based therapies. Trends Mol Med 8(5):221–224. doi:10.1016/S1471-4914(02)02330-4 http://www.ncbi.nlm.nih.gov/sites/entrez?cmd=Retrieve&db=PubMed&list_uids=12067631&dopt=Abstract
Le Ber I, Bouslam N, Rivaud-Pechoux S, Guimaraes J, Benomar A, Chamayou C et al (2004) Frequency and phenotypic spectrum of ataxia with oculomotor apraxia 2: a clinical and genetic study in 18 patients. Brain 127(Pt 4):759–767. doi:10.1093/brain/awh080
Swift M, Morrell D, Cromartie E, Chamberlin AR, Skolnick MH, Bishop DT (1986) The incidence and gene frequency of ataxia–telangiectasia in the United States. Am J Hum Genet 39(5):573–583
Tavani F, Zimmerman RA, Berry GT, Sullivan K, Gatti R, Bingham P (2003) Ataxia–telangiectasia: the pattern of cerebellar atrophy on MRI. Neuroradiology 45(5):315–319
Wullner U, Klockgether T, Petersen D, Naegele T, Dichgans J (1993) Magnetic resonance imaging in hereditary and idiopathic ataxia. Neurology 43(2):318–325
Le Ber I, Brice A, Durr A (2005) New autosomal recessive cerebellar ataxias with oculomotor apraxia. Curr Neurol Neurosci Rep 5(5):411–417. doi:10.1007/s11910-005-0066-4 http://www.ncbi.nlm.nih.gov/sites/entrez?cmd=Retrieve&db=PubMed&list_uids=16131425&dopt=Abstract
Date H, Onodera O, Tanaka H, Iwabuchi K, Uekawa K, Igarashi S et al (2001) Early-onset ataxia with ocular motor apraxia and hypoalbuminemia is caused by mutations in a new HIT superfamily gene. Nat Genet 29(2):184–188. doi:10.1038/ng1001-184
Anttonen AK, Mahjneh I, Hamalainen RH, Lagier-Tourenne C, Kopra O, Waris L et al (2005) The gene disrupted in Marinesco–Sjogren syndrome encodes SIL1, an HSPA5 cochaperone. Nat Genet 37(12):1309–1311. doi:10.1038/ng1677
Engert JC, Berube P, Mercier J, Dore C, Lepage P, Ge B et al (2000) ARSACS, a spastic ataxia common in northeastern Quebec, is caused by mutations in a new gene encoding an 11.5-kb ORF. Nat Genet 2:120–125. doi:10.1038/72769
Manto MU (2005) The wide spectrum of spinocerebellar ataxias (SCAs). Cerebellum 4(1):2–6. doi:10.1080/14734220510007914
Schols L, Bauer P, Schmidt T, Schulte T, Riess O (2004) Autosomal dominant cerebellar ataxias: clinical features, genetics, and pathogenesis. Lancet Neurol 3(5):291–304. doi:10.1016/S1474-4422(04)00737-9
Nagafuchi S, Yanagisawa H, Sato K, Shirayama T, Ohsaki E, Bundo M et al (1994) Dentatorubral and pallidoluysian atrophy expansion of an unstable CAG trinucleotide on chromosome 12p. Nat Genet 6(1):14–18. doi:10.1038/ng0194-14
Koide R, Ikeuchi T, Onodera O, Tanaka H, Igarashi S, Endo K et al (1994) Unstable expansion of CAG repeat in hereditary dentatorubral-pallidoluysian atrophy (DRPLA). Nat Genet 6(1):9–13. doi:10.1038/ng0194-9
McDonald ME, Ambrose CM, Duyao MP et al (1993) A novel gene containing a trinucleotide repeat that is expanded and unstable on Huntington's disease chromosomes. The Huntington's Disease Collaborative Research Group. Cell 72(6):971–983
Rampoldi L, Dobson-Stone C, Rubio JP, Danek A, Chalmers RM, Wood NW et al (2001) A conserved sorting-associated protein is mutant in chorea-acanthocytosis. Nat Genet 28(2):119–120. doi:10.1038/88821
Martin MH, Bouchard JP, Sylvain M, St-Onge O, Truchon S (2007) Autosomal recessive spastic ataxia of Charlevoix–Saguenay: a report of MR imaging in 5 patients. AJNR Am J Neuroradiol 28(8):1606–1608. doi:10.3174/ajnr.A0603
Anheim M, Chaigne D, Fleury M, Santorelli FM, De Seze J, Durr A et al (2008) Autosomal recessive spastic ataxia of Charlevoix–Saguenay: study of a family and review of the literature. Rev Neurol (Paris) 164(4):363–368. doi:10.1016/j.neurol.2008.02.001
Anheim M, Fleury MC, Franques J, Moreira MC, Delaunoy JP, Stoppa-Lyonnet D et al (2008) Clinical and molecular findings of ataxia with oculomotor apraxia type 2 in 4 families. Arch Neurol 65(7):958–962. doi:10.1001/archneur.65.7.958
Tranchant C, Fleury M, Moreira MC, Koenig M, Warter JM (2003) Phenotypic variability of aprataxin gene mutations. Neurology 60(5):868–870
Cossee M, Schmitt M, Campuzano V, Reutenauer L, Moutou C, Mandel JL et al (1997) Evolution of the Friedreich’s ataxia trinucleotide repeat expansion: founder effect and premutations. Proc Natl Acad Sci U S A 94(14):7452–7457. doi:10.1073/pnas.94.14.7452
Epplen C, Epplen JT, Frank G, Miterski B, Santos EJ, Schols L (1997) Differential stability of the (GAA)n tract in the Friedreich ataxia (STM7) gene. Hum Genet 99(6):834–836. doi:10.1007/s004390050458
Schmitz-Hubsch T, du Montcel ST, Baliko L, Berciano J, Boesch S, Depondt C et al (2006) Scale for the assessment and rating of ataxia: development of a new clinical scale. Neurology 66(11):1717–1720. doi:10.1212/01.wnl.0000219042.60538.92
Yabe I, Matsushima M, Soma H, Basri R, Sasaki H (2008) Usefulness of the Scale for Assessment and Rating of Ataxia (SARA). J Neurol Sci 266(1-2):164–166. doi:10.1016/j.jns.2007.09.021
Fahey MC, Corben L, Collins V, Churchyard AJ, Delatycki MB (2007) How is disease progress in Friedreich’s ataxia best measured? A study of four rating scales. J Neurol Neurosurg Psychiatry 78(4):411–413. doi:10.1136/jnnp.2006.096008
du Montcel ST, Charles P, Ribai P, Goizet C, Le Bayon A, Labauge P et al (2008) Composite cerebellar functional severity score: validation of a quantitative score of cerebellar impairment. Brain 131(Pt 5):1352–1361. doi:10.1093/brain/awn059
Mascalchi M, Salvi F, Piacentini S, Bartolozzi C (1994) Friedreich’s ataxia: MR findings involving the cervical portion of the spinal cord. AJR Am J Roentgenol 163(1):187–191
Bhidayasiri R, Perlman SL, Pulst SM, Geschwind DH (2005) Late-onset Friedreich ataxia: phenotypic analysis, magnetic resonance imaging findings, and review of the literature. Arch Neurol 62(12):1865–1869. doi:10.1001/archneur.62.12.1865
Gros-Louis F, Dupre N, Dion P, Fox MA, Laurent S, Verreault S et al (2007) Mutations in SYNE1 lead to a newly discovered form of autosomal recessive cerebellar ataxia. Nat Genet 39(1):80–85. doi:10.1038/ng1927
Dupre N, Gros-Louis F, Chrestian N, Verreault S, Brunet D, de Verteuil D et al (2007) Clinical and genetic study of autosomal recessive cerebellar ataxia type 1. Ann Neurol 62(1):93–98. doi:10.1002/ana.21143
Thiffault I, Tetreault M, Allyson J, Gosselin I, Loiselle L, Mathieu J, Bouchard JP, Lessage J, Brais B. Identification and characterization of a new locus responsible for recessive late-onset cerebellar ataxia (LOCA). ASHG San Diego, CA, 2007 Oct 23–27:355A [1825].
El Euch-Fayache G, Lalani I, Amouri R, Turki I, Ouahchi K, Hentati A et al (2003) Phenotypic features and genetic findings in sacsin related autosomal recessive ataxia in Tunisia. Arch Neurol 60:982–988
Criscuolo C, Banfi S, Orio M, Gasparini P, Monticelli A, Scarano V et al (2004) A novel mutation in SACS gene in a family from southern Italy. Neurology 62(1):100–102
Ogawa T, Takiyama Y, Sakoe K, Mori K, Namekawa M, Shimazaki H et al (2004) Identification of a SACS gene missense mutation in ARSACS. Neurology 62(1):107–109
Bouchard JP, Barbeau A, Bouchard R, Bouchard RW (1978) Autosomal recessive spastic ataxia of Charlevoix–Saguenay. Can J Neurol Sci 5(1):61–69
Acknowledgements
This study was supported by funds from the Institut National de la Santé et de la Recherche Scientifique, the Centre National de la Recherche Scientifique, the Hôpitaux Universitaires de Strasbourg (PHRC régional to C.T.) and the Agence Nationale pour la Recherche-Maladies Rares (ANR-MRAR to M.K.). B. M. is supported by the GIS-Maladies Rares.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Anheim, M., Fleury, M., Monga, B. et al. Epidemiological, clinical, paraclinical and molecular study of a cohort of 102 patients affected with autosomal recessive progressive cerebellar ataxia from Alsace, Eastern France: implications for clinical management. Neurogenetics 11, 1–12 (2010). https://doi.org/10.1007/s10048-009-0196-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10048-009-0196-y