Abstract
This systematic review and meta-analysis aim to evaluate the remission rate of patients with rheumatoid arthritis (RA) in real-world studies and to summarize potential predictors of remission in RA. Studies reporting remission rate in patients with RA were searched from MEDLINE, EMBASE, and Scopus databases. Two reviewers independently assessed all studies according to eligibility criteria and extracted data. Generally, observational studies reporting remission rate in adult (≥ 18 years) patients with RA were included. Quality assessments were performed using the Newcastle-Ottawa Scale. Pooled analyses of remission rate were conducted using a random-effects model and data were analyzed in subgroups to identify potential source of heterogeneity. Sensitivity analyses were performed by serially excluding each study. Potential predictors of remission were summarized. Thirty-one studies with ~ 82,450 RA patients in total were included. Using the DAS28 remission criteria, the pooled 3-, 6-, 12-, and 24-month remission rates were 17.2%, 16.3%, 21.5%, and 23.5%, respectively. Subgroup analyses showed that 11.7% and 13.8% of TNFi inadequate responders reached remission after 6- and 12-month use of non-TNFi biologics. Predictors of remission included male, higher education level, and lower baseline disease activity, while initial use of corticosteroids was negative predictors of remission. Sustained remission was rare regardless of different criteria used. Remission was a reachable target in real-world studies, while attention should also be paid to achieve sustained remission.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rheumatoid arthritis (RA) is a chronic inflammatory rheumatic disease leading to joint destruction, extra-articular manifestations, and systematic comorbidities. It is associated with progressive disability, increased mortality, and socioeconomic costs [1]. According to the treat-to-target (T2T) strategy, which was recommended by international task force American College of Rheumatology (ACR) and European League Against Rheumatism (EULAR), the primary target for RA patients is clinical remission or low disease activity (LDA). Remission is defined as the absence of signs and symptoms of significant inflammatory disease in patients with RA [2], which can be measured by criteria like DAS28, CDAI, SDAI, and 2011 ACR/EULAR criteria.
Real-world evidence (RWE) generally refers to information coming from electronic health records, billing data, registries, but not traditional tightly controlled trials [3]. Selected patients with higher adherence, more severe RA activity, and shorter study durations make it difficult for trials to generalize findings in larger and “random” population of patients in clinical practice. There have been many well-designed registries worldwide studying remission status of patients with RA for more than 30 years [4,5,6,7,8,9,10,11,12,13,14]. But we have insufficient knowledge of how frequently patients achieve remission and whether this “target” is practical or achievable in real-world circumstances as no meta-analysis of remission rate in real-world studies have been carried out. Herein, we conducted a meta-analysis and systematic review of published cohort studies to investigate remission rate and substantial predictors of remission in RA patients in real-world studies and to enhance the T2T strategy into daily practice.
Materials and methods
This meta-analysis was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement protocol [15].
Inclusion and exclusion criteria
Studies that met the following criteria were included:
-
1)
Conducted in adult patients (≥ 18 years) with a diagnosis of RA according to the American College of Rheumatology (ACR) RA classification criteria;
-
2)
Reported remission rates according to different sets of indexes;
-
3)
Prospective cohort studies or consecutive cross-sectional studies. Consecutive cross-sectional studies were defined as an observational study with consecutive patients and reported remission rate of the whole cohort each year. Cross-sectional studies were included in systematic review but not in meta-analysis;
-
4)
Carried out longitudinally and followed up patients for at least 3 months.
Studies that met any of the following criteria were excluded: (1) carried out in patients with any combined rheumatic diseases (like systematic erythematous lupus, Sjogren’s syndrome, dermatomyositis); (2) point remission rate studies where patients had only one visit; (3) Randomized controlled trials, review articles; (4) conference abstracts, as the limited data available in abstracts may hinder ability to assess the quality of study and data.
Literature search and study selection
We searched MEDLINE, EMBASE, and Scopus to identify all potential articles reporting remission rates in patients with RA. Details of search terms and strategies can be found in Supplementary Materials. The eligibility of the reference list retrieved by literature search was assessed independently by two reviewers and disagreements were resolved at each step by consensus. Selected articles were further examined to determine if they contained relevant information.
Data extraction
Data were extracted from the selected studies independently by two authors, using a predefined standardized form according to the Cochrane Handbook. Discrepancies were discussed by the two authors and arbitrated by a third independent reviewer. For each study, the following information were identified by two of the authors: study type, time span, mean follow-up time, baseline data of patients including age, gender, country, clinical characteristics (including disease duration, tender joint counts, swelling joint counts, rheumatoid factor positivity, mean DAS at baseline, remission rate), treatment regime, and predictors of remission. When the available information from the selected studies was incomplete, attempts were made to contact the corresponding authors for additional information. Data given in subgroups from one study were recalculated into one group before meta-analysis to balance their weights in meta-analysis. Sustained remission was defined as being in remission for at least twice in the observation period.
Quality assessment
Quality assessment (Table S1) of each study was performed independently by the two authors, using the Newcastle-Ottawa Scale (http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp), which graded studies according to the quality of selection, comparability, and outcome of study participants. Discrepancies were addressed by re-evaluation of the original article and discussion with a third independent reviewer.
Statistical analysis
We assessed the pooled remission rates of selected cohort studies at 3, 6, 12, and 24 months. Remission rates using different criteria were also listed. We employed a random-effects model to account for heterogeneity between studies in our sample when estimating the common effect size. Statistical evidence of heterogeneity across studies was examined using the Cochrane Q test and the Ι2 statistic. To identify potential sources of heterogeneity in remission rates reported, pre-specified subgroup analyses were conducted according to disease activity criteria, follow-up duration, geographical region, disease duration, sample size, use of biologic DMARDs (bDMARDs), and type of bDMARDs used. Sensitivity analyses were performed by serially excluding each study to evaluate its influence on the overall results. Publication bias was assessed using funnel plots and the Egger’s test. All analyses were performed using Stata Version 14.0 (StataCorp, Texas, USA), and a p value of less than 0.05 was considered statistically significant. In the summary of potential predictive factors of remission, only results from multivariate analysis (multiple linear logistic regression or Cox proportional hazards model) were included.
Availability of data and material
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Results
Literature search
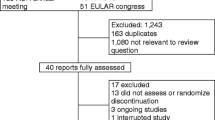
The search of MEDLINE, EMBASE, and Scopus databases up to November 17, 2017 resulted in a total of 8323 articles, of which 6782 remained after duplicates were removed. A total of 4596 articles that did not meet the inclusion criteria were excluded after title and abstract screening and the 441 remaining articles were reviewed for full texts. Finally, 31 studies including ~ 82,450 patients were selected. Twelve studies were included in subsequent meta-analysis, and all 31 studies were included in qualitative analysis. A flowchart of article screening for the systematic review has been illustrated in Fig. 1.
Study characteristics
For included studies, 19 in Europe, 7 in North America, 1 in Asia, 2 in South America, 1 in Africa, and 1 registry in Oceania were included (Table 1). The METEOR registry was carried out in 32 countries, including countries in Europe and Asia (Japan and India). The 31 included studies were mostly carried out in the first 15 years of the twenty-first century and were published between 2006 and 2017.
Main characteristics of the 31 selected studies were summarized in Table 1. Mean age was between 50 to 60 in 29/31 studies. Gender distribution was similar across registries (ranged from 64 to 88.8%), except that 90% patients in the VARA registry were male. Differences in patients’ characteristics were noticed, mainly in disease duration (mean duration ranged from 5.9 months to 16.6 years), disease activity at baseline (mean DAS ranged from 3.15 to 6.7), and treatment strategies. General treatment strategies were similar among studies, though variance existed. Methotrexate were used in 28 cohorts, percent of patients on MTX ranged from 40.9 to 97.7%. Glucocorticoids (GCs) were used in 15 studies, and proportions of patients on GCs ranged from 31.0 to 84.1%. Though most studies contained patients in cs-/bDMARDs monotherapy or combination therapy, there were both studies where every patient was on biologics and studies where no patient was receiving TNFis or non-TNFi biologics.
Remission rate
Ranges of remission rates according to their remission criteria, grouped by corresponding follow-up duration, were summarized in Table S3, where a trend of remission rate increasing with follow-up duration was roughly noticed.
DAS28
Twenty-one registries reported remission rate according to DAS28 criteria, making it the most frequently used criteria (Table S3). Pooled remission rates (DAS28 < 2.6) were 17.2%, 16.3%, 21.5%, and 23.5% for 3-, 6-, 12-, and 24-month follow-ups, respectively (Fig. 2). Significant heterogeneity among studies was noted (I2 ranged from 83.5 to 96.8%). Further subgroup analyses were conducted for the 6- and 12-month remission rates. Regarding treatment strategies (Table S4), all patients from 6-month group were treated with bDMARDs. Subgroup analyses showed that patients who received TNFi (I2 97.1%, p 0.000) had higher remission rate than patients who received non-TNFi biologics (I2 0.0%, p 0.687). For the 12-month group, 26.1% of TNFi patients (I2 91.6%, p 0.000) reached remission while 13.8% of non-TNFi patients reached remission (I2 67.2%, p 0.081). Subgroup analyses by geographical region, disease duration, sample size, and biologics use showed no significant change in heterogeneity (results not shown). Rate of remission or LDA (DAS28 < 3.2) ranged from 35.0 to 61.7% for 6 months, 31.6 to 55.0% for 12 months, and stabled at around 64% for 24, 36, and 60 months, respectively.
Sensitivity analysis and assessment of publication bias
Sensitivity analysis (Table S2) suggested that the 3-, 6-, 12-, and 24-month remission rate was stable and omitting a single study did not change the significance of the pooled survival rates, while removal of the study by Couderc et al. led to the largest increase in the 24-month remission rate. Visual inspection of the funnel plots revealed mild to moderate asymmetry (Fig. S1). According to the Egger’s test, there was no evidence of publication bias in studies reporting on remission rates of 3-, 6-, 12-, and 24-month.
Predictors of remission
We summarized significant predictors of remission reported by the included studies (Table 2). Though predictors varied across studies, some of them remained consistent.
-
1)
Gender, five studies showed that male was an independent predictor of remission.
-
2)
Education level, higher level of education is considered as an independent predictor of remission in two studies.
-
3)
Baseline clinical characteristics, eight studies addressed clinical characteristics at baseline as independent predictors. Lower TJC28, lower disease activity, and lower HAQ at baseline were positively associated with remission, while higher baseline PhGA, PtGA, HAQ, SJC28, ESR predicted lower remission rate.
-
4)
Glucocorticoids use at baseline, three studies found that GC use at baseline predicted a reduced likelihood of treatment response.
Sustained remission
Eight studies reported sustained remission rates (Table 3). Although no agreement has been reached, sustained remission is commonly defined in two ways: (1) remission at two consecutive visits (with certain period apart), or (2) remission lasted a certain of time after the first one. Generally, sustained remission for 1 year occurred in 7.7–37.0%, 19.6–31.3%, 16.7–27.1%, and 23.8% patients according to DAS28, SDAI, CDAI, and ACR/EULAR remission criteria.
Discussion
It is important to know how real-world RA patients are managed as reaching the target of clinical remission or LDA is associated with better long-term prognosis [39]. Many studies have reported remission rates and relevant predictors in individual studies, but to our knowledge, this is the first systematic review and meta-analysis to investigate the pooled remission rates in patients with RA from real-world longitudinal studies. Scott et al. [40] reviewed remission of patients with early RA from 17 observational studies and 20 RCTs, and found a successive decrease in remission rate through patients from RCTs receiving DMARD combination therapies (42% for DAS criteria), patients from observational studies (33%), and patients from RCTs receiving DMARD monotherapy (26%). Though carried out in early RA patients, the observational studies group showed similar remission rate with our study. Patients in RCTs may have higher remission rate than observational studies due to reasons like better compliance, regularly arranged follow-ups, better access to certain high-cost drugs, and less heterogeneity. But results from RCTs are strictly restricted within certain patients that cannot be generalized. In observational studies, a trend of increasing remission rate with follow-up duration was seen in both longitudinal (Table S3) and consecutive cross-sectional cohorts (Fig. 3). Remission is a reachable target in real-life patients and real-world studies are providing tremendous evidence.
We have tried to find potential sources of heterogeneity by sensitivity analysis and subgroup analysis according to follow-up duration, remission criteria, geographical region, and treatment strategies. In both 6- and 12-month group, patients treated with TNFi had higher remission rate than non-TNFi group. Both studies [22, 24] included patients who had previous TNFi failures for non-TNFi treatment. Though only one tenth of patients reached remission, it proved the efficacy of non-TNFi biologics on patients inadequately responded to TNFi. This is consistent with another meta-analysis which showed that switching to non-TNFi was more effective than cycling among TNFis [41].
Our study approved traditional predictors of remission like male, higher educational level, lower TJC28, lower baseline disease activity, and lower HAQ. But we also found controversies. Three studies reported that younger age was a predictor of remission [16, 29, 31] while Lahaye et al. [24] found that younger age does not predict remission but less adverse effects and complications. Smoking has also been a traditional negative predictor of remission [42], but we found that there may be no difference between smokers and non-smokers. Canhao et al. [30] reported that smoking predicted reduced remission rate while Kuriya et al. [5] found no significant difference among current or ex-smokers and never smokers. Patients with negative predictors, like older age and lower educational level, should receive strengthened therapies as they are less likely to achieve remission. Stratified therapies for individual patient should be noted on the basis of international guidelines. Three studies showed that initial use of GCs predicts worse prognosis [5, 29, 30]. All three studies explained that initial use of GCs may introduce channeling bias as doctors tended to prescribe GCs to patients less likely to achieve remission with higher baseline disease activity [43].
Sustained remission was rare in included studies regardless of different definitions. In the VARA registry, probability of remaining in remission for 3, 12 and 24 months after the first remission were 86.3%, 24.7%, and 8.1% (DAS28), respectively. They also reported that probability of a remission lasting for 2 years was 6.0–14.1%. We have worked so hard to treat patients to remission, but transient remission is not our target. More attention should be paid on maintaining remission and enhancing sustained remission rate. Predictors for sustained remission (SR) were also summarized. Some SR predictors were in accordance with that of remission: male gender, lower baseline disease activity [31], lower PhGA [23], and initial use of combination DMARDs [5]. Darawankul et al. [38] reported that in multivariate regression analysis, only a good EULAR response at the first year was significantly associated with SR (OR 3.1, 95% CI 1.15–8.36, p = 0.03). Negatively associated predictors were higher TJC [23], initial use of oral steroids, baseline pain, and longer time to remission [5]. Kuriya et al. [5] found that being obese (OR 0.30 95% CI [0.10–0.90], p = 0.002) predicted worse outcomes in patients with RA, while association of BMI and remission was not identified in other included studies. Association of other variates, including early diagnosis, RF negativity, no erosion on X-ray at baseline, and ever prednisolone use with SR, were not significant.
Some registries illustrated how disease activity changed over time by reporting consecutive cross-sectional remission rates, though not included in quantitative analysis. For each registry, cross-sectional remission rate (DAS28) increased with years (Fig. 3). Yamanaka et al. [7] reported that from 2000 to 2006, remission rate defined by DAS28 increased from 8.5 to 21.5%, and patients in LDA increased from 22.2 to 38.8%. Not only mean DAS28, but also all four components TJC, SJC, ESR, and PtGA had also improved from 2000 to 2006. In the report of Hyrich et al. [4], both the proportions of 1-year EULAR good responders and remission rate increased from 2001 to 2008 (8% vs. 17%, p < 0.001). Aga et al. [14] reported a twofold increase of remission rate in the 6-month follow-up group from 2000 to 2010, and RA disease activity level at MTX and TNFi+MTX initiation decreased from high to moderate at the mean time. Littlejohn et al. [11] reported that the remission rate increased from 36.7% in 2009 to 53.5% in 2014 (DAS28 criteria). They also addressed that most disease activity change happened in the first 3 years of diagnosis. Greenberg et al. [36] pointed out that according to their two-phase (2005–2007 and 2010–2012) study, improvements in disease activity and remission rate were seen among all racial and ethnic groups.
This study has several limitations. First, as studies were designed, carried out, and reported differently, heterogeneity among studies was significant. Verstappen et al. [9] compared demographic and clinical characteristics in five registries (CORRONA, SRR, NOAR, IORRA, and CORRONA International) and found it difficult to compare data across registries. They have found a solution of collecting original data and redivide patients into subgroups by treatment response. Some registries that recruit international patients (like the METEOR registry in 32 countries) found that geographical variance was significant in patients with RA [13]. Radner et al. [44] have recently reported 2017 EULAR recommendations for a core data set in RA observational research, which has listed the least content variables so that data setup will be more standardized and comparable in RA registries. Second, generalizability is limited as some large, bDMARDs-based registries may introduce channeling bias as more patients receiving biologics were included [6, 29, 37, 45]. Third, as we only included patients with at least 3 months follow-up, some well-designed registries with only one cross-sectional remission rate reported have been ruled out and a lot of patients may be lost in this way.
Conclusions
Rate of remission increased with longer follow-up duration. Though remission rate has been elevated in recent years, sustained remission is still rare. Remission was more frequently achieved in patients who were male, with younger age, higher education level, and lower baseline disease activity, while initial use of corticosteroids reduced the likelihood of remission. Remission is a reachable target for patients with RA, and further efforts on maintaining remission and achieving sustained remission should be paid.
References
Smolen JS, Aletaha D, McInnes IB (2016) Rheumatoid arthritis. Lancet 388(10055):2023–2038
Smolen JS, Landewe R, Bijlsma J et al (2017) EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2016 update. Ann Rheum Dis 76(6):960–977
Sherman RE, Anderson SA, Dal Pan GJ, Gray GW, Gross T, Hunter NL, LaVange L, Marinac-Dabic D, Marks PW, Robb MA, Shuren J, Temple R, Woodcock J, Yue LQ, Califf RM (2016) Real-world evidence - what is it and what can it tell us? N Engl J Med 375(23):2293–2297
Hyrich KL, Watson KD, Lunt M, Symmons DP, British Society for Rheumatology Biologics R (2011) Changes in disease characteristics and response rates among patients in the United Kingdom starting anti-tumour necrosis factor therapy for rheumatoid arthritis between 2001 and 2008. Rheumatology (Oxford) 50(1):117–123
Kuriya B, Xiong J, Boire G, Haraoui B, Hitchon C, Pope J, Thorne JC, Tin D, Keystone EC, Bykerk V, for the CATCH Investigators, Ahluwalia V, Akhavan P, Arbillaga H, Baron M, Bell M, Bensen W, Boire G, Bykerk V, Cividino A, Colmegna I, Haraoui P, Hitchon C, Jamal S, Keystone E, Klinkhoff A, Kraishi M, Larche M, Lyddell C, Menard H, Mosher D, Nair B, Norris E, Penney C, Pope J, Rubin L, Shaw E, Sutton E, Thorne JC, Zummer M (2014) Earlier time to remission predicts sustained clinical remission in early rheumatoid arthritis--results from the Canadian Early Arthritis Cohort (CATCH). J Rheumatol 41(11):2161–2166
Chatzidionysiou K, Askling J, Eriksson J, Kristensen LE, van Vollenhoven R, group A (2015) Effectiveness of TNF inhibitor switch in RA: results from the national Swedish register. Ann Rheum Dis 74(5):890–896
Yamanaka H, Inoue E, Singh G, Tanaka E, Nakajima A, Taniguchi A, Hara M, Tomatsu T, Kamatani N (2007) Improvement of disease activity of rheumatoid arthritis patients from 2000 to 2006 in a large observational cohort study IORRA in Japan. Mod Rheumatol 17(4):283–289
Sung YK, Cho SK, Choi CB, Park SY, Shim J, Ahn JK, Bang SY, Cha HS, Choe JY, Chung WT, Her M, Hong SJ, Hong YK, Joung CI, Jun JB, Jung YO, Kang YM, Kim DY, Kim HR, Kim HA, Kim J, Kim SK, Kim SI, Kim TH, Kim TJ, Koh E, Lee CK, Lee HS, Lee J, Lee SH, Lee SH, Lee SS, Lee SW, Lee YA, Nah SS, Park SH, Sheen DH, Shim SC, Gyu Song G, Suh CH, Uhm WS, Yoo DH, Yoo WH, Yoon BY, Bae SC (2012) Korean Observational Study Network for Arthritis (KORONA): establishment of a prospective multicenter cohort for rheumatoid arthritis in South Korea. Semin Arthritis Rheum 41(6):745–751
Verstappen SM, Askling J, Berglind N et al (2015) Methodological challenges when comparing demographic and clinical characteristics of international observational registries. Arthritis Care Res (Hoboken) 67(12):1637–1645
Hetland ML, Jensen DV, Krogh NS (2014) Monitoring patients with rheumatoid arthritis in routine care: experiences from a treat-to-target strategy using the DANBIO registry. Clin Exp Rheumatol 32(5 Suppl 85):S141–S146
Littlejohn G, Roberts L, Bird P, de Jager J, Griffiths H, Nicholls D, Young J, Zochling J, Tymms KE (2015) Patients with rheumatoid arthritis in the Australian OPAL cohort show significant improvement in disease activity over 5 years: a multicenter observational study. J Rheumatol 42(9):1603–1609
Kristensen LE, Kapetanovic MC, Gulfe A, Soderlin M, Saxne T, Geborek P (2008) Predictors of response to anti-TNF therapy according to ACR and EULAR criteria in patients with established RA: results from the south Swedish arthritis treatment group register. Rheumatology (Oxford) 47(4):495–499
Navarro-Compan V, Smolen JS, Huizinga TW et al (2015) Quality indicators in rheumatoid arthritis: results from the METEOR database. Rheumatology (Oxford) 54(9):1630–1639
Aga AB, Lie E, Uhlig T, Olsen IC, Wierød A, Kalstad S, Rødevand E, Mikkelsen K, Kvien TK, Haavardsholm EA (2015) Time trends in disease activity, response and remission rates in rheumatoid arthritis during the past decade: results from the NOR-DMARD study 2000–2010. Ann Rheum Dis 74(2):381–388
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097
Balogh E, Madruga Dias J, Orr C et al (2013) Comparison of remission criteria in a tumour necrosis factor inhibitor treated rheumatoid arthritis longitudinal cohort: patient global health is a confounder. Arthritis Res Ther. 15(6):R221
Benbouazza K, Rkain H, Benchekroun B, Amine B, Bzami F, Benbrahim L, Atouf O, Essakalli M, Abouqal R, Dougados M, Hajjaj-Hassouni N (2012) Remission in early rheumatoid arthritis treated with conventional DMARDs. Results of a two-year follow-up study of El Ayachi Moroccan cohort. Joint Bone Spine 79(1):43–46
Brenol CV, da Chakr RM, Andrade NP et al (2015) Daily practice feasibility and effectiveness of treating long-standing rheumatoid arthritis to target with synthetic disease-modifying antirheumatic drugs: a prospective cohort study. Clin Rheumatol 34(10):1781–1785
Thorne C, Bensen WG, Choquette D, Chow A, Khraishi M, Atkins CJ, Kelsall JT, Lehman AJ, Shawi M, Khalil H, Nantel F, Rampakakis E, Sampalis JS, Otawa S (2014) Effectiveness and safety of infliximab in rheumatoid arthritis: analysis from a Canadian multicenter prospective observational registry. Arthritis Care Res (Hoboken). 66(8):1142–1151
Alemao E, Joo S, Kawabata H, al MJ, Allison PD, Rutten-van Mölken MPMH, Frits ML, Iannaccone CK, Shadick NA, Weinblatt ME (2016) Effects of achieving target measures in rheumatoid arthritis on functional status, quality of life, and resource utilization: analysis of clinical practice data. Arthritis Care Res (Hoboken). 68(3):308–317
Kovalchik SA, Charles-Schoeman C, Khanna D, Paulus HE (2012) An association study of disease activity score components and patient satisfaction with overall health for early RA patients on non-biologic DMARD therapy. Rheumatol Int 32(9):2725–2729
Couderc M, Gottenberg JE, Mariette X, Pereira B, Bardin T, Cantagrel A, Combe B, Dougados M, Flipo RM, le Loet X, Shaeverbeke T, Ravaud P, Soubrier M, on behalf of Club Rhumatismes et Inflammations (2014) Influence of gender on response to rituximab in patients with rheumatoid arthritis: results from the autoimmunity and rituximab registry. Rheumatology (Oxford) 53(10):1788–1793
Barnabe C, Homik J, Barr SG, Martin L, Maksymowych WP (2014) The effect of different remission definitions on identification of predictors of both point and sustained remission in rheumatoid arthritis treated with anti-TNF therapy. J Rheumatol 41(8):1607–1613
Lahaye C, Soubrier M, Mulliez A, Bardin T, Cantagrel A, Combe B, Dougados M, Flipo RM, le Loët X, Shaeverbeke T, Ravaud P, Mariette X, Gottenberg JE, French Society of Rheumatology (2016) Effectiveness and safety of abatacept in elderly patients with rheumatoid arthritis enrolled in the French Society of Rheumatology's ORA registry. Rheumatology (Oxford) 55(5):874–882
de Punder YM, Fransen J, Kievit W et al (2012) The prevalence of clinical remission in RA patients treated with anti-TNF: results from the Dutch rheumatoid arthritis monitoring (DREAM) registry. Rheumatology (Oxford) 51(9):1610–1617
Atzeni F, Antivalle M, Pallavicini FB, Caporali R, Bazzani C, Gorla R, Favalli EG, Marchesoni A, Sarzi-Puttini P (2009) Predicting response to anti-TNF treatment in rheumatoid arthritis patients. Autoimmun Rev 8(5):431–437
Rannio T, Asikainen J, Kokko A, Hannonen P, Sokka T (2016) Early remission is a realistic target in a majority of patients with DMARD-naive rheumatoid arthritis. J Rheumatol 43(4):699–706
Ciubotariu E, Gabay C, Finckh A, Physicians of the Swiss Clinical Quality Management Program for Rheumatoid A (2014) Joint damage progression in patients with rheumatoid arthritis in clinical remission: do biologics perform better than synthetic antirheumatic drugs? J Rheumatol 41(8):1576–1582
Flouri I, Markatseli TE, Voulgari PV, Boki KA, Papadopoulos I, Settas L, Zisopoulos D, Skopouli FN, Iliopoulos A, Bertsias GK, Geborek P, Drosos AA, Boumpas DT, Sidiropoulos P (2014) Comparative effectiveness and survival of infliximab, adalimumab, and etanercept for rheumatoid arthritis patients in the Hellenic registry of biologics: low rates of remission and 5-year drug survival. Semin Arthritis Rheum 43(4):447–457
Canhao H, Rodrigues AM, Mourao AF, Martins F, Santos MJ, Canas-Silva J, Polido-Pereira J, Pereira Silva JA, Costa JA, Araujo D, Silva C, Santos H, Duarte C, da Silva JAP, Pimentel-Santos FM, Branco JC, Karlson EW, Fonseca JE, Solomon DH (2012) Comparative effectiveness and predictors of response to tumour necrosis factor inhibitor therapies in rheumatoid arthritis. Rheumatology (Oxford) 51(11):2020–2026
Contreras-Yanez I, Pascual-Ramos V (2015) Window of opportunity to achieve major outcomes in early rheumatoid arthritis patients: how persistence with therapy matters. Arthritis Res Ther 17(1):177
Shahouri SH, Michaud K, Mikuls TR, Caplan L, Shaver TS, Anderson JD, Weidensaul DN, Busch RE, Wang S, Wolfe F (2011) Remission of rheumatoid arthritis in clinical practice: application of the American College of Rheumatology/European League Against Rheumatism 2011 remission criteria. Arthritis Rheum 63(11):3204–3215
Svensson B, Andersson ML, Bala SV, Forslind K, Hafstrom I, group Bs (2013) Long-term sustained remission in a cohort study of patients with rheumatoid arthritis: choice of remission criteria. BMJ Open 3(9):e003554
Mierau M, Schoels M, Gonda G, Fuchs J, Aletaha D, Smolen JS (2007) Assessing remission in clinical practice. Rheumatology (Oxford) 46(6):975–979
Listing J, Strangfeld A, Rau R, Kekow J, Gromnica-Ihle E, Klopsch T, Demary W, Burmester GR, Zink A (2006) Clinical and functional remission: even though biologics are superior to conventional DMARDs overall success rates remain low--results from RABBIT, the German biologics register. Arthritis Res Ther. 8(3):R66
Greenberg JD, Spruill TM, Shan Y, Reed G, Kremer JM, Potter J, Yazici Y, Ogedegbe G, Harrold LR (2013) Racial and ethnic disparities in disease activity in patients with rheumatoid arthritis. Am J Med 126(12):1089–1098
Hyrich KL, Watson KD, Silman AJ, Symmons DP, British Society for Rheumatology Biologics R (2006) Predictors of response to anti-TNF-alpha therapy among patients with rheumatoid arthritis: results from the British society for rheumatology biologics register. Rheumatology (Oxford) 45(12):1558–1565
Darawankul B, Chaiamnuay S, Pakchotanon R, Asavatanabodee P, Narongroeknawin P (2015) The good EULAR response at the first year is strongly predictive of clinical remission in rheumatoid arthritis: results from the TARAC cohort. Clin Rheumatol 34(1):43–49
Smolen JS, Breedveld FC, Burmester GR, Bykerk V, Dougados M, Emery P, Kvien TK, Navarro-Compán MV, Oliver S, Schoels M, Scholte-Voshaar M, Stamm T, Stoffer M, Takeuchi T, Aletaha D, Andreu JL, Aringer M, Bergman M, Betteridge N, Bijlsma H, Burkhardt H, Cardiel M, Combe B, Durez P, Fonseca JE, Gibofsky A, Gomez-Reino JJ, Graninger W, Hannonen P, Haraoui B, Kouloumas M, Landewe R, Martin-Mola E, Nash P, Ostergaard M, Östör A, Richards P, Sokka-Isler T, Thorne C, Tzioufas AG, van Vollenhoven R, de Wit M, van der Heijde D (2016) Treating rheumatoid arthritis to target: 2014 update of the recommendations of an international task force. Ann Rheum Dis 75(1):3–15
Ma MH, Scott IC, Kingsley GH, Scott DL (2010) Remission in early rheumatoid arthritis. J Rheumatol 37(7):1444–1453
Kim HL, Lee MY, Park SY, Park SK, Byun JH, Kwon S, Lee EK (2014) Comparative effectiveness of cycling of tumor necrosis factor-alpha (TNF-alpha) inhibitors versus switching to non-TNF biologics in rheumatoid arthritis patients with inadequate response to TNF-alpha inhibitor using a Bayesian approach. Arch Pharm Res 37(5):662–670
Cappelli LC, Konig MF, Gelber AC, Bingham CO 3rd, Darrah E (2018) Smoking is not linked to the development of anti-peptidylarginine deiminase 4 autoantibodies in rheumatoid arthritis. Arthritis Res Ther. 20(1):59
Black RJ, Lester S, Buchbinder R, Barrett C, Lassere M, March L, Whittle S, Hill CL (2017) Factors associated with oral glucocorticoid use in patients with rheumatoid arthritis: a drug use study from a prospective national biologics registry. Arthritis Res Ther. 19(1):253
Radner H, Chatzidionysiou K, Nikiphorou E, Gossec L, Hyrich KL, Zabalan C, van Eijk-Hustings Y, Williamson PR, Balanescu A, Burmester GR, Carmona L, Dougados M, Finckh A, Haugeberg G, Hetland ML, Oliver S, Porter D, Raza K, Ryan P, Santos MJ, van der Helm-van Mil A, van Riel P, von Krause G, Zavada J, Dixon WG, Askling J (2018) 2017 EULAR recommendations for a core data set to support observational research and clinical care in rheumatoid arthritis. Ann Rheum Dis 77(4):476–479
Valesini G, Montecucco C, Cutolo M (2006) Recommendations for the use of biologic (TNF-alpha blocking) agents in the treatment of rheumatoid arthritis in Italy. Clin Exp Rheumatol 24(4):413–423
Funding
This study was supported by the Chinese National Key Technology R&D Program (2017YFC0907601, 2017YFC0907604).
Author information
Authors and Affiliations
Contributions
CY, SYJ, YHW, and MTL designed the study and discussed on the search terms. CY and SYJ independently identified the search, reviewed the titles and abstracts, retrieved full articles to determine eligibility of each study, and extracted data from selected articles using a standardized form. Discrepancies were resolved at each step by consensus with a third reviewer (YHW). CY drafted the manuscript. NJ, CYW, QW, XPT, and XFZ revised the manuscript critically.
Corresponding authors
Ethics declarations
Ethical standards (human and animal rights)
Not applicable for database search results.
Disclosures
None.
Electronic supplementary material
ESM 1
(DOCX 122 kb)
Rights and permissions
About this article
Cite this article
Yu, C., Jin, S., Wang, Y. et al. Remission rate and predictors of remission in patients with rheumatoid arthritis under treat-to-target strategy in real-world studies: a systematic review and meta-analysis. Clin Rheumatol 38, 727–738 (2019). https://doi.org/10.1007/s10067-018-4340-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-018-4340-7