Abstract
To compare the preventive effect of tumor necrosis factor (TNF) inhibitors (anti-TNF antibody and soluble TNF receptor fusion protein (TNFR)) and nonsteroidal anti-inflammatory drugs (NSAIDs) on uveitis in patients with ankylosing spondylitis (AS). This retrospective cohort study included all AS patients (n = 1055) who have been treated with either TNF inhibitor or NSAIDs at the Seoul National University Hospital from 2004 to 2016. Treatment episodes of each patient were assigned to anti-TNF antibody (n = 517), TNFR (n = 341), and NSAID (n = 704) groups. The incidence of uveitis in each group was compared using a Cox proportional hazard model. The incidence rates of uveitis before and after initiation of TNF inhibitors were also assessed. A propensity score-matched (PSM) comparison was performed for a sensitivity analysis. Uveitis was significantly less common in the anti-TNF antibody group than the NSAID group (adjusted hazard ratio (HR) 0.53; 95% confidence interval (CI) 0.29–0.96) while it was higher in the TNFR group (adjusted HR 2.25, 95% CI 1.43–3.53). Anti-TNF antibody further reduced the incidence of uveitis when prescribed with NSAIDs (combination therapy) (adjusted HR 0.39; 95% CI 0.19–0.79). Combination therapy was preventive in AS patients with a history of uveitis (adjusted HR 0.31; 95% CI 0.12–0.81), but not in those without history of uveitis. The incidence rate of uveitis fell from 6.36 to 2.60 per 100 person-years when anti-TNF antibody was added to NSAIDs. Anti-TNF antibody plus NSAIDs reduces the risk of uveitis to a greater extent than NSAIDs alone in AS patients with a history of uveitis. Combination therapy may be an effective secondary prevention measure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Uveitis is a representative extra-articular manifestation of ankylosing spondylitis (AS) that can occur at any time during the disease course, or even before a diagnosis of AS [1]. Uveitis usually presents as an acute anterior form that affects the iris or the ciliary body and lasts for less than 3 months [2]. It is known to be more likely to occur in patients with AS who are male, are human leukocyte antigen B27 (HLA-B27) positive, or had previous uveitis [3,4,5]. Smokers were found to be at higher risk for infectious uveitis, but not for HLA-B27-associated uveitis [6]. Unfortunately, AS-related uveitis is common [7, 8] and can lead to ocular complications such as cataract, intraocular pressure-related problems, and visual impairment, ultimately reducing both vision and health-related quality of life [9, 10]. Therefore, prevention of uveitis in patients with AS, particularly those suffering recurrent attack, is of paramount importance.
A small, single retrospective study showed that nonsteroidal anti-inflammatory drugs (NSAIDs), a first-line therapy for AS [11, 12], reduce recurrence of acute anterior uveitis [13]. Tumor necrosis factor (TNF) inhibitors have been shown to be effective in reducing axial symptoms and are well tolerated in patients with AS, despite increased risk of latent tuberculosis reactivation and opportunistic infections [14, 15]. The anti-TNF antibodies are associated with a greater risk of infections than the chimeric soluble TNF receptor fusion protein (TNFR) [15]. Recently, several trials also examined the efficacy of TNF inhibitors for treating the extra-articular features of AS, including uveitis. They showed that anti-TNF antibodies, including infliximab and adalimumab, are more effective at preventing recurrence of uveitis than TNFR, etanercept [16,17,18,19,20].
However, there are no evidence-based guidelines for the management of extra-articular manifestations such as uveitis in AS patients. Also, no study has compared the efficacy of TNF inhibitors and NSAIDs for preventing recurrent uveitis in patients with AS. In this study, we evaluated the preventive effects of TNF inhibitors on uveitis in a cohort of AS patients compared to NSAIDs, to provide evidence for optimal management of recurrent uveitis.
Materials and methods
Patients and data collection
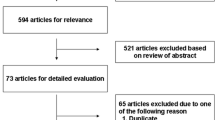
All of the patients with AS (n = 1055), who received at least one of medications at the Seoul National University Hospital from January 2004 through December 2016, were enrolled. A diagnosis of AS was based on the 1984 modified New York criteria [21]. The patients started with NSAIDs and could be switched to TNF inhibitors if they showed high disease activity (Bath Ankylosing Spondylitis Disease Activity Index [BASDAI] ≥ 4) despite treatment with NSAIDs for more than 3 months. Otherwise, NSAID treatment was maintained. Demographic information, including gender; age at the time of symptom onset; symptom duration; history of uveitis before treatment; smoking status; detailed treatment history including the use of NSAIDs, TNF inhibitors, and concomitant medications such as methotrexate (MTX), sulfasalazine, or systemic glucocorticoids; human leukocyte antigen B27 (HLA-B27) status; baseline erythrocyte sedimentation rate (ESR); and C-reactive protein (CRP) levels at the time of diagnosis, was collected from electronic medical records. The index of NSAID intake (NSAID index) was calculated based on dose, regimen, and prescription duration as recommended by the Assessment of SpondyloArthritis International Society (ASAS) [22]. The NSAID index < 50 was defined as low-dose NSAID and ≥ 50 as high-dose NSAID [23]. The exposure of TNF inhibitor was also quantified by calculating TNF inhibitor index as (actual prescribed dose / standard dose) × (standard dosing interval / actual dosing interval) × 100 [24]. Data was followed up until 31 December 2016. The study was approved by the institutional review board of the Seoul National University Hospital [IRB No. H-1607-111-777] and was conducted in accordance with the principles of the Declaration of Helsinki and Good Clinical Practice guidelines. Informed consent was waived due to the retrospective nature of the study.
Study design and outcomes
This study is a single-center retrospective cohort study on patients with AS. The primary objective of the study was to compare occurrence of uveitis in AS patients receiving TNF inhibitors and NSAIDs. The TNF inhibitor group was subdivided into an anti-TNF antibody group (adalimumab, infliximab, or golimumab) and TNFR group (etanercept). Since uveitis was significantly more common in the latter (Online Resource 1), following analysis was focused on the anti-TNF antibody group. NSAIDs included a selective cyclo-oxygenase-2 (COX-2) inhibitor (celecoxib) and non-selective COX inhibitors (aceclofenac, naproxen, meloxicam, indomethacin, diclofenac, morniflumate, nabumetone, etodolac, and piroxicam).
To reflect different treatments in one patient, analysis was based on “treatment episode.” Different variants of anti-TNF antibody were regarded as an anti-TNF antibody group and different types of NSAIDs were regarded as an NSAID group. The observation period for one treatment episode ran from the start of the intervention with one type of treatment to the occurrence of uveitis, discontinuation or change of treatment, death or loss of follow-up, or the right truncation, whichever came first.
The primary outcome was occurrence of uveitis during the treatment episodes. Uveitis event was defined as acute uveitis characterized by sudden onset and limited duration of 3 months or less, according to the standardized nomenclature for uveitis [25]. Uveitis was diagnosed when there were characteristic symptoms of uveitis and inflammatory cells were identified in anterior chamber with slit lamp microscopy by an ophthalmologist. A uveitis diagnosed outside the Seoul National University Hospital was also included if the diagnosis was made by an ophthalmologist. The uveitis with relapse in less than 3 months was regarded as a single event [25]. We compared the incidences of uveitis among the different treatments.
Subgroup analysis was performed according to the history of uveitis before treatment. To identify additive effects of TNF inhibitors plus NSAIDs, the effect of combination therapy (anti-TNF antibody + NSAIDs) was evaluated. Dose response was also evaluated according to combined NSAID index. To overcome differences in the baseline characteristics of individuals in each treatment group, the incidence rate of uveitis during TNF inhibitor treatment was compared with that during NSAIDs treatment in a subgroup of AS patients who started treatment with TNF inhibitors after NSAID treatment. Propensity score-matched (PSM) analysis was also performed between treatment with TNF inhibitors and NSAIDs as a sensitivity analysis.
Statistical analysis
Baseline characteristics of two treatment groups were compared using Student’s t test (continuous variables) or the Chi-square or Fisher’s exact tests (categorical variables). A Cox proportional hazard model was used to compare the hazard ratio (HR) with its 95% confidence interval (CI) for occurrence of uveitis during treatment episode with TNF inhibitors (anti-TNF antibody or TNFR) or NSAIDs. A crude HR and an adjusted HR (which reflected gender, age at the time of symptom onset, history of uveitis, HLA-B27 status, and baseline ESR) were calculated. Time-by-covariate interactions were used to test the proportional hazard assumption and restricted cubic spline functions to test the linear relationship between continuous variables. The robust sandwich covariance estimate was applied to adjust for the clustering effect of each individual during different treatment episodes in all analyses using treatment episodes.
The Cox proportional hazard regression model was then used to analyze subgroups according to a history of uveitis at the time of enrolment. The same analysis was performed to compare occurrence of uveitis in the TNF inhibitor combination therapy (anti-TNF antibody + NSAIDs or TNFR + NSAIDs) and NSAID monotherapy groups. For longitudinal comparison, the incidence rate (IR) was calculated per 100 patient-years as the number of incident uveitis events divided by total patient-years of follow-up for each treatment (NSAIDs or TNF inhibitor). Poisson regression was used to calculate incidence rate ratio (IRR) and its 95% CI.
1:1 propensity score matching was performed in the three groups (all treatment episodes, treatment episodes of patients with or without a history of uveitis) and standardized difference was used for comparison between the PSM NSAID and PSM anti-TNF antibody groups. All statistical analyses were performed using SPSS version 22.0 (IBM SPSS statistical software) and SAS version 9.4 (SAS Institute, Cary, NC). P < 0.05 was considered statistically significant.
Results
Patient characteristics
The baseline characteristics of the study population are summarized in Table 1. Among 1055 patients with AS, 620 were treated with NSAIDs only, while 435 patients changed to TNF inhibitors during the observation period. The mean treatment episode duration was 2.7 ± 2.6 years and mean follow-up duration for one patient was 4.3 ± 3.2 years. The percentage of HLA-B27-positive patients in both groups was similar. However, patients in the TNF inhibitor group had higher ESR and CRP levels at the time point of AS diagnosis (P < 0.001 for both). TNF inhibitor group also contained a higher percentage of patients with a history of uveitis before treatment (22.3 versus 15.3%; P = 0.004).
The 435 patients receiving TNF inhibitors experienced a total 858 treatment episodes: 517 (60.3%) treatment episodes belonged to the anti-TNF antibody group and 341 (39.7%) to the TNF receptor group (Table 2). The anti-TNF antibody group showed higher ESR and CRP levels than the NSAID group as the whole TNF inhibitor group. (P < 0.001 for both), but not the proportion of patients with a history of uveitis before treatment (P = 0.07).
Exposure to NSAIDs and TNF inhibitors
The mean NSAID index over treatment episode was 66.9 ± 31.6 in the NSAID group. NSAID was also used concomitantly with TNF inhibitors during 72.5% (375/517) and 72.4% (247/341) of treatment episodes in the anti-TNF antibody group and TNFR group, respectively. The mean concomitant NSAID index over treatment episodes was 32.3 ± 37.3 for the anti-TNF antibody group and 33.0 ± 35.9 for the TNF receptor group. Among the anti-TNF antibody group, adalimumab was most commonly used (319/517, 61.7%), followed by infliximab (144/517, 27.9%) and golimumab (54/517, 10.4%). The mean TNF inhibitor index over treatment episode was 89.0 ± 16.9 in the anti-TNF antibody group, and the standard dose was maintained in 311 (60.2%) treatment episodes.
Incidence of uveitis during treatment with TNF inhibitors versus NSAIDs
Uveitis occurred in 13.1% (92/704) of treatment episodes with NSAIDs, in 12.6% (65/517) with anti-TNF antibody, and in 30.5% (104/341) with TNFR treatment during the total follow-up. Since the occurrence of uveitis was significantly higher during TNFR treatment (Online Resource 1), we focused on anti-TNF antibody treatment in the following analyses.
Compared with NSAID treatment, the risk of uveitis was significantly lower during anti-TNF antibody treatment (adjusted HR 0.53, 95% CI 0.29–0.96) (Table 3). When the treatment episodes were stratified by history of uveitis before treatment, the preventive effect of anti-TNF antibody versus NSAIDs persisted for patients with a history of uveitis (adjusted HR 0.43, 95% CI 0.19–0.96), but disappeared in patients without history of uveitis (adjusted HR 0.84, 95% CI 0.41–1.76) (Table 3).
Combination treatment with anti-TNF antibody and NSAIDs
As patients with AS often use anti-TNF antibodies alongside NSAIDs, we compared the effect of combination therapy (anti-TNF antibody + NSAIDs) with that of NSAID monotherapy. Combination therapy resulted in 61% reduction in the risk of uveitis compared with NSAID monotherapy (adjusted HR 0.39, 95% CI 0.19–0.79) (Table 3). In addition, the preventive effect of combination therapy persisted in AS patients with a history of uveitis, resulting in 69% reduction in the risk of uveitis versus NSAID monotherapy (adjusted HR 0.31, 95% CI 0.12–0.81) (Table 3). Of note, there was no difference in the preventive effect on uveitis between anti-TNF antibody and NSAIDs in patients without history of uveitis, and this finding was true irrespective of whether anti-TNF antibody treatment was given alongside NSAIDs or not.
The effect of combination therapy was more prominent when high-dose NSAIDs were combined. The risk of uveitis during combination therapy with a high-dose NSAIDs plus an anti-TNF antibody was lower than that during combination therapy with a low-dose NSAIDs plus an anti-TNF antibody (adjusted HR 0.32, 95% CI 0.14–0.76 versus 0.51, 95% CI 0.28–0.92) (Table 4).
Even though the proportion of treatment episodes using sulfasalazine concomitantly was higher in the NSAID group than the anti-TNF antibody group, the preventive effect of combination therapy persisted in those without concomitant sulfasalazine (adjusted HR 0.55, 95% CI 0.32–0.93).
Incidence rates of uveitis after a change of treatment from NSAID to anti-TNF antibody
Overall, 390 patients in the TNF inhibitor group (and whose history of uveitis was ascertained in detail during NSAID treatment) took NSAIDs before the use of TNF inhibitors. Among these, 211 patients had received anti-TNF antibodies, but not TNF receptor. The incidence rate of uveitis in these 211 patients fell significantly by 46% after introduction of an anti-TNF antibody (IRR 0.54; 95% CI 0.34–0.84) (Fig. 1). The incidence rate of uveitis fell even further after switching to combination therapy from NSAID monotherapy (IRR 0.41; 95% CI 0.23–0.68) (Fig. 1). This effect of combination therapy persisted in a subgroup of patients with a history of uveitis (IRR 0.44; 95% CI 0.27–0.68).
Incidence rates of uveitis during NSAID treatment before anti-TNF antibody start and during anti-TNF antibody treatment in AS patients who received anti-TNF antibody monotherapy or combination therapy (a) and combination therapy only (b). Anti-TNF Ab, anti-tumor necrosis factor antibody; TNFi, tumor necrosis factor inhibitor; NSAIDs, nonsteroidal anti-inflammatory drugs
PSM analyses
PSM analysis was performed after adjusting for gender, age at the time of symptom onset, symptom duration, history of uveitis, HLA-B27 status, smoking status, baseline ESR, and CRP, and there were 216 PSM treatment episodes in each NSAID and anti-TNF antibody treatment group (Online Resource 3). The result of PSM in terms of primary outcome was consistent with the results of our primary comparison of data from NSAID and anti-TNF antibody treatment. The Cox proportional hazard model revealed that the combination of anti-TNF antibody and NSAID group showed a 51% reduction in the incidence of uveitis when compared with the PSM NSAID group (Table 3). Of note, combination therapy reduced the risk of uveitis to a greater extent than NSAIDs in a subgroup of patients with a history of uveitis (Table 3).
Discussion
Here, we showed that anti-TNF antibody was more effective than NSAIDs alone at suppressing uveitis attacks in patients with AS. The preventive effect was greatest when patients received a combination of anti-TNF antibody plus NSAIDs. The preventive effect of combination therapy persisted in AS patients with a history of uveitis, but not in patients without a history of uveitis. To the best of our knowledge, this is the first study to compare the ability of anti-TNF antibodies and NSAIDs to prevent uveitis in patients with AS.
Uveitis is the most common extra-articular manifestation of AS, irrespective of whether AS is HLA-B27-related or not [2]. It occurs in about 25% of patients and recurs frequently [1]. Sometimes, recurrent uveitis is a more annoying clinical problem than inflammatory back pain, leading to visual loss in patients with physical and mobility impairment. NSAIDs, sulfasalazine, or methotrexate reduces occurrence of uveitis in patients with AS [26,27,28], and recent studies showed similar effects for different TNF inhibitors on uveitis [4, 16,17,18]; however, optimal strategy to prevent recurrence of uveitis remains to be known.
Here, we found that TNFR (etanercept) was no better at preventing uveitis than anti-TNF antibody, which is consistent with other reports [18,19,20, 29, 30]. One possible explanation for this is that upregulation of the ability of T cells to produce TNFα via etanercept-induced counter-regulatory mechanism prevents apoptosis of inflammatory cells [31]. Another possible reason is that etanercept binds TNF and prevents its clearance from the eye [29, 32]. Therefore, a cautious approach is recommended when using soluble TNF receptor fusion protein to treat AS patients at risk of uveitis.
Anti-TNF antibody was significantly better than NSAIDs at prevention of uveitis; indeed, risk of uveitis reduced by 47% with anti-TNF antibody compared with NSAIDs. Anti-TNF antibodies are supposed to be effective because TNFα is a key inflammatory mediator responsible for the development of uveitis. TNFα levels in the serum and aqueous humor of patient with uveitis are elevated and correlate with disease activity of AS [33,34,35]. The greatest preventive effects were observed with combination treatment of anti-TNF antibody plus NSAIDs rather than with anti-TNF antibody alone. When high-dose NSAIDs were used alongside an anti-TNF antibody, protection was more pronounced. Consistent with our results, Gensler et al. reported that radiologic progression among AS patients who took TNF inhibitors plus high-dose NSAIDs was slower than that in patients taking TNF inhibitors alone (adjusted OR = 0.17, 95% CI 0.05–0.55, P = 0.003) [36].
Combination treatment with anti-TNF antibody plus NSAIDs effectively prevented uveitis in AS patients with a history of uveitis while there was no significant effect in patients without history of uveitis. The results suggest that combination therapy with an anti-TNF antibody plus NSAIDs is an optimal strategy for secondary prevention of uveitis, while NSAID therapy alone may be sufficient for primary prevention.
This study has several limitations due to its retrospective nature. First, a history of NSAID and TNF inhibitor treatment was solely based on medical records. Therefore, patient compliance cannot be measured. Second, episodes of uveitis were ascertained by review of hospital medical records; therefore, some cases could be missed if they were treated at another hospital. However, such cases were rare and, furthermore, the incidence rate of uveitis observed herein was very similar to that in the Swedish biologics register data [20]. Third, there was an imbalance between the baseline clinical characteristics of patients receiving TNF inhibitors and those receiving NSAIDs, which is an inherent limitation of a retrospective study. However, PSM analysis also showed that anti-TNF antibody treatment was effective. Furthermore, the effect of anti-TNF antibody was also observed in a longitudinal cohort in which NSAID therapy was switched to anti-TNF antibodies, suggesting that the results are valid even in balanced population between anti-TNF antibody and NSAIDs. Despite the consistency of the results, hidden confounder problems can be clearly addressed only by a randomized prospective study.
In conclusion, combination therapy with an anti-TNF antibody plus NSAIDs is more effective in reducing the risk of uveitis in AS patients than NSAIDs alone. Combination therapy is recommended for AS patients who suffer recurrent uveitis.
References
Stolwijk C, van Tubergen A, Castillo-Ortiz JD, Boonen A (2015) Prevalence of extra-articular manifestations in patients with ankylosing spondylitis: a systematic review and meta-analysis. Ann Rheum Dis 74(1):65–73
Muñoz-Fernández S, Martín-Mola E (2006) Uveitis. Best Pract Res Clin Rheumatol 20(3):487–505
Jaakkola E, Herzberg I, Laiho K, Barnardo MC, Pointon JJ, Kauppi M, Kaarela K, Tuomilehto-Wolf E, Tuomilehto J, Wordsworth BP (2006) Finnish HLA studies confirm the increased risk conferred by HLA-B27 homozygosity in ankylosing spondylitis. Ann Rheum Dis 65(6):775–780
Sieper J, Koenig A, Baumgartner S, Wishneski C, Foehl J, Vlahos B, Freundlich B (2010) Analysis of uveitis rates across all etanercept ankylosing spondylitis clinical trials. Ann Rheum Dis 69(01):226–229
Chang JH, McCluskey PJ, Wakefield D (2005) Acute anterior uveitis and HLA-B27. Surv Ophthalmol 50(4):364–388
Lin P, Loh AR, Margolis TP, Acharya NR (2010) Cigarette smoking as a risk factor for uveitis. Ophthalmology 117(3):585–590
Zeboulon N, Dougados M, Gossec L (2008) Prevalence and characteristics of uveitis in the spondyloarthropathies: a systematic literature review. Ann Rheum Dis 67(7):955–959. https://doi.org/10.1136/ard.2007.075754
Canoui-Poitrine F, Lekpa FK, Farrenq V, Boissinot V, Hacquard-Bouder C, Comet D, Bastuji-Garin S, Thibout E, Claudepierre P (2012) Prevalence and factors associated with uveitis in spondylarthritis patients in France: results from an observational survey. Arthritis Care Res 64(6):919–924. https://doi.org/10.1002/acr.21616
Fabiani C, Vitale A, Lopalco G, Iannone F, Frediani B, Cantarini L (2016) Different roles of TNF inhibitors in acute anterior uveitis associated with ankylosing spondylitis: state of the art. Clin Rheumatol 35(11):2631–2638. https://doi.org/10.1007/s10067-016-3426-3
Frick KD, Drye LT, Kempen JH, Dunn JP, Holland GN, Latkany P, Rao NA, Sen HN, Sugar EA, Thorne JE (2012) Associations among visual acuity and vision-and health-related quality of life among patients in the multicenter uveitis steroid treatment trial. Invest Ophthalmol Vis Sci 53(3):1169–1176
Braun J, Van Den Berg R, Baraliakos X, Boehm H, Burgos-Vargas R, Collantes-Estevez E, Dagfinrud H, Dijkmans B, Dougados M, Emery P (2011) 2010 update of the ASAS/EULAR recommendations for the management of ankylosing spondylitis. Ann Rheum Dis 70(6):896–904
Escalas C, Trijau S, Dougados M (2010) Evaluation of the treatment effect of NSAIDs/TNF blockers according to different domains in ankylosing spondylitis: results of a meta-analysis. Rheumatology 49(7):1317–1325
Fiorelli VM, Bhat P, Stephen Foster C (2010) Nonsteroidal anti-inflammatory therapy and recurrent acute anterior uveitis. Ocul Immunol Inflamm 18(2):116–120
Murdaca G, Negrini S, Magnani O, Penza E, Pellecchio M, Gulli R, Mandich P, Puppo F (2018) Update upon efficacy and safety of etanercept for the treatment of spondyloarthritis and juvenile idiopathic arthritis. Mod Rheumatol 28(3):417–431
Murdaca G, Spano F, Contatore M, Guastalla A, Penza E, Magnani O, Puppo F (2015) Infection risk associated with anti-TNF-alpha agents: a review. Expert Opin Drug Saf 14(4):571–582. https://doi.org/10.1517/14740338.2015.1009036
Rudwaleit M, Rødevand E, Holck P, Vanhoof J, Kron M, Kary S, Kupper H (2009) Adalimumab effectively reduces the rate of anterior uveitis flares in patients with active ankylosing spondylitis: results of a prospective open-label study. Ann Rheum Dis 68(5):696–701
van Denderen JC, Visman IM, Nurmohamed MT, Suttorp-Schulten MS, van der Horst-Bruinsma IE (2014) Adalimumab significantly reduces the recurrence rate of anterior uveitis in patients with ankylosing spondylitis. J Rheumatol 41(9):1843–1848
Braun J, Baraliakos X, Listing J, Sieper J (2005) Decreased incidence of anterior uveitis in patients with ankylosing spondylitis treated with the anti-tumor necrosis factor agents infliximab and etanercept. Arthritis Rheumatol 52(8):2447–2451
Lim LL, Fraunfelder FW, Rosenbaum JT (2007) Do tumor necrosis factor inhibitors cause uveitis? A registry-based study. Arthritis Rheumatol 56(10):3248–3252
Lie E, Lindström U, Zverkova-Sandström T, Olsen IC, Forsblad-d'Elia H, Askling J, Kapetanovic MC, Kristensen LE, Jacobsson LT (2017) Tumour necrosis factor inhibitor treatment and occurrence of anterior uveitis in ankylosing spondylitis: results from the Swedish biologics register. Annals of the Rheumatic Diseases:annrheumdis-2016-210931
Linden SVD, Valkenburg HA, Cats A (1984) Evaluation of diagnostic criteria for ankylosing spondylitis. Arthritis Rheumatol 27(4):361–368
Dougados M, Paternotte S, Braun J, Burgos-Vargas R, Maksymowych WP, Sieper J, van der Heijde D (2011) ASAS recommendations for collecting, analysing and reporting NSAID intake in clinical trials/epidemiological studies in axial spondyloarthritis. Ann Rheum Dis 70(2):249–251
Poddubnyy D, Rudwaleit M, Haibel H, Listing J, Märker-Hermann E, Zeidler H, Braun J, Sieper J (2012) Effect of non-steroidal anti-inflammatory drugs on radiographic spinal progression in patients with axial spondyloarthritis: results from the German Spondyloarthritis Inception Cohort. Annals of the Rheumatic Diseases:annrheumdis-2011-201252
Park JW, Kwon HM, Park JK, Choi JY, Lee EB, Song YW, Lee EY (2016) Impact of dose tapering of tumor necrosis factor inhibitor on radiographic progression in ankylosing spondylitis. PLoS One 11(12):e0168958. https://doi.org/10.1371/journal.pone.0168958
Group SoUNW (2005) Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol 140(3):509–516
Benitez-Del-Castillo JM, Garcia-Sanchez J, Iradier T, Bañares A (2000) Sulfasalazine in the prevention of anterior uveitis associated with ankylosing spondylitis. Eye 14:340–343
Muñoz-Fernández S, García-Aparicio A, Hidalgo M, Platero M, Schlincker A, Bascones M, Pombo M, Morente P, Sanpedro J, Martin-Mola E (2009) Methotrexate: an option for preventing the recurrence of acute anterior uveitis. Eye 23(5):1130–1133
Muñoz-Fernández S, Hidalgo V, Fernández-Melón J, Schlincker A, Bonilla G, Ruiz-Sancho D, Fonseca A, Gijón-Baños J, Martín-Mola E (2003) Sulfasalazine reduces the number of flares of acute anterior uveitis over a one-year period. J Rheumatol 30(6):1277–1279
Raffeiner B, Ometto F, Bernardi L (2014) Inefficacy or paradoxical effect? Uveitis in ankylosing spondylitis treated with etanercept. Case Rep Med 2014:471319–471314. https://doi.org/10.1155/2014/471319
Wendling D, Joshi A, Reilly P, Jalundhwala YJ, Mittal M, Bao Y (2014) Comparing the risk of developing uveitis in patients initiating anti-tumor necrosis factor therapy for ankylosing spondylitis: an analysis of a large US claims database. Curr Med Res Opin 30(12):2515–2521
Zou J, Rudwaleit M, Brandt J, Thiel A, Braun J, Sieper J (2003) Up regulation of the production of tumour necrosis factor α and interferon γ by T cells in ankylosing spondylitis during treatment with etanercept. Ann Rheum Dis 62(6):561–564
Wendling D, Prati C (2014) Paradoxical effects of anti-TNF-α agents in inflammatory diseases. Expert Rev Clin Immunol 10(1):159–169
Khera TK, Dick AD, Nicholson LB (2010) Mechanisms of TNFalpha regulation in uveitis: focus on RNA-binding proteins. Prog Retin Eye Res 29(6):610–621. https://doi.org/10.1016/j.preteyeres.2010.08.003
Santos Lacomba M, Marcos Martin C, Gallardo Galera JM, Gomez Vidal MA, Collantes Estevez E, Ramirez Chamond R, Omar M (2001) Aqueous humor and serum tumor necrosis factor-alpha in clinical uveitis. Ophthalmic Res 33(5):251–255 doi:55677
Perez-Guijo V, Santos-Lacomba M, Sanchez-Hernandez M, Castro-Villegas Mdel C, Gallardo-Galera JM, Collantes-Estevez E (2004) Tumour necrosis factor-alpha levels in aqueous humour and serum from patients with uveitis: the involvement of HLA-B27. Curr Med Res Opin 20(2):155–157. https://doi.org/10.1185/030079903125002847
Gensler LSRJ, Lee M, Learch T, Brown M, Rahbar MH, Weisman M, Ward M (2016) High dose nonsteroidal anti-inflammatory drugs (NSAIDs) and tumor necrosis factor inhibitor use results in less radiographic progression in ankylosing spondylitis – a longitudinal analysis [abstract]. Arthritis Rheumatol 2016:68 (suppl 10)
Funding
This research was partly supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (2016R1D1A1A02937044).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
EBL has acted as a consultant to Pfizer and received research grants from Green Cross Corp. and Hanmi Pharm. The other authors declare no conflicts of interest.
Ethical standards
The study was approved by the institutional review board of the Seoul National University Hospital [IRB No. H-1607-111-777] and was conducted in accordance with the principles of the Declaration of Helsinki and Good Clinical Practice guidelines. Informed consents were waived based on the retrospective nature of the study.
Electronic supplementary material
ESM 1
(PDF 127 kb)
Rights and permissions
About this article
Cite this article
Kim, M.J., Lee, E.E., Lee, E.Y. et al. Preventive effect of tumor necrosis factor inhibitors versus nonsteroidal anti-inflammatory drugs on uveitis in patients with ankylosing spondylitis. Clin Rheumatol 37, 2763–2770 (2018). https://doi.org/10.1007/s10067-018-4249-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-018-4249-1