Abstract
Iloprost (ILO) is employed intravenously for the treatment of severe Raynaud phenomenon (RP) and digital ulcers (DU) in systemic sclerosis (SSc). The aim of this study was to evaluate the safety and tolerability of the intravenous treatment with ILO in different phases of SSc. Eighty-one consecutive non-selected SSc patients, all on nifedipine, with moderate RP, treated with ILO infusion, were retrospectively evaluated. Patients were sub classified according to the edematous or fibrotic/atrophic cutaneous phase of the disease. ILO was infused with a progressive increase of the dosage up to the achievement of patient’s tolerance, 1 day/week. In cases of slower infusion regimen due to adverse events (AE) at the beginning of the administration, patients received a lower dose of the drug (not possible to quantify precisely the final cumulative dosage). 16/81 SSc patients presented digital edema, 5 developed diarrhea, and 9 developed transient hypotension during the infusion at 20 ml/h that ameliorated when the drug was withdrawn. Moreover, 10/16 edematous patients experienced significant and painful digital swelling, unlike patients in the fibrotic group (p < 0.0001); 11/16 patients reported flushing and 7/16 headache, always controlled with dose tapering below 10 ml/h. In the atrophic/fibrotic phase patients (65/81), 10 developed diarrhea and 24 hypotension at infusion rate of 20 ml/h that led to temporary withdrawal of the drug. When ILO was restarted and kept below 10 ml/h, no side effects were experienced. 23/65 patients experienced flushing and 8/65 headache, all controlled with infusion reduction below 10 ml/h. In these patients, adverse events were significantly less frequent than in the edematous group (p = 0.023 and p = 0.008, respectively). Our data suggest that calcium channel blockers should be transitorily stopped while using ILO and that a pre-treatment approach might reduce or control adverse events. In patients with digital edema, ILO infusion should be carefully employed after the evaluation of patient’s drug tolerance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Systemic sclerosis (SSc) is a connective tissue disease characterized by vascular abnormalities, fibrosis of the skin and of internal organs, and immune system dysregulation [1]. The cutaneous involvement of the disease is characterized by different evolutive phases: generally, it starts with an edematous phase which is followed by a fibrotic and eventually atrophic phase. In these three phases, the progression of the microvascular system spans from leaky giant capillaries [2] evolving to structural aberration and loss of capillaries. These phases are characterized by edema, finger skin fibrosis, and atrophy, respectively [3]. All phases are indeed characterized by the reduction of peripheral blood perfusion (PBP) and increased incidence of digital ulcers (DU) [4]. Nowadays, several drugs are available to manage Raynaud’s phenomenon (RP) and ischemic ulcers, such as calcium channel blockers (CCB), phosphodiesterase type V (PDE V) inhibitors, prostanoids, angiotensin II receptor antagonist, angiotensin-converting enzyme inhibitor, alpha-blocker or selective serotonin reuptake inhibitor, platelet aggregation inhibitors, and endothelin-1 receptor antagonists [5,6,7,8,9,10,11,12]. A systematic review of the literature by de la García de la Peña Lefebvre et al. reported that CCB, IV iloprost (ILO), bosentan, and tadalafil show the best evidence of efficacy in treating RP attacks or DU, which supports the recommendations established by EUSTAR [11, 13].
ILO is a stable analogue of natural prostacyclin (PGI2), which inhibits platelet aggregation and adhesion, dilates arterioles and venules, activates fibrinolysis, and reduces the release of oxygen-reactive species [14]. On fibroblasts, ILO blocks the activation of connective tissue growth factor, inhibits the expression of collagen type 1 (induced by interleukin 1, TGF-α and β, IGF-1, and platelet-derived growth factor [15, 16]), and inhibits the expression of vascular cell adhesion molecule-1 and inter-cellular adhesion molecule-1 [17]. In clinics, ILO is used to manage critical leg ischemia [18] and RP [19, 20] and ischemic ulcers secondary to connective tissue diseases [21, 22].
A meta-analysis in 1998, which included the results of five RCT with intravenous iloprost, one RCT with oral iloprost, and one RCT with oral cisaprost [14, 23,24,25,26,27], including overall 332 SSc patients, indicated that ILO is effective in reducing the frequency and severity of SSc-RP [28].
Severe vascular complications represent a major cause of morbidity and mortality in SSc patients. Vascular injury involving small vessels, particularly the arterioles, occurs in virtually all organs causing tissue hypoxia and preceding fibrosis development [3]. In particular, DU are one of the most frequent and disabling SSc features, hardly affecting patients’ quality of life; the treatment of DU, usually chronic or recurrent lesions, is a major concern for the rheumatologists because of their resistance to treatment.
Nowadays, there is no standard protocol of ILO treatment for RP and DUs in systemic sclerosis. Over the years, several studies and RCT evaluated different therapeutic schemes. Wigley et al. in a multicenter, randomized, parallel placebo-controlled, double-blind study compared five daily sequential, 6-h intravenous infusions of ILO (0.5 to 2.0 ng/kg per minute) versus placebo for the treatment of RP, showing a significant reduction in DU number (35 pts. with DU at baseline) and less new DU onset in the ILO group and a significant RP improvement [14]. Rademaker et al. compared IV ILO (0.5–2 ng/kg/min 8 h on 3 consecutive days with a further single infusion at week 8) versus nifedipine [29] showing a significant decrease in the frequency, duration, and severity of RP attacks with both treatment as well as a reduction of digital lesions. Scorza et al. [20] in a RCT analyzed IV ILO (2 ng/kg/min on 5 consecutive days over a period of 8 h/day and subsequently for 8 h on 1 day every 6 weeks) versus 40 mg/day of nifedipine in 46 patients. Both drugs improved symptoms related to RP. Millio et al. in a randomized study treated 30 patients with ILO, given by intravenous infusion, at progressively increasing doses (from 0.5 to 2 ng/kg/min) over a period of 6 h each day for 10 days in 2 consecutive weeks, with repeated cycles at regular intervals of 3 months for 18 months [30]. It is clear that there is no consensus on which is the best therapeutic scheme, because in all the studies mentioned above, ILO has been effective in treatment of vascular complication in SSc.
The present study focused, in a real-life scenario, on the tolerability of ILO in the treatment of SSc patients in different phases of disease. Therefore, we analyzed the clinical histories of our case series in order to find all eventual adverse events (AE) related to ILO infusions.
Patients and methods
The clinical records of 81 consecutive non-selected SSc patients, classified according to the 2013 ACR/EULAR criteria [31], with moderate–severe RP (more than two attacks/day with moderate pain) not responsive to CCB and/or SSc-related DU, referred to two Academic Rheumatology units (the Policlinico of Modena and the “Careggi” Hospital in Florence) since 1st January 2007 to 31th May 2017 and receiving ILO infusions for a period of at least 2 years, were retrospectively evaluated. All patients received treatment from September to July, except 3 patients with severe DUs that received ILO throughout the year. Patients were sub classified in edematous or fibrotic/atrophic cutaneous phase of the disease. All patients were treated with nifedipine (20 mg/day), regardless of ILO infusions. Intravenous therapy was prepared by diluting a vial of 0.05 mg of ILO in 250 ml of 0.9% saline solution (200 ng/ml). ILO schedule consisted in 1 day per week IV infusion with a schedule of 6–8-h infusion with a progressive increase of the dosage up to the achievement of patient’s tolerance (dose ranging from 0.5 to 1.5 ng/kg/min). The pump infusion was started at 5 ml/h (1000 ng/h corresponding to 16 ng/min) and increased every half an hour up to a maximum of 20 ml/h (4000 ng/h which corresponds to 67 ng/min) according to patient tolerance and appearance of side effects, with a progressive increase of the dosage up to the achievement of patient’s tolerance, 1 day/week (average cumulative dose 24 μg for each session of 6 h). In cases of slower infusion regimen (0.5 ng/kg/min) due to AE at the beginning of the administration, patients received a lower dose of the drug (not possible to quantify precisely the final cumulative dosage). No pre-treatment regimen, in particular, no antiemetic treatment was employed in all patients.
To evaluate the safety and tolerability of infusion therapy with ILO, the infusion rate (ng/kg/min) and the occurrence of any AE during the infusion or in the following hours after treatment were recorded.
The number and characteristic of AE event were recorded and classified according to severity and frequency, thus requiring dose reduction, temporary suspension, or drug discontinuation. The retrospective study was approved by the Ethical Committee (protocol n. 282/15). All patients gave their written consent.
Statistical analysis
Data were presented as mean ± standard deviation (SD), or median (range) for non-normalized data series. Comparisons were made using the chi-square test (with Fisher’s exact test where applicable) and the p values less than 0.05 were considered statistically significant.
Results
SSc patients’ features at baseline were the following: males:females, 5:76; mean age at SSc diagnosis, 45.56 ± 7.57 years; median disease duration at the beginning of therapy, 8 years (range 2–12); diffuse cutaneous subset of SSc in 47/81 (58%) patients while limited subset cutaneous in 34/81 (42%); anti-Scl70 and anticentromere autoantibodies were present in 45/81 (55%) and 32/81 (39%) patients, respectively. Fifty-five (68%) patients had active or history of DU while 10 (12%) patients had calcinosis at the beginning of ILO treatment (Table 1).
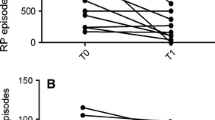
Sixteen patients (19.8%) were in the edematous phase with puffy fingers (digital edema) [males:females, 2:14; mean age at SSc diagnosis, 46 ± 7.84 years; median disease duration at the beginning of therapy, 3.75 years (2–5)]. In this subgroup, 5 patients (31.2%) developed diarrhea and 9 (56.2%) transient hypotension (systolic pressure below 90 mmHg) during the infusion at 20 ml/h. When the drug was withdrawn, patients had an immediate amelioration, but when ILO at an infusion rate below 10 ml/h was restarted, diarrhea or hypotension again developed, thus leading to definitive interruption of the treatment. Moreover, 10/16 patients (62.5%) experienced significant and painful digital swelling which led to the tapering of the infusion dosage below 10 ml/h (the dose thus tapered to 0.5 ng/kg/min) (not possible to quantify precisely the final cumulative dosage). Out of these 10 patients, only 1 could continue the treatment while the other 9 had to be definitively withdrawn because of intense digital pain due to intense vasodilation. Finally, 11 patients (68.7%) reported flushing and 7 (43.7%) headache, but they were always controlled with the reduction of the infusion below 10 ml/h.
Sixty-five patients (80.3%) were in the fibrotic/atrophic cutaneous phase [males:females, 3:62; mean age at SSc diagnosis, 45.45 ± 7.49 years; median disease duration at the beginning of therapy, 8 years (5–12)]. During the infusion at infusion rate of 20 ml/h (0.5–1.5 ng/kg/min), 10 patients (15.3%) developed diarrhea and 24 patients (37%) hypotension, leading to temporary withdrawal. When ILO was restarted and kept below 10 ml /h, no AE were experienced.
Flushing in 23 cases (35.4%) and headache in 8 cases (12.3%) were experienced but were controlled with infusion rate reduction below 10 ml/h; moreover, these AE were significantly less frequent than in the patients belonging to the edematous group (p = 0.023 and p = 0.008, respectively) (Table 2).
Almost 60% of patients received 6-h infusion because it was better tolerated compared to 8 h. However, it is noteworthy that 40% of the patients had a longer administration period of 8 h: these patients received a lower dose of the drug for a longer period due to AE registered at the beginning of the administration. For this reason, the rate of administration was never increased and remained at a lower level.
Finally, also episodes of agitation, tachycardia, and extrasystoles were experienced but were immediately controlled with the described dose tapering. No severe side effects were noticed.
Discussion
Several studies showed the efficacy of ILO in the treatment of vascular manifestations of SSc, namely RP and DU [24, 32, 33]. The data obtained from this retrospective study show that the safety and tolerability of ILO, a powerful, chemically stable prostacyclin I2 analogue, are satisfactory, confirming results of our previous study [34]. Our results have been obtained on a small number of patients; however, the data may indicate that the drug should be carefully employed in these patients to limit the digital pain due to abrupt swelling. Overall, the flow chart summarizes mainly the approach to the rate and length of the infusion, while the repetition remains to be decided by the physician (Fig. 1).
In our patients, the most important side effects were flushing, headache, and digital pain due to worsening of edema, in particular in patients with puffy fingers. Surprisingly, tolerability is much better in the fibrotic and atrophic phases of the disease than in the edematous phase, even if the last one is the phase that presents the least vascular involvement. During ILO infusion, pain due to worsening of digital edema suggests a careful approach to patients in the early phase of disease. Likely, the concomitant treatment with nifedipine (20 mg/day) could have contributed to the vasodilating effect, thus fostering the worsening of the edema. Episodes of diarrhea during ILO infusion were more frequent in edematous and fibrotic patients with gastrointestinal involvement, i.e., with symptomatic or subclinical abnormalities at anorectal manometry (was not investigated in this study) since the early phase of disease [35].
Other side effects like agitation, tachycardia, arrhythmia, and extrasystoles were also observed but were easily controlled with dose tapering.
In the literature, some reports have suggested the potential risk of developing ischemic cardiovascular complications (myocardial infarction or stroke). These events were reported in patients that presented a higher cardiovascular risk (14%) in respect to those without cardiovascular risk (2.4%) [36]. The potential ischemic cardiac risk has been linked to a “stealing” vascular event, which in an extramural coronary atherosclerosis could foster a myocardial ischemia. Therefore, this evidence suggests that ILO may have a crucial role in ischemic cardiovascular complications in patients at high cardiovascular risk. Therefore, the cardiovascular risk should be always investigated in SSc to carefully identify patients at high risk for ischemic cardiac events [37,38,39].
In our previous study [34], no patient had diarrhea or vomiting during ILO infusion; however, all subjects received premedication with ondansetron. This may highlight that the control of the dose and the rate of infusion would not be the unique method in order to limit ILO side effects.
Initially, in our cases, we used ILO at dose of 0.5–1.5 ng/kg/min (average cumulative dose 24 μg for each session of 6 h), according to pharmaceutical recommendations [40]. However, the relative high frequency of AE led us to reduce ILO infusion rate and, consequently, the total dosage of ILO administered; indeed, ILO infusion level of average 10 ml/h (0.5 ng/kg/min) guaranteed the spontaneous resolution of the large majority of the AE reported.
A randomized, open-label trial including 50 patients with SSc has evaluated the effects of low doses of iloprost (0.5 ng/kg/min for 6 h/day) compared to high doses of ILO (0.5 ng/kg/min increased to a maximum of 2.0 ng/kg/min for 6 h/day) [40]. Both doses, reported average reduction in the frequency and duration of attacks of RP after 21 days of therapy, and significant DU healing have been reported, although the sample size was small, and some patients showed no effect of treatment.
Caramaschi P et al. described that ILO infusion once a month at the mean dosage of 0.94 ± 0.26 ng/kg/min for 6 h/day was effective on DU prevention and healing, without major side effects [39]. Consistently, in our previous study, the administration of mean ILO dose of 0.8–1 ng/kg/min resulted in a well-tolerated therapy, without losing clinical efficacy [34].
Other studies have tried a discontinuation regimen to reduce the number of side effects with poor clinical results that did not suggest its use [33].
Recently, the combination of ILO and bosentan has been reported to be efficient in preventing the recurrence of digital ulcers without experiencing major AE that led to the interruption of drug administration. In one study, ILO was employed with 0.5–2 ng/kg/min for the duration of 6 h every 4 weeks for 6 months [33] or average 80 μg/day, for 5 continuous days, every 3 months for 2 years [41]. This combination has been shown also to contribute to the partial recovery of the microvasculature without inducing any major side effects [42, 43]. The literature has shown that ILO is effective in treating vascular ischemic disease in SSc-related RP [40, 44]. Several pharmacological effects, e.g., vasodilation, platelet inhibition, blockade of leukocyte migration, reduction of the expression of adhesion molecules, and fibrinolysis, explain ILO efficacy in SSc. Furthermore, the immunoregulatory properties of ILO could contribute to attenuate inflammation [44]. Our experience shows for the first time that the physician may assess patient tolerability and consequently modulate the drug dosage. This can be helpful in a real-life setting because it spares the patient from overlapping further AE, thus allowing to continue the treatment and avoiding withdrawal.
In fact, our data suggest that the ILO dose must be tailored in accordance with the patient’s individual tolerability. Therefore, considering our experience and the results of previous randomized and observational clinical studies, the therapeutic regimen shown in Fig. 1 may be proposed. Treatment with ILO should be modulated according to the patient’s symptoms, with increasing doses consistently with the severity of the clinical picture.
In our retrospective study, the safety and tolerability of ILO on a small number of patients were evaluated before designing a large-scale randomized trial. The data demonstrate that ILO was well tolerated in fibrotic or atrophic SSc patients, where side effects could be well managed by reducing/modulating the infusion rate. Conversely, in edematous SSc patients, ILO infusion should be always carefully employed because of the occurrence of diarrhea and digital pain and swelling. Our data suggest that the therapy with nifedipine should be transitorily stopped when ILO is used. Moreover, a pre-treatment approach may help in reducing or better controlling AE. Therefore, the therapeutic advantages expected on SSc features should be evaluated after consideration of the single patient’s ILO tolerance and the problem of using nifedipine in combination during the treatment carefully evaluated.
In our work, the weekly ILO administration, the 8-h infusion, the HCQ treatment without a premedication with ondansetron, the parallel use of CCB, and the heterogeneous population can be considered as limiting factors. Moreover, also the retrospective and descriptive design of the work can be considered as a limitation. However, our data provide useful information on safety of IV ILO in a “real-life scenario” reporting what is observed in clinical practice. In fact, the lack of adjusting for potential confounders may be seen as factors limiting the significance of the data. It should be also noted that the edematous patients were not very numerous compared to those in the fibrotic phase. Despite this, it was interesting to observe that these patients presented a worsening of their quality of life due to the increase of digital pain and edema as well as diarrhea.
Conclusions
In the fibrotic/atrophic phase of SSc, ILO was well tolerated and side effects were managed by reducing/modulating the infusion rate. In edematous patients, side effects were more frequent and led to drug withdrawal, mostly because of painful digital swelling and diarrhea. Our data suggest that calcium channel blockers should be transitorily stopped while using ILO and that a pre-treatment approach might reduce or control adverse events. In patients with digital edema, ILO infusion should be carefully employed after the evaluation of patient’s drug tolerance. New studies with a larger sample size might be important to broaden the data analysis in order to confirm the present data.
References
Matucci-Cerinic M, Kahaleh B, Wigley FM (2013) Evidence that systemic sclerosis is a vascular disease. Arthritis Rheum 65:1953–1962
Frech TM, Revelo MP, Drakos SG, Murtaugh MA, Markewitz BA, Sawitzke AD et al (2012) Vascular leak is a central feature in the pathogenesis of systemic sclerosis. J Rheumatol 39:1385–1391
Matucci-Cerinic M, Manetti M, Bruni C, Chora I, Bellando Randone S, Lepri G et al (2017) The “myth” of loss of angiogenesis in systemic sclerosis: a pivotal early pathogenetic process or just a late unavoidable event? Arthritis Res Ther 6(19):162
Rabquer BJ, Koch AE (2012) Angiogenesis and vasculopathy in systemic sclerosis: evolving concepts. Curr Rheumatol Rep 14:56–63
Ennis H, Hughes M, Anderson ME, Wilkinson J, Herrick A (2016) Calcium channel blockers for primary Raynaud’s phenomenon. Cochrane Database Syst Rev 2:CD002069
Herrick AL, van den Hoogen F, Gabrielli A, Tamimi N, Reid C, O'Connell D, Vázquez-Abad MD, Denton CP (2011) Modified-release sildenafil reduces Raynaud’s phenomenon attack frequency in limited cutaneous systemic sclerosis. Arthritis Rheum 63:775–782
Thompson AE, Shea B, Welch V, Fenlon D, Pope JE (2001) Calcium-channel blockers for Raynaud’s phenomenon in systemic sclerosis. Arthritis Rheum 44:1841–1847
Hettema ME, Zhang D, Bootsma H, Kallenberg CGM (2007) Bosentan therapy for patients with severe Raynaud’s phenomenon in systemic sclerosis. Ann Rheum Dis 66:1398–1399
Matucci-Cerinic M, Denton CP, Furst DE, Mayes MD, Hsu VM, Carpentier P, Wigley FM, Black CM, Fessler BJ, Merkel PA, Pope JE, Sweiss NJ, Doyle MK, Hellmich B, Medsger TA, Morganti A, Kramer F, Korn JH, Seibold JR (2011) Bosentan treatment of digital ulcers related to systemic sclerosis: results from the RAPIDS-2 randomised, double-blind, placebo-controlled trial. Ann Rheum Dis 70:32–38
Della Rossa A, Doveri M, D’Ascanio A, Tavoni A, Consensi A, Neri R et al (2011) Oral sildenafil in skin ulcers secondary to systemic sclerosis. Scand J Rheumatol 40:323–325
Kowal-Bielecka O, Landewé R, Avouac J, Chwiesko S, Miniati I, Czirjal L et al (2009) EULAR recommendations for the treatment of systemic sclerosis: a report from the EULAR Scleroderma Trials and Research group (EUSTAR). Ann Rheum Dis 68:620–628
Wise RA, Wigley FM, White B, Leatherman G, Zhong J, Krasa H, Kambayashi J, Orlandi C, Czerwiec FS (2004) Efficacy and tolerability of a selective alpha(2C)-adrenergic receptor blocker in recovery from cold-induced vasospasm in scleroderma patients: a single-center, double-blind, placebo-controlled, randomized crossover study. Arthritis Rheum 50:3994–4001
García de la Peña Lefebvre P, Nishishinya MB, Pereda CA, Loza E, Sifuentes Giraldo WA, Román Ivorra JA, Carreira P, Rúa-Figueroa I, Pego-Reigosa JM, Muñoz-Fernández S (2015) Efficacy of Raynaud’s phenomenon and digital ulcer pharmacological treatment in systemic sclerosis patients: a systematic literature review. Rheumatol Int 35:1447–1459
Wigley FM, Wise RA, Seibold JR, McCloskey DA, Kujala G, Medsger TA et al (1994) Intravenous iloprost infusion in patients with Raynaud phenomenon secondary to systemic sclerosis. A multicenter, placebo-controlled, double-blind study. Ann Intern Med 120:199–206
Stratton R, Rajkumar V, Ponticos M, Nichols B, Shiwen X, Black CM et al (2002) Prostacyclin derivatives prevent the fibrotic response to TGF-beta by inhibiting the Ras/MEK/ERK pathway. FASEB J 16:1949–1951
Stratton R, Shiwen X, Martini G, Holmes A, Leask A, Haberberger T et al (2001) Iloprost suppresses connective tissue growth factor production in fibroblasts and in the skin of scleroderma patients. J Clin Invest 2001(108):241–250
Lindemann S, Gierer C, Darius H (2003) Prostacyclin inhibits adhesion of polymorphonuclear leukocytes to human vascular endothelial cells due to adhesion molecule independent regulatory mechanisms. Basic Res Cardiol 98(1):8–15
Fiessinger JN, Schäfer M (1990) Trial of iloprost versus aspirin treatment for critical limb ischemia for thromboangiitis obliterans. Lancet 335:555–557
Wigley FM, Seibold JR, Wise RA, McCloskey DA, Dole WP (1992) Intravenous iloprost treatment of Raynaud’s phenomenon and ischemic ulcers secondary to systemic sclerosis. J Rheumatol 19:1407–1414
Scorza R, Caronni M, Mascagni B, Berruti V, Bazzi S, Micallef E, Arpaia G, Sardina M, Origgi L, Vanoli M (2001) Effects of long-term cyclic iloprost therapy in systemic sclerosis with Raynaud’s phenomenon. A randomized, controlled study. Clin Exp Rheumatol 19:503–508
Veale DJ, Muir AH, Morley KD, Belch JJF (1995) Treatment of vasculitic leg ulcers in connective tissue disease with iloprost. Clin Rheumatol 14:187–191
Zahavi J, Charach G, Schafer R, Toeg A, Zahavi M (1993) Ischaemic necrotic toes associated with antiphospholipid syndrome and treated with iloprost. Lancet 342:862
Belch JJ, Capell HA, Cooke ED, Kirby JD, Lau CS, Madhok R, Murphy E, Steinberg M (1995) Oral iloprost as a treatment for Raynaud’s syndrome: a double blind multicentre placebo controlled study. Ann Rheum Dis 54:197–200
Kyle MV, Belcher G, Hazleman BL (1992) Placebo controlled study showing therapeutic benefit of iloprost in the treatment of Raynaud’s phenomenon. J Rheumatol 19:1403–1406
Lau CS, Belch JJ, Madhok R, Cappell H, Herrick A, Jayson M, Thompson JM (1993) A randomised, double-blind study of cicaprost, an oral prostacyclin analogue, in the treatment of Raynaud’s phenomenon secondary to systemic sclerosis. Clin Exp Rheumatol 11:35–40
McHugh NJ, Csuka M, Watson H, Belcher G, Amadi A, Ring EF et al (1988) Infusion of iloprost, a prostacyclin analogue, for treatment of Raynaud’s phenomenon in systemic sclerosis. Ann Rheum Dis 47:43–47
Yardumian DA, Isenberg DA, Rustin M, Belcher G, Snaith ML, Dowd PM et al (1988) Successful treatment of Raynaud’s syndrome with iloprost, a chemically stable prostacyclin analogue. Br J Rheumatol 27:220–226
Pope J, Fenlon D, Thompson A, Shea B, Furst D, Wells G et al (2000) Iloprost and cisaprost for Raynaud’s phenomenon in progressive systemic sclerosis. Cochrane Database Syst Rev. 2:CD000953
Rademaker M, Cooke ED, Almond NE, Beacham JA, Smith RE, Mant TG, Kirby JD (1989) Comparison of intravenous infusion of iloprost and oral nifedipine in treatment of Raynaud’s phenomenon in patients with systemic sclerosis: a double blind randomised study. Br Med J 298:561–564
Milio G, Corrado E, Genova C, Amato C, Raimondi F, Almasio PL, Novo S (2006) Iloprost treatment in patients with Raynaud’s phenomenon secondary to systemic sclerosis and the quality of life: a new therapeutic protocol. Rheumatology 45:999–1004
Van den Hoogen F, Khanna D, Fransen J, Johnson SR, Baron M, Tyndall A et al (2013) 2013 classification criteria for systemic sclerosis: an American College of Rheumatology/European League against Rheumatism collaborative initiative. Arthritis Rheum 65:2737–2747
Bettoni L, Geri A, Airò P, Danieli E, Cavazzana I, Antonioli C, Chiesa L, Franceschini F, Grottolo A, Zambruni A, Radaeli E, Cattaneo R (2002) Systemic sclerosis therapy with iloprost: a prospective observational study of 30 patients treated for a median of 3 years. Clin Rheumatol 21:244–250
Bali G, Schwantzer G, Aberer F, Kraenke B, Aberer E (2011) Discontinuing long-term iloprost treatment for Raynaud’s phenomenon and systemic sclerosis: a single-center, randomized, placebo-controlled, double-blind study. Acta Dermatovenerol Alp Pannonica Adriat 20:13–21
Colaci M, Lumetti F, Giuggioli D, Guiducci S, Bellando-Randone S, Fiori G et al (2017) Long-term treatment of scleroderma-related digital ulcers with iloprost: a cohort study. Clin Exp Rheumatol 106:179–183
Lepri G, Bellando-Randone S, Guiducci S, Giani I, Bruni C, Blagojevic J et al (2015) Esophageal and anorectal involvement in patients with very early diagnosis of systemic sclerosis (VEDOSS): report from a single EUSTAR centre. Ann Rheum Dis 74:124–128
Colaci M, Sebastiani M, Giuggioli D, Manfredi A, Rossi R, Modena MG, Ferri C (2008) Cardiovascular risk and prostanoids in systemic sclerosis. Clin Exp Rheumatol 26(2):333–336
Arreghini M, Prudente P, Maglione W, Arnoldi C, Tosi S, Marchesoni A (2001) Tolerability, safety and efficacy of iloprost infusion without peristaltic pump in systemic sclerosis. Reumatismo 53:140–144
Torley HI, Madhok R, Capell HA, Brouwer RM, Maddison PJ, Black CM, Englert H, Dormandy JA, Watson HR (1991) A double blind, randomised, multicentre comparison of two doses of intravenous iloprost in the treatment of Raynaud’s phenomenon secondary to connective tissue diseases. Ann Rheum Dis 50:800–804
Caramaschi P, Martinelli N, Volpe A, Pieropan S, Tinazzi I, Patuzzo G, Mahamid H, Bambara LM, Biasi D (2009) A score of risk factors associated with ischemic digital ulcers in patients affected by systemic sclerosis treated with iloprost. Clin Rheumatol 28:807–813
Kawald A, Burmester GR, Huscher D, Sunderkötter C, Riemekasten G (2008) Low versus high-dose iloprost therapy over 21 days in patients with secondary Raynaud’s phenomenon and systemic sclerosis: a randomized, open, single-center study. J Rheumatol 35:1830–1837
De Cata A, Inglese M, Molinaro F, De Cosmo S, Rubino R, Bernal M et al (2016) Digital ulcers in scleroderma patients: a retrospective observational study. Int J Immunopathol Pharmacol 29:180–187
Cutolo M, Ruaro B, Pizzorni C, Ravera F, Smith V, Zampogna G, Paolino S, Seriolo B, Cimmino M, Sulli A (2014) Longterm treatment with endothelin receptor antagonist bosentan and iloprost improves fingertip blood perfusion in systemic sclerosis. J Rheumatol 41:881–886
Cestelli V, Manfredi A, Sebastiani M, Praino E, Cannarile F, Giuggioli D, Ferri C (2017) Effect of treatment with iloprost with or without bosentan on nailfold videocapillaroscopic alterations in patients with systemic sclerosis. Mod Rheumatol 27(1):110–114
D’Amelio P, Cristofaro MA, D’Amico L, Veneziano L, Roato L, Sassi F (2010) Iloprost modulates the immune response in systemic sclerosis. BMC Immunol 11:62–68
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The retrospective study was approved by the Ethical Committee (protocol n. 282/15). All patients gave their written consent.
Disclosures
None.
Rights and permissions
About this article
Cite this article
Bellando-Randone, S., Bruni, C., Lepri, G. et al. The safety of iloprost in systemic sclerosis in a real-life experience. Clin Rheumatol 37, 1249–1255 (2018). https://doi.org/10.1007/s10067-018-4043-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-018-4043-0