Abstract
The purpose of this study is to investigate the clinical and serological associations of anti-ribosomal P0 protein antibodies (anti-Rib-P0) in patients with systemic lupus erythematosus (SLE). The sera of 470 patients with SLE and 124 patients with primary Sjogren’s Syndrome (pSS) were collected. Line immunoassay (LIA) was used to detect anti-Rib-P0 and other related antibodies. A complete laboratory evaluation and clinical examination were also performed in each SLE patient. The prevalence of anti-Rib-P0 in SLE patients was significantly higher than that in pSS patients (35.74 vs 6.45%) (P < 0.001). There was a significantly lower prevalence of cardiac involvement in anti-Rib-P0-positive SLE patients compared to anti-Rib-P0-negative SLE patients (P = 0.019); no significant associations of anti-Rib-P0 antibodies with encephalopathy manifestations and other vital organs involvement were observed. Anti-nucleosomes, anti-dsDNA, anti-Histones, anti-SmD1, and anti-U1snRNP were significantly associated with serum anti-Rib-P0 antibodies positivity in SLE patients (all P < 0.05). The sensitivity and specificity of the anti-Rib-P0 antibodies to diagnose SLE were 35.74 and 93.55%, respectively. There is a higher prevalence of anti-Rib-P0 in SLE patients. Anti-Rib-P0 positivity may indicate lower cardiac involvement for SLE patients. It may serve as an important complementary parameter in SLE, in addition to anti-dsDNA, anti-SmD1, and anti-nucleosomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Systemic lupus erythematosus (SLE) is a chronic inflammatory and autoimmune disease characterized by the presence of autoantibodies directed against a variety of nuclear and cytoplasmic antigens. It cannot only affect multiple organs, but also has a large spectrum of clinical presentations. Assessment of the autoantibody profile is fundamental and important process in the diagnosis, pathogenesis, and clinical management of SLE [1].
The targets of anti-ribosomal antibodies are three highly conserved P proteins located on the 60S subunit of ribosomes [2, 3]. These three ribosomal proteins (P0, P1, P2) are organized in a pentamer consisting of one copy of P0 and two copies each of P1 and P2, with the molecular weights of 38, 19, and 17 kD. The immunodominant epitope of SLE patients is a shared sequence at the carboxy (C)-termini of the P proteins [4,5,6]. Autoantibody directed against three phosphorylated protein (P proteins) components of ribosomes is present in the sera of SLE patients and is highly specific for this disease. The reported prevalence of anti-ribosomal P protein antibodies (anti-Rib-P) in SLE population ranges from 6 to 46%, which is higher in Asian patients than Afro-Americans and Caucasians [7,8,9,10,11,12]. Anti-ribosomal P0 protein antibody (anti-Rib-P0) is one of the three subunits of anti-Rib-P; several previous studies have addressed the diagnostic value of anti-Rib-P0; sera anti-Rib-P0 is highly specific for SLE, therefore having a significant clinical value in the diagnosis of SLE [13, 14]. However, comprehensive analyses on the clinical associations of anti-Rib-P0 which mediate SLE-related organ injuries in the Chinese population remain largely unknown.
The aim of our study is to evaluate the clinical and serological associations of anti-Rib-P0 in a large cohort of Chinese SLE patients and clarify the correlation of anti-Rib-P0 with vital organs damage in SLE.
Materials and methods
Study subjects
This study is approved by the ethical committees in the First Affiliated Hospital of Bengbu Medical College. Methods were carried out in accordance with the approved guidelines. All subjects were enrolled after informed consent had been obtained. Four hundred and seventy patients with SLE (441 females, 29 males; mean age 35.63 ± 13.23 years, range from 14 to 70 years) were recruited from the Department of Rheumatology and Immunology at the First Affiliated Hospital of Bengbu Medical College from 2013 to 2015. All patients fulfilled the American College of Rheumatology (ACR) criteria for SLE [15]; drug-induced SLE patients were excluded. From the same hospital, 124 patients with primary Sjögren’s syndrome (pSS) (121 females, 3 males; mean age 46.44 ± 12.65 years, range from 20 to 81 years) who fulfilled the preliminary European League Against Rheumatism Criteria of Vitali et al. [16] were chosen as controls. Clinical features were defined according to the ACR criteria [15], encephalopathy was diagnosed according to the ACR guidelines [17]. Cardiac involvement involves the pericardium, valves, myocardium, and coronary arteries. Interstitial lung disease was diagnosed by CT scan. Demographic data, clinical data, and laboratory data were collected from hospital records or by self-designed questionnaire and reviewed by experienced physicians.
Extraction of serum and measurement of autoantibodies
Blood samples were obtained from 5 ml of whole blood of all enrolled SLE and pSS patients and then stored at − 20 °C until analysis. The anti-Rib-P0 and other antibodies (anti-nucleosomes, anti-dsDNA, anti-Histones, anti-SmD1, anti-U1snRNP, anti-SSA/Ro60, anti-SSA/Ro52, anti-SSb/La, anti-Scl70, anti-Centromere and anti-Jo1) were determined by line immunoassay (LIA). Reagents were purchased from Human Gesellschaft fur Biochemica und Diagnostica mbH, Wiesbaden, Germany. The detection was performed according to the manufacturers’ instructions.
Statistical analysis
All results were presented as mean ± SD or median (interquartile range, IQR) if they were not in normal distribution. The Student’s t test was used for comparison of ECLAM score indices, expressed as mean ± SD. Clinical and serological parameters were analyzed using conventional chi-square test or Fisher’s exact test. Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) statistical software for Windows, version 10.01 (SPSS Inc., IL, USA). All results were considered significant at the 0.05 level.
Results
The general features of study subjects are shown in Table 1. We examined two groups of subjects: 470 SLE patients and 124 pSS controls. Their mean age (± SD) was 35.63 ± 13.23 and 46.44 ± 12.65 years, respectively. Females accounted for 94% of the SLE group and 98% of the pSS controls. The disease duration of SLE and pSS was (4.01 ± 4.62) years and (4.07 ± 4.93 years), respectively. The prevalence of nephritis, encephalopathy, cardiac involvement, and gastrointestinal vasculitis in SLE patients was significantly higher than that in pSS patients (all P < 0.05). The prevalence of anti-Rib-P0 in SLE patients was significantly higher than that in pSS patients (35.74 vs 6.45%) (P < 0.05).
The comparison of the clinical findings between the antibody-positive and antibody-negative groups demonstrated a much lower prevalence of cardiac involvement in anti-Rib-P0-positive patients (P = 0.019). No significant differences in the prevalence of other vital organ damages were observed between the anti-Rib-P0-positive and anti-Rib-P0-negative SLE patients (Table 2).
Associations of anti-Rib-P0 antibodies with categorical laboratory parameters of SLE patients were also analyzed, and the results showed that anti-Rib-P0 antibodies were associated with anti-nucleosomes, anti-dsDNA, anti-Histones, anti-SmD1, and anti-U1snRNP (Table 3).
The sensitivity and specificity of the anti-Rib-P0 antibodies to diagnose SLE were 35.74 and 93.55%, respectively. The seroprevalence of antibodies and clinical accuracy was shown in Table 4.
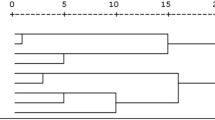
Anti-nucleosomes, anti-dsDNA, anti-Histones, anti-SmD1, and anti-Rib-P0 showed a higher seroprevalence and area under the curve (AUC) than the combination diagnostic of these five antibodies (Table 5).
Discussion
SLE is a chronic, multifaceted rheumatic disease characterized by the generation of autoantibodies predominantly directed against nuclear proteins and nucleic acids. Anti-Rib-P antibodies are serological markers for SLE described in 13–20% of patients; it might contribute to the cognitive impairment which is frequently observed in SLE patients [18].
An original and important finding of this study was that the prevalence of anti-Rib-P0 in SLE patients was significantly higher than in pSS controls. The sensitivity and specificity of the anti-Rib-P0 antibodies to diagnose SLE were 35.74 and 93.55%, respectively. In addition, anti-Rib-P0 antibodies were also found in the serum of patients with pSS; this is inconsistent with previous studies on the specificity of anti-Rib-P0 in SLE. The possible explanation is that some of pSS patients would fold to SLE after years of slow progression; therefore, the presence of anti-Rib-P0 in pSS may predict the possibility of future concurrent SLE.
There was a much lower prevalence of cardiac involvement in anti-Rib-P0 positive SLE patients compared to anti-Rib-P0 negative SLE patients, but those vital complications of SLE such as nephritis and encephalopathy were not associated with anti-Rib-P0 positivity. In addition, there was no significant correlation between neural symptoms and anti-Rib-P0; this result is consistent with previous studies [19, 20].
Giving the evidence for an association of anti-Rib-P0 with other specific autoantibodies for SLE, the frequency of anti-nucleosomes, anti-dsDNA, anti-Histones, anti-SmD1, and anti-U1snRNP were higher in anti-Rib-P0 positive patients than those of negative patients. However, we found no significant correlation of anti-Rib-P0 with anti-SSA/Ro60, anti-SSA/Ro52, anti-SSb/La, anti-Scl70, anti-Centromere, and anti-Jo1, respectively.
As the prevalence of anti-Rib-P0 antibodies in SLE varies according to several factors, of which the most important factor is the method for antibody detection/measurement, we investigated the anti-Rib-P0 antibodies by using LIA; the prevalence of anti-Rib-P0 antibodies in SLE patients was 35.7%. Previous studies showed that the prevalence of anti-Rib-P0 in a Chinese SLE cohort and a Caucasian SLE cohort was 33 and 22% by means of enzyme-linked immunosorbent assays (ELISA), respectively [19, 20].
Some limitations should be considered in the current study. First, the cardiac involvements in SLE patients are broad, it contains pericarditis, endocarditis, myocarditis, coronary vasculitis and other cardiac diseases, but in this study, it has pericarditis that had been reported only; any other cardiac involvements (endocarditis, myocarditis, and coronary vasculitis) of SLE patients were not recorded. Second, the measurement for anti-Rib-P0 is by LIA, which is a qualitative but not a quantitative determination method. Therefore, the value of anti-Rib-P0 and its association with clinical characteristics cannot be fully analyzed. Furthermore, this study is a retrospective study, we have no detailed clinical data of patients with positive anti-Rib-P0 only; thus we could not compare the differences of clinical characteristics between having positive anti-Rib-P0 patients and those having negative anti-Rib-P0 patients.
Nevertheless, the present study also has its advantages: the study included a large Chinese population including 470 SLE patients and 124 pSS patients; the evaluation of these antibodies was by a method commonly used in clinical practice with high sensitivity and specificity.
Conclusion
In conclusion, our results indicate the potential usefulness of anti-Rib-P0 as a specific marker in SLE patients. In addition, anti-Rib-P0 positivity may indicate lower cardiac involvement for SLE patients.
References
Viana VT, Durcan L, Bonfa E, Elkon KB (2017) Ribosomal P antibody: 30 years on the road. Lupus 26(5):453–462. https://doi.org/10.1177/0961203317690243
Elkon KB, Parnassa AP, Foster CL (1985) Lupus autoantibodies target ribosomal P proteins. J Exp Med 162(2):459–471
Francoeur AM, Peebles CL, Heckman KJ, Lee JC, Tan EM (1985) Identification of ribosomal protein autoantigens. J Immunol 135(4):2378–2384
Mahler M, Kessenbrock K, Raats J, Williams R, Fritzler MJ, Bluthner M (2003) Characterization of the human autoimmune response to the major C-terminal epitope of the ribosomal P proteins. J Mol Med (Berl) 81(3):194–204. https://doi.org/10.1007/s00109-003-0423-1
Elkon K, Skelly S, Parnassa A, Moller W, Danho W, Weissbach H, Brot N (1986) Identification and chemical synthesis of a ribosomal protein antigenic determinant in systemic lupus erythematosus. Proc Natl Acad Sci U S A 83(19):7419–7423
Hasler P, Brot N, Weissbach H, Danho W, Blount Y, Zhou JL, Elkon KB (1994) The effect of phosphorylation and site-specific mutations in the immunodominant epitope of the human ribosomal P proteins. Clin Immunol Immunopathol 72(2):273–279
Sato T, Uchiumi T, Ozawa T, Kikuchi M, Nakano M, Kominami R, Arakawa M (1991) Autoantibodies against ribosomal proteins found with high frequency in patients with systemic lupus erythematosus with active disease. J Rheumatol 18(11):1681–1684
Nojima Y, Minota S, Yamada A, Takaku F, Aotsuka S, Yokohari R (1992) Correlation of antibodies to ribosomal P protein with psychosis in patients with systemic lupus erythematosus. Ann Rheum Dis 51(9):1053–1055
Arnett FC, Reveille JD, Moutsopoulos HM, Georgescu L, Elkon KB (1996) Ribosomal P autoantibodies in systemic lupus erythematosus. Frequencies in different ethnic groups and clinical and immunogenetic associations. Arthritis Rheum 39(11):1833–1839
Mahler M, Kessenbrock K, Szmyrka M, Takasaki Y, Garcia-De La Torre I, Shoenfeld Y, Hiepe F, Shun-le C, von Muhlen CA, Locht H, Hopfl P, Wiik A, Reeves W, Fritzler MJ (2006) International multicenter evaluation of autoantibodies to ribosomal P proteins. Clin Vaccine Immunol 13(1):77–83. https://doi.org/10.1128/CVI.13.1.77-83.2006
Teh LS, Lee MK, Wang F, Manivasagar M, Charles PJ, Nicholson GD, Hay EM, Isenberg DA, Amos N, Williams BD (1993) Antiribosomal P protein antibodies in different populations of patients with systemic lupus erythematosus. Br J Rheumatol 32(8):663–665
Haddouk S, Marzouk S, Jallouli M, Fourati H, Frigui M, Hmida YB, Koubaa F, Sellami W, Baklouti S, Hachicha J, Bahloul Z, Masmoudi H (2009) Clinical and diagnostic value of ribosomal P autoantibodies in systemic lupus erythematosus. Rheumatology (Oxford) 48(8):953–957. https://doi.org/10.1093/rheumatology/kep142
Shi ZR, Cao CX, Tan GZ, Wang L (2015) The association of serum anti-ribosomal P antibody with clinical and serological disorders in systemic lupus erythematosus: a systematic review and meta-analysis. Lupus 24(6):588–596. https://doi.org/10.1177/0961203314560003
Valoes CC, Molinari BC, Pitta AC, Gormezano NW, Farhat SC, Kozu K, Sallum AM, Appenzeller S, Sakamoto AP, Terreri MT, Pereira RM, Magalhaes CS, Ferreira JC, Barbosa CM, Gomes FH, Bonfa E, Silva CA, Brazilian Childhood-onset Systemic Lupus Erythematosus G (2017) Anti-ribosomal P antibody: a multicenter study in childhood-onset systemic lupus erythematosus patients. Lupus 26(5):484–489. https://doi.org/10.1177/0961203316676386
Hochberg MC (1997) Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 40(9):1725. https://doi.org/10.1002/1529–0131(199709)40:9<1725::AID-ART29>3.0.CO;2-Y
Vitali C, Bombardieri S, Jonsson R, Moutsopoulos HM, Alexander EL, Carsons SE, Daniels TE, Fox PC, Fox RI, Kassan SS, Pillemer SR, Talal N, Weisman MH (2002) Classification criteria for Sjogren's syndrome: a revised version of the European criteria proposed by the American-European consensus group. Ann Rheum Dis 61(6):554–558
The American College of Rheumatology nomenclature and case definitions for neuropsychiatric lupus syndromes (1999). Arthritis Rheum 42(4):599–608. doi:https://doi.org/10.1002/1529-0131(199904)42:4<599::AID-ANR2>3.0.CO;2-F
Bravo-Zehnder M, Toledo EM, Segovia-Miranda F, Serrano FG, Benito MJ, Metz C, Retamal C, Alvarez A, Massardo L, Inestrosa NC, Gonzalez A (2015) Anti-ribosomal P protein autoantibodies from patients with neuropsychiatric lupus impair memory in mice. Arthritis Rheumatol 67(1):204–214. https://doi.org/10.1002/art.38900
Barkhudarova F, Dahnrich C, Rosemann A, Schneider U, Stocker W, Burmester GR, Egerer K, Schlumberger W, Hiepe F, Biesen R (2011) Diagnostic value and clinical laboratory associations of antibodies against recombinant ribosomal P0, P1 and P2 proteins and their native heterocomplex in a Caucasian cohort with systemic lupus erythematosus. Arthritis Res Ther 13(1):R20. https://doi.org/10.1186/ar3244
Li J, Shen Y, He J, Jia R, Wang X, Chen X, Wang D, Han L, Zhu L, Chi X, Saschenbrecker S, Dahnrich C, Stocker W, Schlumberger W, Li ZG (2013) Significance of antibodies against the native ribosomal P protein complex and recombinant P0, P1, and P2 proteins in the diagnosis of Chinese patients with systemic lupus erythematosus. J Clin Lab Anal 27(2):87–95. https://doi.org/10.1002/jcla.21543
Acknowledgements
This work was supported by grants from the National Natural Science Foundation of China (81573222).
Author information
Authors and Affiliations
Contributions
H.-F.P. and Z.-J.L. designed the study; Y.-J.M., P.W., C.J., T.W., and L.-J.C. performed the experiments; Y.-J.M. and P.W. collected and analyzed the data; Y.-J.M. wrote the paper; H.-F.P. reviewed the paper.
Corresponding authors
Ethics declarations
Disclosures
None.
Additional information
Yong-Jun Mei and Peng Wang should be considered co-first authors.
Rights and permissions
About this article
Cite this article
Mei, YJ., Wang, P., Jiang, C. et al. Clinical and serological associations of anti-ribosomal P0 protein antibodies in systemic lupus erythematosus. Clin Rheumatol 37, 703–707 (2018). https://doi.org/10.1007/s10067-017-3886-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-017-3886-0