Abstract
Objectives
To identify the predictive value of anti-ribosomal P protein (anti-RibP) antibodies on the accrual of neuropsychiatric damage in systemic lupus erythematosus (SLE) patients in a large cohort in the Chinese SLE Treatment and Research group (CSTAR) database.
Methods
This single-center prospective study was conducted based on data from the CSTAR registry. At baseline, we collected demographic characteristics, autoantibody profiles, clinical manifestations, disease activity status, and organ damage. Follow-up data were collected by reviewing clinical records and telephone interviews. Anti-RibP antibodies were identified by immunoblot containing all three native RibP (P0, P1, P2) antigenic proteins.
Results
Of 2395 SLE patients with complete follow-up data, 659 (27.5%) were anti-RibP antibody positive. At baseline, positive anti-RibP antibodies were associated with a higher proportion of neurological involvement (𝑃 < 0.05). During follow-up, patients with positive anti-RibP antibodies were more likely to accumulate neuropsychiatric damage (adjusted HR = 3.8, 95% CI 2.7–57), p < 0.001). What is more, the cumulative probability of new-onset neurological involvement increased gradually in anti-RibP antibody–positive patients.
Conclusion
Anti-RibP antibodies can provide information about not only organ involvement at baseline, but also neuropsychiatric damage accrual and new-onset neurological involvement during follow-up. We suggested that anti-RibP antibody detection should be done in the newly diagnosed SLE patients to predict organ involvement and even the accumulation of neuropsychiatric damage.
Key Points
• Positive anti-RibP antibodies were associated with baseline neurological involvement.
• Baseline positive anti-RibP antibodies can predict the neuropsychiatric damage accrual and new-onset neurological involvement.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Systemic lupus erythematosus (SLE) is a complex autoimmune disease characterized by generation of autoantibodies [1]. Autoantibodies are closely associated with clinical manifestations and disease activity [2]. Among those SLE-related autoantibodies, anti-dsDNA antibody and anti-Sm antibody have been widely used in clinical diagnosis of SLE [3] and their relationship with organ involvement have been well studied [4]. Besides, other autoantibodies are also important in SLE pathogenesis [5]. Some were regarded as potential biomarkers to predict organ involvement and inform effective treatments [6]. Anti-ribosomal P protein (anti-RibP) antibodies direct to 3 ribosomal phosphoproteins (P0, P1, and P2) and are highly specific for SLE. Multiple studies have demonstrated that anti-RibP antibodies are associated with neuropsychiatric lupus erythematosus (NPSLE) [7], lupus hepatitis [8], and lupus nephritis (LN) [9]. With improvement in SLE survival, prevention of cumulative organ damage became a major goal in SLE management since it affects mortality and quality of life [10, 11]. However, the predictive value of the anti-RibP antibodies on organ damage has not been well studied due to the small case number. Therefore, in this single-center prospective study, we aimed to investigate the predictive value of anti-RibP antibodies on the accumulation of organ damage and probability of new-onset neurological involvement in a large CSTAR-based cohort of Chinese SLE patients.
Methods
Patients and follow-up
Chinese SLE treatment and research (CSTAR) is the first multi-center Chinese SLE cohort composed of 104 rheumatology centers from 30 provinces in China [12]. CSTAR launched in 2009 and has already described the major demographic and clinical manifestations of SLE patients [13]. Based on this prospective cohort, we consecutively collected 2516 patients registered in CSTAR and diagnosed SLE at Peking Union Medical College Hospital (PUMCH, the biggest center of CSTAR) from January 2006 to June 2020. All the patients fulfilled the revised American College of Rheumatology (ACR) classification criteria for SLE (1997) [14] or 2012 classification criteria of the Systemic Lupus International Collaborating Centers (SLICC) group [15]. Patients without autoantibody profile data were excluded (48 patients). After enrollment, all patients were followed up at the clinic. The loss to follow-up was defined as follows: the patient never revisited PUMCH and could not be contacted, or he or she chose to discontinue participation after enrollment. This study was approved by the Institute Review Board of PUMCH (Approval number, S-197).
Data collection and follow-up
The time of recruitment (baseline) was defined as the time of SLE diagnosis. We collected the baseline data through CSTAR online registry, including demography, clinical manifestations, laboratory data, Disease Activity Index 2000 (SLEDAI) [16], and Systemic Lupus International Collaborating Clinics/American College of Rheumatology damage index (SDI) [17]. Clinical records were reviewed to collect follow-up data, mainly for SDI at the individual organ systems and the occurring time of new organ damage. Telephone interviews were employed to supply additional data for analysis. We defined the end-point as the occurrence of new organ damage or the latest follow-up. Time in the Kaplan-Meier survival analysis for new organ damage in anti-RibP antibody–positive and anti-RibP antibody–negative patients was measured from baseline to end-point.
Measures
The clinical manifestations in our study included malar rash, discoid skin lesions, photosensitivity, arthritis, oral ulcerations, alopecia, serositis, vasculitis, nephropathy, neurological involvement, and hematological involvement. Neurological involvement was defined as seizures, psychosis mononeuritis multiplex, vasculitis myelitis, peripheral or cranial neuropathy, or acute confusional state in the absence of offending drugs or known metabolic derangements [15]. Nephropathy was defined clinically (persistent proteinuria > 0.5 grams per day or cellular casts) [15] or histologically (renal biopsy compatible with LN histopathology classes I, II, III, IV) [18]. Hematologic involvement was defined as hemolytic anemia with reticulocytosis or leukopenia (< 4000/mm3 on ≥ 2 occasions) or lymphopenia (< 1500/mm3 on ≥ 2 occasions) or thrombocytopenia (< 100,000/mm3) in the absence of offending drugs. SLEDAI [16] was used to assess disease activity. SDI, which covers 12 organ systems, was adopted to evaluate organ damage of SLE patients [17]. Neuropsychiatric damage was defined as an increase of at least one point in the neural domain of the SDI damage index, including cognitive impairment or major psychosis, seizures requiring therapy for 6 months, cerebrovascular accident, cranial or peripheral neuropathy (excluding optic), and transverse myelitis. Cognitive impairment included memory deficit, difficulty with calculation, poor concentration, difficulty in spoken or written language, and impaired performance level. Other neuropsychiatric damages were diagnosis through neuroimaging, including brain MRI/MRA (magnetic resonance angiography), and/or electrophysiological studies [19].
The autoantibodies were all measured at the lab of PUMCH with the same assays. Anti-nuclear antibody (ANA) was detected by indirect immunofluorescence (IIF) assay with Hep-2 cell line from Euroimmun AG (Lübeck, Germany). Anti-dsDNA antibody was tested by IIF using flagellate protoctista substrates and enzyme-linked immunosorbent assay (ELISA) using IMTEC ds-DNA Antibodies ELISA KT (Human Worldwide, Wiesbaden, Germany). Anti-extractable nuclear antigen (ENA) antibodies were tested with the immunoblotting assay using the EUROLINE ENA Profile 9 Ag (Euroimmun) according to the manufacturer’s instructions. Anti-RibP antibodies were identified by immunoblot containing all three native RibP (P0, P1, P2) antigenic proteins. The antiphospholipid (aPL) antibodies, including IgG or IgM anticardiolipin antibodies, anti-𝛽2 glycoprotein I, and lupus anticoagulant, were tested using ELISA (anticardiolipin and anti-𝛽2 glycoprotein I antibody) or dilute Russell viper venom test (lupus anticoagulant).
Statistical analyses
Descriptive statistics are presented as frequency for categorical variables and median ± standard deviations (SD) for continuous variables. Chi-square tests were performed to identify the association between baseline clinical manifestations and anti-RibP antibodies. We adopted univariable and multivariate regression analysis of the cox proportional hazard model to determine the prediction value of anti-RibP antibodies on organ damage accumulation. The Kaplan-Meier method was used for survival analysis, and the log-rank test was adopted to compare the survival rates between the anti-RibP antibody–positive and anti-RibP antibody–negative groups. The results were presented as hazard ratios (HRs) and 95% confidence intervals (CIs). All tests of significance were two-sided, and a 𝑃 value of < 0.05 was considered statistically significant. Statistical analysis was performed by using SPSS 24.0 (IBM, Armonk, NY, USA) and R Statistical Software, version 3.6.1. (R Foundation for Statistical Computing, Vienna, Austria).
Results
Baseline clinical manifestations of SLE patients
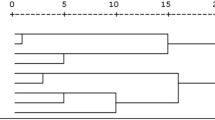
In this prospective study, 2516 SLE patients were enrolled. Among them, 121 (4.8%) patients were lost to follow-up after recruitment. Included in further analysis were 2395 patients with complete follow-up data (163 males and 2232 female patients). The presence of anti-RibP antibodies in this study was 27.5% (659/2395) (Table 1). No correlation was found between the reactivity of anti-RibP antibodies and other antibodies (Fig. 1).
The association between anti-RibP antibodies and baseline clinical manifestations
The association analysis revealed that, compared with negative anti-RibP antibodies patients, patients with positive anti-RibP antibodies had a higher rate of neurological involvement (24.6% vs 19.4%, 𝑃 < 0.05), malar rash (45.8% vs 38.7%, 𝑃 < 0.05), photosensitivity (7.1% vs 4.6%, 𝑃 < 0.05), alopecia (45.8% vs 38.7%, 𝑃 < 0.05), and arthritis (55.5% vs 50.5%, 𝑃 < 0.05) at baseline (Table 2).
Survival analysis
The predictive value of anti-RibP antibodies on organ damage accrual
During the follow-up, 279 (11.65%) increases of SDI damage index occurred. The mean (± SD) time of follow-up was 4.9 (± 4.1) years. To identify the association between anti-RibP antibodies and irreversible organ damage, univariable cox regression analyses were carried out. Only items that included more than 20 patients were compared. As shown in Table 3, patients with positive anti-RibP antibodies were more often develop neuropsychiatric damage (HR = 5.79, 95% CI 4.05–8.27, 𝑃 < 0.001) and avascular necrosis (HR = 2.03, 95% CI 1.05–3.92, 𝑃 < 0.001) during the follow-up period than those with negative one. When the neuropsychiatric damage item was divided into its components, cognitive impairment (HR = 4.59, 95% CI 2.36–8.30, 𝑃 < 0.001) and cerebral vascular (HR = 2.89, 95% CI 1.79–4.66, 𝑃 < 0.001) were more common in anti-RibP antibody–positive patients. Besides neuropsychiatric damage, anti-RibP antibodies were also the risk factor of avascular necrosis (HR = 2.03, CI 1.05–3.92, 𝑃 < 0.001).
As shown in Fig. 2, there were significant differences between the neuropsychiatric damage accumulation of anti-RibP antibody–positive and anti-RibP antibody–negative patients (log-rank test, p < 0.05). To further identify the predictive value of anti-RibP antibodies on neuropsychiatric damage accrual, we carried out multivariable cox regression model (Table 3). Potential confounding factors included age at visit (years), sex, aPL antibodies, and baseline organ damage > 0. Besides positive anti-RibP antibodies, patients with younger age (HR = 0.97, 95% CI 0.94–0.99, p < 0.05), positive aPL antibodies (HR =1.8, 95% CI 1.3–2.7, p < 0.05), and presence of organ damage at baseline (HR = 1.5, 95% CI 1.3–1.8, p < 0.001) were also associated with neuropsychiatric damage accrual. After accounting for potential confounders, anti-RibP antibodies remained independently associated with increased neuropsychiatric damage accrual (adjusted HR = 3.8, 95% CI 2.7–5.7, p < 0.001).
The cumulative probability of new-onset neurological involvement in anti-RibP antibody–positive patients
As shown in Table 2, among the 659 patients with positive anti-RibP antibodies, 162 patients showed neurological involvement at baseline. The other 497 patients without neurological involvement at baseline were included in the sub-group analysis. The follow-up period was 11.5 years, as all the new-onset neurological involvement occurred during this period. The rate of appearance of neurological involvement gradually increased during the follow-up period (Fig. 3). Patients with positive anti-RibP antibodies were more likely to develop neurological involvement than those with negative ones (log-rank test, p < 0.05). Before the endpoint, 12.1% (60/497) anti-RibP antibody–positive patients develop neurological symptoms, which was higher than that in anti-RibP antibody–negative patients (1.9%, 26/1389).
Discussion
In this study, we identified the role of anti-RibP antibodies in SLE in a large prospective cohort (2395). We confirmed the associations between anti-RibP antibodies and neurological involvement, neuropsychiatric damage, alopecia, malar rash, and avascular necrosis. Since organ damage has become more and more critical in SLE management, the feasibility of predicting the accumulation of organ damage has gained interest. The associations discovered in our study indicated that anti-RibP antibodies may be effective not only in the prediction of organ involvement but also in the accumulation of neuropsychiatric damage.
Anti-RibP antibody is a specific autoantibody of SLE [20] and has been reported to be associated with NPSLE [7, 21, 22] and hepatitis [23]. Anti-RibP antibodies bind to the key components of the 60S ribosomal subunit [24]. The immunoassays target the three RibP antigens (P0, P1, P2) and (or) the C-terminal 22 amino acid peptide (C22, key epitope on P0, P1, P2) [25]. According to an international meta-analysis involving > 6752 patients, this autoantibody was associated with CNS involvement, depression, and psychosis [23]. However, some studies demonstrated that anti-RibP antibodies had low sensitivity (26%) and specificity (80%) for NPSLE [26]. Our study confirmed the association between anti-RibP antibodies and baseline neurological involvement.
Although it is well accepted that anti-RibP antibodies are associated with neurological involvements, much of this information was derived from cross-sectional studies, and few of them focus on its prediction value on the accumulation of organ damage during follow-up [27]. Hanly et al. clarified that anti-RibP antibodies were associated with neurological involvements that occurred around the time of diagnosis [28]. Milena Mimica et al. [29] identified that the presence of anti-nucleosome antibodies could predict neural damage accrual, but anti-RibP antibodies cannot. Older age, higher disease activity, positive anti-Ro/SSA antibody, and positive aPL antibodies at baseline have also been reported to be associated with the development of neuropsychiatric damage [30,31,32]. To our best knowledge, the present study is the first to indicate the predictive value of anti-RibP antibodies on neuropsychiatric damage accrual and avascular necrosis (Table 3). What is more, we identified the cumulative probability of new-onset neurological involvement in patients with positive anti-RibP antibodies and negative neural symptoms at baseline. As the largest registry cohort study in China, CSTAR has already disclosed the features of SLE patients in China [33]. Our study might draw attention to the importance of optimizing interventions in patients with positive anti-RibP antibodies to prevent the accrual of neuropsychiatric damage.
Previous studies have provided theoretical evidence of the pathological properties anti-RibP antibodies may play in the accumulation of neuropsychiatric damage [34,35,36]. Anti-RibP antibodies have been reported to bind to the antigen on the neural cell membrane in the limbic system, hippocampus, and cingulate cortex [34, 35]. In murine models, anti-RibP antibodies can localize in olfactory piriform brain regions and give rise to depression-like behavior [36]. What is more, it can alter the blood-brain barrier and evoke inflammatory responses [9, 37]. However, few studies considered the fluctuation of anti-RibP antibodies, which may lead to a controversial value of anti-RibP antibodies for neuropsychiatric damage accumulation. Further studies are needed to clarify the role of anti-RibP antibodies in NPSLE pathogenesis.
Nevertheless, our study has some limitations. Our analysis did not clarify the exact pathological properties that enable anti-RibP antibodies to cause neuropsychiatric damage. Secondly, the cox analysis did not consider the fluctuation of anti-RibP antibodies. What is more, we lack data on therapeutic factors which may influence damage progression. International cohorts and further investigation into the pathological role of anti-RibP antibodies are needed.
Conclusion
In conclusion, our data demonstrated the association between anti-RibP antibodies and clinical manifestations, as well as the accumulation of organ damage. We suggest that more attention should be paid on the management of anti-RibP antibody–positive patients to predict the occurrence of organ involvements and even the accumulation of organ damage.
Availability of data and material
Yes.
Code availability
Yes.
References
Tsokos GC (2011) Systemic lupus erythematosus. N Engl J Med 365(22):2110–2121. https://doi.org/10.1056/NEJMra1100359
Yaniv G, Twig G, Shor DB, Furer A, Sherer Y, Mozes O, Komisar O, Slonimsky E, Klang E, Lotan E, Welt M, Marai I, Shina A, Amital H, Shoenfeld Y (2015) A volcanic explosion of autoantibodies in systemic lupus erythematosus: a diversity of 180 different antibodies found in SLE patients. Autoimmun Rev 14(1):75–79. https://doi.org/10.1016/j.autrev.2014.10.003
Aringer M, Costenbader K, Daikh D, Brinks R, Mosca M, Ramsey-Goldman R, Smolen JS, Wofsy D, Boumpas DT, Kamen DL, Jayne D, Cervera R, Costedoat-Chalumeau N, Diamond B, Gladman DD, Hahn B, Hiepe F, Jacobsen S, Khanna D et al (2019) 2019 European League Against Rheumatism/American College of Rheumatology Classification Criteria for Systemic Lupus Erythematosus. Arthritis Rheum 71(9):1400–1412. https://doi.org/10.1002/art.40930
Ghiggeri GM, D'Alessandro M, Bartolomeo D, Degl'Innocenti ML, Magnasco A, Lugani F, Prunotto M, Bruschi M (2019) An update on antibodies to necleosome components as biomarkers of sistemic lupus erythematosus and of lupus flares. Int J Mol Sci 20(22):5799. https://doi.org/10.3390/ijms20225799
Mohan C, Putterman C (2015) Genetics and pathogenesis of systemic lupus erythematosus and lupus nephritis. Nat Rev Nephrol 11(6):329–341. https://doi.org/10.1038/nrneph.2015.33
Fava A, Petri M (2019) Systemic lupus erythematosus: diagnosis and clinical management. J Autoimmun 96:1–13. https://doi.org/10.1016/j.jaut.2018.11.001
Bonfa E, Golombek SJ, Kaufman LD, Skelly S, Weissbach H, Brot N, Elkon KB (1987) Association between lupus psychosis and anti-ribosomal P protein antibodies. N Engl J Med 317(5):265–271. https://doi.org/10.1056/nejm198707303170503
Arnett FC, Reichlin M (1995) Lupus hepatitis: an under-recognized disease feature associated with autoantibodies to ribosomal P. Am J Med 99(5):465–472. https://doi.org/10.1016/s0002-9343(99)80221-6
Arinuma Y, Kikuchi H, Hirohata S (2019) Anti-ribosomal P protein antibodies influence mortality of patients with diffuse psychiatric/neuropsychological syndromes in systemic lupus erythematous involving a severe form of the disease. Mod Rheumatol 29(4):612–618. https://doi.org/10.1080/14397595.2018.1508801
Bruce IN, O'Keeffe AG, Farewell V, Hanly JG, Manzi S, Su L, Gladman DD, Bae SC, Sanchez-Guerrero J, Romero-Diaz J, Gordon C, Wallace DJ, Clarke AE, Bernatsky S, Ginzler EM, Isenberg DA, Rahman A, Merrill JT, Alarcón GS et al (2015) Factors associated with damage accrual in patients with systemic lupus erythematosus: results from the Systemic Lupus International Collaborating Clinics (SLICC) Inception Cohort. Ann Rheum Dis 74(9):1706–1713. https://doi.org/10.1136/annrheumdis-2013-205171
Segura BT, Bernstein BS, McDonnell T, Wincup C, Ripoll VM, Giles I, Isenberg D, Rahman A (2020) Damage accrual and mortality over long-term follow-up in 300 patients with systemic lupus erythematosus in a multi-ethnic British cohort. Rheumatology (Oxford) 59(3):524–533. https://doi.org/10.1093/rheumatology/kez292
Li M, Zhang W, Leng X, Li Z, Ye Z, Li C, Li X, Zhu P, Wang Z, Zheng Y, Li X, Zhang M, Zhang F, Zhao Y, Zeng X (2013) Chinese SLE Treatment and Research group (CSTAR) registry: I. Major clinical characteristics of Chinese patients with systemic lupus erythematosus. Lupus 22(11):1192–1199. https://doi.org/10.1177/0961203313499086
Zhao J, Bai W, Zhu P, Zhang X, Liu S, Wu L, Ma L, Bi L, Zuo X, Sun L, Huang C, Tian X, Li M, Zhao Y, Zeng X (2016) Chinese SLE Treatment and Research group (CSTAR) registry VII: prevalence and clinical significance of serositis in Chinese patients with systemic lupus erythematosus. Lupus 25(6):652–657. https://doi.org/10.1177/0961203315625460
Hochberg MC (1997) Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 40(9):1725. https://doi.org/10.1002/art.1780400928
Petri M, Orbai AM, Alarcón GS, Gordon C, Merrill JT, Fortin PR, Bruce IN, Isenberg D, Wallace DJ, Nived O, Sturfelt G, Ramsey-Goldman R, Bae SC, Hanly JG, Sánchez-Guerrero J, Clarke A, Aranow C, Manzi S, Urowitz M et al (2012) Derivation and validation of the Systemic Lupus International Collaborating Clinics classification criteria for systemic lupus erythematosus. Arthritis Rheum 64(8):2677–2686. https://doi.org/10.1002/art.34473
Bombardier C, Gladman DD, Urowitz MB, Caron D, Chang CH (1992) Derivation of the SLEDAI. A disease activity index for lupus patients. The Committee on Prognosis Studies in SLE. Arthritis Rheum 35(6):630–640. https://doi.org/10.1002/art.1780350606
Gladman D, Ginzler E, Goldsmith C, Fortin P, Liang M, Urowitz M, Bacon P, Bombardieri S, Hanly J, Hay E, Isenberg D, Jones J, Kalunian K, Maddison P, Nived O, Petri M, Richter M, Sanchez-Guerrero J, Snaith M et al (1996) The development and initial validation of the Systemic Lupus International Collaborating Clinics/American College of Rheumatology damage index for systemic lupus erythematosus. Arthritis Rheum 39(3):363–369. https://doi.org/10.1002/art.1780390303
Hahn BH, McMahon MA, Wilkinson A, Wallace WD, Daikh DI, Fitzgerald JD, Karpouzas GA, Merrill JT, Wallace DJ, Yazdany J, Ramsey-Goldman R, Singh K, Khalighi M, Choi SI, Gogia M, Kafaja S, Kamgar M, Lau C, Martin WJ et al (2012) American College of Rheumatology guidelines for screening, treatment, and management of lupus nephritis. Arthritis Care Res 64(6):797–808. https://doi.org/10.1002/acr.21664
Hanly JG (2014) Diagnosis and management of neuropsychiatric SLE. Nat Rev Rheumatol 10(6):338–347. https://doi.org/10.1038/nrrheum.2014.15
Sturgill BC, Carpenter RR (1965) Antibody to ribosomes in systemic lupus erythematosus. Arthritis Rheum 8:213–218. https://doi.org/10.1002/art.1780080205
Shi ZR, Cao CX, Tan GZ, Wang L (2015) The association of serum anti-ribosomal P antibody with clinical and serological disorders in systemic lupus erythematosus: a systematic review and meta-analysis. Lupus 24(6):588–596. https://doi.org/10.1177/0961203314560003
Moore E, Huang MW, Putterman C (2020) Advances in the diagnosis, pathogenesis and treatment of neuropsychiatric systemic lupus erythematosus. Curr Opin Rheumatol 32(2):152–158. https://doi.org/10.1097/bor.0000000000000682
Choi MY, FitzPatrick RD, Buhler K, Mahler M, Fritzler MJ (2020) A review and meta-analysis of anti-ribosomal P autoantibodies in systemic lupus erythematosus. Autoimmun Rev 19(3):102463. https://doi.org/10.1016/j.autrev.2020.102463
Francoeur AM, Peebles CL, Heckman KJ, Lee JC, Tan EM (1985) Identification of ribosomal protein autoantigens. J Immunol 135(4):2378–2384
Mahler M, Kessenbrock K, Raats J, Fritzler MJ (2004) Technical and clinical evaluation of anti-ribosomal P protein immunoassays. J Clin Lab Anal 18(4):215–223. https://doi.org/10.1002/jcla.20026
Karassa FB, Afeltra A, Ambrozic A, Chang DM, De Keyser F, Doria A, Galeazzi M, Hirohata S, Hoffman IE, Inanc M, Massardo L, Mathieu A, Mok CC, Morozzi G, Sanna G, Spindler AJ, Tzioufas AG, Yoshio T, Ioannidis JP (2006) Accuracy of anti-ribosomal P protein antibody testing for the diagnosis of neuropsychiatric systemic lupus erythematosus: an international meta-analysis. Arthritis Rheum 54(1):312–324. https://doi.org/10.1002/art.21539
Schwartz N, Stock AD, Putterman C (2019) Neuropsychiatric lupus: new mechanistic insights and future treatment directions. Nat Rev Rheumatol 15(3):137–152. https://doi.org/10.1038/s41584-018-0156-8
Hanly JG, Urowitz MB, Siannis F, Farewell V, Gordon C, Bae SC, Isenberg D, Dooley MA, Clarke A, Bernatsky S, Gladman D, Fortin PR, Manzi S, Steinsson K, Bruce IN, Ginzler E, Aranow C, Wallace DJ, Ramsey-Goldman R et al (2008) Autoantibodies and neuropsychiatric events at the time of systemic lupus erythematosus diagnosis: results from an international inception cohort study. Arthritis Rheum 58(3):843–853. https://doi.org/10.1002/art.23218
Mimica M, Barra I, Ormeño R, Flores P, Calderón J, Padilla O, Bravo-Zehnder M, González A, Massardo L (2019) Predictors of damage accrual in systemic lupus erythematosus: a longitudinal observational study with focus on neuropsychological factors and anti-neuronal antibodies. Clin Rheumatol 38(11):3129–3137. https://doi.org/10.1007/s10067-019-04707-x
Conti F, Ceccarelli F, Perricone C, Leccese I, Massaro L, Pacucci VA, Truglia S, Miranda F, Spinelli FR, Alessandri C, Valesini G (2016) The chronic damage in systemic lupus erythematosus is driven by flares, glucocorticoids and antiphospholipid antibodies: results from a monocentric cohort. Lupus 25(7):719–726. https://doi.org/10.1177/0961203315627199
González LA, Pons-Estel GJ, Zhang J, Vilá LM, Reveille JD, Alarcón GS (2009) Time to neuropsychiatric damage occurrence in LUMINA (LXVI): a multi-ethnic lupus cohort. Lupus 18(9):822–830. https://doi.org/10.1177/0961203309104392
Mikdashi J, Handwerger B (2004) Predictors of neuropsychiatric damage in systemic lupus erythematosus: data from the Maryland lupus cohort. Rheumatology (Oxford) 43(12):1555–1560. https://doi.org/10.1093/rheumatology/keh384
Li J, Leng X, Li Z, Ye Z, Li C, Li X, Zhu P, Wang Z, Zheng Y, Li X, Zhang M, Tian XP, Li M, Zhao J, Zhang FC, Zhao Y, Zeng X (2014) Chinese SLE treatment and research group registry: III. association of autoantibodies with clinical manifestations in Chinese patients with systemic lupus erythematosus. J Immunol Res 2014:809389. https://doi.org/10.1155/2014/809389
Segovia-Miranda F, Serrano F, Dyrda A, Ampuero E, Retamal C, Bravo-Zehnder M, Parodi J, Zamorano P, Valenzuela D, Massardo L, van Zundert B, Inestrosa NC, González A (2015) Pathogenicity of lupus anti-ribosomal P antibodies: role of cross-reacting neuronal surface P antigen in glutamatergic transmission and plasticity in a mouse model. Arthritis Rheum 67(6):1598–1610. https://doi.org/10.1002/art.39081
Szmyrka M, Pokryszko-Dragan A, Słotwiński K, Gruszka E, Korman L, Podemski R, Wiland P (2019) Cognitive impairment, event-related potentials and immunological status in patients with systemic lupus erythematosus. Adv. Clin Exp Med 28(2):185–192. https://doi.org/10.17219/acem/76711
Katzav A, Solodeev I, Brodsky O, Chapman J, Pick CG, Blank M, Zhang W, Reichlin M, Shoenfeld Y (2007) Induction of autoimmune depression in mice by anti-ribosomal P antibodies via the limbic system. Arthritis Rheum 56(3):938–948. https://doi.org/10.1002/art.22419
Hirohata S, Sakuma Y, Matsueda Y, Arinuma Y, Yanagida T (2018) Role of serum autoantibodies in blood brain barrier damages in neuropsychiatric systemic lupus erythematosus. Clin Exp Rheumatol 36(6):1003–1007
Acknowledgments
We thank CSTAR co-authors as following for assistance with cases collections. All the authors approved the submitted version for publication. All data relevant to the study are included in the article.
Funding
This work was supported by the Chinese National Key Technology R&D Program, Ministry of Science and Technology (2017YFC0907601, 2017YFC0907602, 2017YFC0907603, 2021YFC2501300), Beijing Municipal Science & Technology Commission (No. Z 201100005520022,23, 25-27), and CAMS Innovation Fund for Medical Sciences (CIFMS) (2021-I2M-1-005).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Yufang Ding, Jiuliang Zhao, and Mengtao Li. The first draft of the manuscript was written by Yufang Ding, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval
This study was approved by the institutional review board (IRB) of Peking Union Medical College Hospital (Approval number, S-197). Informed consent was obtained.
Disclosures
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ding, Y., Zhao, J., Qian, J. et al. The role of anti-ribosomal P autoantibodies in the prediction of neuropsychiatric damage in systemic lupus erythematosus based on CSTAR cohort (XIV). Clin Rheumatol 41, 1371–1379 (2022). https://doi.org/10.1007/s10067-021-06034-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-021-06034-6