Abstract
The manufacture of biologics is a complex process involving numerous steps. Over time, differences may arise as a result of planned changes to the manufacturing processes of a biologic from the same manufacturer. Comparability is the regulatory process that outlines the scope of an assessment required of an already licensed biologic after a manufacturing process change made by the same manufacturer. The aim of a comparability assessment is to demonstrate that any pre-manufacturing and post-manufacturing changes have no adverse impact on quality, safety, and efficacy of the biologic. A comparability assessment is distinct from a biosimilarity assessment, which involves extensive assessment of a biologic that is highly similar to the originator (reference product) in terms of quality, safety, and efficacy. The US Food and Drug Administration, European Medicines Agency, and World Health Organization have applied the fundamental comparability concepts into their respective biosimilarity guidance documents. In this review, we examine the rationale behind the distinct, highly regulated approval processes governing changes that may occur over time to an originator biologic due to planned manufacturing changes (as described by a comparability exercise) and those that outline the approval of a proposed biosimilar drug, based on its relationship with the reference product (biosimilarity evaluations).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Biologics are medicinal products whose active ingredients are created by biological processes rather than chemical synthesis. Biologics can include whole blood extracts or gene therapy products but primarily include protein molecules made by genetically engineering living bacterial, animal, or plant cells [1]. In contrast to chemically synthesized small-molecule drugs, biologics are typically 100-fold to 1000-fold larger in size, with a higher level of structural heterogeneity. Biologics are manufactured in complex, technically challenging processes involving multiple steps [1, 2].
Compared with biologics, small-molecule drugs are easier to replicate, thereby facilitating the manufacture of a homogeneous batch of an exact copy of the originator product. Copies of small-molecule drugs (known as “generic drugs”) can be manufactured by using non-proprietary manufacturing knowledge and standard chemical synthesis. Generic copies are equivalent to small-molecule drugs in terms of identity, quality, efficacy, and safety. The regulatory approval requirements for small-molecule generics are well established, and in the USA, this follows an Abbreviated New Drug Application, outlined in the US Drug Price Competition and Patent Term Restoration Act of 1984 [3]. This legislation is reflected in the US Food and Drugs Administration (FDA) guidance and states that large clinical studies designed to assure efficacy are not required to gain regulatory approval of generic copies of small-molecule drugs [4]. Rather, the regulatory foundations of creating a generic small-molecule drug are based on the consistent and robust production of an identical active ingredient, with the same dosage, efficacy, safety, and intended therapeutic indication as the originator. Indeed, generic copies of small-molecule drugs must only demonstrate bioequivalence to the originator [5, 6].
This same approach for small-molecule generic drugs cannot be applied directly to biologics because it is not possible to create an exact copy of a reference drug. Challenges in manufacturing a biologic primarily arise due to their size and complexity, as well as considerations that may include differences in expression systems and host cell lines [1]. Control of biological expression systems is complex, and minor variations of bioreactor control parameters can influence the product profile. Moreover, the product quality profile of biologics can be influenced by operational factors such as pH, temperature, and shear forces experienced during cell culture and downstream purification operations, formulation, and storage [7]. Consequently, a degree of micro-heterogeneity within and between batches of the same biologic product is routinely observed, which is typically not noted for small-molecule drugs.
Over the past decades, the ability to produce protein biologics, ranging from smaller proteins, such as hormones and growth factors, to highly complex monoclonal antibodies and fusion proteins by using recombinant DNA technology, has revolutionized the management of several diseases, including rheumatoid arthritis and several types of cancer [8, 9]. The approaching loss of patent exclusivity for a number of originator biologics has driven efforts by manufacturers to pursue the development and approval of biologics that are highly similar to the originator.
A biosimilar is a “biological medicinal product that contains a version of the active substance of an already authorized originator biologic” [10]. A biosimilar developer must demonstrate similarity to the originator product in terms of quality characteristics, biologic activity, safety, and efficacy based on a comprehensive similarity exercise [10, 11]. In contrast to the extensive industry experience in the development and approval of generic copies of small-molecule drugs, the development of biosimilars and the regulatory approval process is an emerging field [10]. A demonstrated lack of clinically meaningful differences between originator biologics and biosimilars forms the basis of the regulatory approval of biosimilars [10, 11].
A biopharmaceutical manufacturing process must comply with current Good Manufacturing Processes, with well-defined control strategies to guarantee the consistent production of high-quality products, be it the originator product or biosimilar, which ensure public safety and confidence that patient health care is not compromised. Patient safety remains the highest consideration in assessing all biologics, and potential concerns such as drug immunogenicity and host reaction-related safety are the primary challenges associated with the use of biologics in clinical practice [12]. As such, regulatory bodies and clinicians require a high level of assurance that the risk of immunogenicity of all biologics, including biosimilars, has been thoroughly evaluated during drug development and approval and through post-licensure approval pharmacovigilance [12].
This review examines the rationale behind the distinct, highly regulated approval processes governing changes that may occur over time with an originator biologic due to planned manufacturing changes (as covered by a comparability exercise) and those that underlie the approval of a proposed biosimilar drug, based on its relationship with the reference product (biosimilarity evaluations). This article also aims to provide a greater understanding of the term “biosimilar” which is clearly defined by regulatory authorities, and it is important that clinicians recognize that originator biologics which undergo planned manufacturing changes are not biosimilars.
Considerations in the manufacture of biologics
The biochemical, tertiary structures, activity, and stability characteristics of recombinant protein biologics are primarily influenced by their primary amino acid sequence, protein folding pattern, and post-translational modifications, such as glycosylation. In turn, the amino acid sequence gives rise to the corresponding secondary and higher order structures (i.e., tertiary or quaternary structures), the conformation of which may be influenced by other post-translational modifications [13, 14]. Ultimately, the structure and, consequently, the biological activity of the biologic can therefore be potentially influenced by events that occur not only throughout biosynthesis and purification but also during formulation and storage of the protein. Characterization of a biologic is a complex exercise and must be performed by using a broad range of orthogonal “state-of-the-art” physical, biochemical, and biological analytical methodologies [15].
Numerous processing factors can have an impact on the structure and intrinsic stability of biologic molecules. Manufacturers extensively characterize their processes and develop strategies to control process variability within an acceptable range of product characteristics during routine production [7]. Typical sources of variability can arise from bioreactor performance or purification operations or during the formulation of the drug product (Fig. 1). Several factors can influence the process performance and, in turn, the characteristics of the protein quality attributes. These factors include the source and grade of raw materials used, the culture media composition, the bioreactor operating conditions (e.g., culture duration, temperature, pH, and extent of agitation), the downstream purification processing steps, and the final formulation [15]. The selection of an appropriate host expression cell line (e.g., Chinese hamster ovary cell lines vs Sp2/0) is an important consideration in the development of a biologic, and the cultivation conditions in the bioreactor greatly dictate the glycosylation profile of these complex biologics. Glycosylation profiles, which contain appreciable levels of certain alpha-gal structures, can confer the potential for undesired immunogenicity [16].
Manufacturing of biologics. Adapted with permission [Mellstedt H. The challenge of biosimilars. Ann Oncol. 2008;19(3):411–9 by permission of the official journal of the European Society for Medical Oncology/ESMO] [7]
Defining control strategies for critical product quality characteristics of biologics, such as glycosylation, overall molecular charge heterogeneity, and degree of aggregation, requires substantial efforts by the manufacturer during the process characterization phase of product development. It is the capability to consistently and reproducibly control product quality characteristics within defined ranges that ensures the efficacy of the product and safety of the patient [11, 17]. Recombinant protein biologics, such as monoclonal antibodies and fusion proteins, are typically glycosylated (e.g., N-glycosylated and/or O-glycosylated), and control of the glycosylation profile of the biologic is a critical element in the manufacturing process. The glycosylation profile can potentially influence the biological activity, pharmacokinetic (PK) profile, serum half-life, induce effector functions, and, in some instances, the stability of the drug product. Typically, during the early stages of process development, significant effort will be applied to build the process knowledge to the degree of manufacturing controls required to ensure a consistent product quality profile that is safe and efficacious [18, 19].
Appropriate manufacturing process control and analytical testing strategies are then applied to assure the necessary degree of process and product quality consistency through in-process and end-product testing [20, 21]. The overall product control strategy includes detailed evaluations of raw materials, cell line testing, in-process sampling during manufacturing, analytical release testing, and stability testing over the intended storage conditions and time period. In addition, extensive characterization is typically conducted by using a variety of state-of-the-art analytical methods, as appropriate [22], to confirm that all aspects of the protein product quality profile are within the established ranges.
The potential influences of intended manufacturing variations are examined, typically during the early phases of process development. The manufacturer will develop an extensive knowledge base of how operating conditions may influence process performance characteristics and the relative proportions of the various structural isoforms [19]. As such, robust in-process and end-product analytical testing techniques are required that can detect minor differences, to provide biologic manufacturers and regulators with the necessary assurance that a process, once validated, will deliver a consistent product quality on a batch-to-batch basis [19].
Manufacturing implications for the approval of biologics
Unlike small-molecule drugs, the development pathway for a biologic is typically a lengthy and complex process. This is primarily due to the complexity of the molecules, and the extensive nature of development activities to support process and product characterization, optimal formulation, and appropriate storage conditions for the product [7]. The approval of a biologic must be supported by a comprehensive analytical characterization program, including the molecular integrity of the gene being expressed and the phenotypic and genotypic characteristics of the host cell after long-term cultivation [23]. In addition, suitably validated manufacturing process equipment and a stringent process control strategy that specifies the criteria to which the product or materials should conform are key elements that help ensure the consistency of the product throughout the manufacturing process [23]. All of these elements represent the manufacturing control components that underlie a fully characterized biologic and an appropriately validated manufacturing process [22].
Demonstrating comparability after manufacturing changes
The concept of a comparability assessment is outlined in the International Conference on Harmonization (ICH) Q5E: Comparability of Biotechnological/Biological Products Subject to Changes in Their Manufacturing Process [24]. This guidance document forms the regulatory framework that denotes the extent to which batches of the biologic from the same manufacturer are comparable both pre-manufacturing and post-manufacturing changes. The ICH Q5E guideline also outlines the requirements that will ensure that any detectable differences arising as a result of manufacturing changes do not adversely impact the safety and efficacy of the biologic (Fig. 2). In order to identify any potential change in the product quality attribute that may influence the quality, stability, safety, or efficacy profile of the product, a comparability exercise typically involves the detailed characterization of a number of representative lots of the biologic pre-manufacturing and post-manufacturing process change [25].
There are numerous reasons why a manufacturer may introduce a change to the manufacturing process, such as the need to qualify a new raw material to align with compendial requirements or to replace one that is no longer commercially available, to improve operations to comply with evolving regulatory requirements, to improve the safety profile of the original product, or to enhance the yield or robustness of the manufacturing process [24]. The scope of these modifications can range from relatively minor changes, such as process equipment changes, to more significant variations, e.g., those relating directly to in-process control strategies. The assessment of risk as a function of the manufacturing changes which potentially impact the safety and efficacy of a biologic will influence the amount and type of data required to evaluate comparability of the product pre-change and post-change. The biologic manufacturer will typically perform a comparability characterization study where an assessment is made of moderate or major risk of potential impact on the clinical profile [25]. All changes should be considered on a case-by-case basis; examples of substantive process changes include alterations to the cell line, culture media formulation changes, and modifications to the purification process, all of which are considered to have the potential to impact the quality characteristics of a biologic. Changes in processing or formulation with new excipients or drug product–delivery systems also have the potential to impact the characteristics and stability of the biologic [24].
Comparability: current regulatory perspectives
According to the guidance provided in the ICH Q5E guidelines, it is not essential that the quality attributes of the pre-change and post-change product are identical. As noted previously, the guidance requires that quality attributes must be similar and the manufacturer must demonstrate that any differences between pre-change and post-change product do not adversely affect the safety or efficacy of the biologic [24].
Comparability is determined based on a combination of detailed process characterization studies, comprehensive orthogonal and heightened characterization analytical tests, with supporting stability evaluations of the corresponding drug substance and/or drug product. In certain cases (e.g., potential cases where significant manufacturing changes have been undertaken and there are product quality differences that cannot be addressed through in vitro tests), supportive non-clinical and/or clinical studies may be required based on risk assessment considerations (Fig. 2) [24]. For example, the scale-up of production of Myozyme®/Lumizyme® (alglucosidase alfa; Genzyme, Cambridge, MA, USA) conducted within the same manufacturing organization revealed considerable differences in glycosylation and PK properties between the pre-change and post-change product, such that additional clinical studies were needed and a new biologics license application was required for Myozyme/Lumizyme [26]. Additional clinical studies were conducted to support comparability of alglucosidase alfa, as the analytical comparability data package and PK data failed to establish product comparability following switching of production to a larger production vessel to meet demand [27].
Establishing biosimilarity: fundamental principles
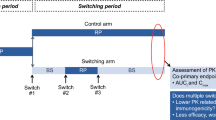
The technical considerations and regulatory approval pathway that are used to show biosimilarity are distinct from those required to show comparability of an originator biologic after a manufacturing change (Fig. 2). Biosimilarity requires a demonstration of the absence of clinically meaningful differences from the reference product, which must be confirmed with appropriate clinical studies, in accordance with European Medicines Agency (EMA), FDA, and World Health Organization (WHO) guidelines [10, 11, 23]. In addition, rigorous and extensive analytical assessments are the foundation of the similarity assessment [10, 11, 23].
In the determination of similarity with the originator (or reference product), various regulatory agencies have applied the “totality of evidence” paradigm whereby a regulatory authority will consider the entire data and information submitted in the application of a proposed biosimilar. This includes structural and functional characterization, non-clinical evaluation, human PK and pharmacodynamic (PD) studies, clinical immunogenicity assessments, and comparative clinical data to establish similarity between the potential biosimilar and the reference product, notwithstanding “minor differences in clinically inactive components” and that “there are no clinically meaningful differences in terms of the safety, purity, and potency of the product” [11]. The development of biosimilars is a rigorous and carefully controlled process, guided by the principles of the ICH Q5E guidance, Good Manufacturing Practice, by using the appropriate in-process controls and quality control strategies [23]. While the principles of ICH Q5E are helpful for biosimilar development, the regulatory expectation is very different, because demonstrating similarity requires a higher regulatory burden of proof than required when the same manufacturer makes an intended change to their own manufacturing process. This is because however rigorous the development of biosimilars are, developers do not have the depth of historical knowledge of the manufacturing process of the reference product and must therefore develop the relationship between their own process to the associated product quality profile via “reverse engineering” to achieve a product that is similar to the reference product. The biosimilar manufacturer must also take into account the variability of the reference product when establishing the quality ranges within which the biosimilar must lie. This is typically achieved by analyzing multiple lots of the reference product from a variety of regions and over an extended time period [10, 23].
As outlined above, manufacturers of originator biologics have developed extensive proprietary knowledge about their processes and product and the process development phase. This knowledge includes the detailed process history of the expression host cell line (e.g., master cell bank), the potential influence of various culture conditions, purification, and formulation processing factors of the associated product quality and stability profiles. Such technical knowledge is considered state-of-the-art practice in the biopharmaceutical industry; however, the process and technical understanding of the originator process are proprietary and confidential to the manufacturer. In addition, the biosimilar manufacturer will often be required to develop new PK and immunogenicity assays which are required to be in line with the current state of the art. In contrast to the requirements for a comparability exercise, all of the information for the PK and immunogenicity assays are available, as well as the specifications for the reagents. Although updates for the assays may be required to meet the current state of the art, this is less often the case for products that are in active development. Consequently, a biosimilar manufacturer faces a “knowledge gap” and must independently establish a new expression cell line and manufacturing process capable of delivering a drug that is highly similar to the reference product [10, 19]. To close this knowledge gap, the development of a biosimilar typically requires an iterative process of reverse engineering of the manufacturing process, focusing on critical product attributes and biological activity, which ultimately results in a biosimilar that is highly similar to the originator product via extensive and comprehensive biochemical and functional characterization evaluations [28].
The manufacturing steps are modified and adjusted until the characterization evaluations undertaken ultimately determine that the resulting biosimilar protein is deemed highly similar to those of the originator product. Subsequently, with regulatory review of the extensive process and analytical characterization data, the proposed biosimilar will undergo pre-clinical and clinical validation under regulatory oversight [28].
In essence, manufacturers of biosimilars must have a comprehensive and highly capable technical and process knowledge based on biopharmaceutical manufacturing capabilities, regulatory scientific know-how, and a clinical understanding of the originator product. This knowledge is harnessed in order to undertake a successful biosimilar development program, where the objective is to reverse engineer a product to be highly similar to the originator but with no or very limited proprietary knowledge of the originator product. This is in contrast to a comparability exercise that will utilize existing knowledge and experience with the product, as previously discussed.
Biosimilarity: current regulatory perspectives
There is general agreement among the EMA, FDA, and WHO regarding the overarching guiding principles in the development of biosimilars [10, 11, 23]. The EMA defines a biosimilar as “a biological medicinal product that contains a version of the active substance of an already authorized original biological medicinal product [reference medicinal product] in the European regulatory jurisdictions” [10]. Likewise, the FDA defines a biosimilar as a biologic product that is “highly similar to an FDA-approved biologic [the reference product] and has no clinically meaningful differences in terms of safety and effectiveness” [11]. These principles are echoed by the WHO guidelines in relation to the evaluation of “similar biotherapeutic products” (Table 1) [23].
Regulatory authorities have developed specific guidelines that set criteria for assessing biosimilarity. The EMA has led the way in establishing an approval pathway for biosimilar medicines. To date, the majority of biosimilars approved by the EMA have been recombinant versions of naturally occurring hormones and cytokines that have well-characterized structures and pharmacologic profiles, such as erythropoietin, growth hormones, and granulocyte colony-stimulating factors [29]. However, with more complex biologics such as monoclonal antibodies and fusion proteins forming a substantial focus for recent biosimilar development, current guidelines from the FDA [11], EMA [10], and WHO [23] are evolving to reflect the complexity and multifunctional nature of these molecules.
The WHO guidelines comprise globally accepted standards for the regulatory approval of biosimilars, which emphasize the stringent review and approval processes needed to ensure that no clinically meaningful differences exist between the proposed biosimilar and the reference product in terms of safety, purity, and potency [23]. This includes a targeted clinical program encompassing comparative PK, PD, efficacy, and safety studies (including immunogenicity) appropriately powered to establish equivalence to the originator product as a comparator in the trials prior to regulatory approval [23]. These studies are followed by extensive post-approval pharmacovigilance to monitor safety and adverse events (Fig. 2) [22].
The WHO guidance was built on the principles originally outlined by the EMA [10]. Overall, the regulatory framework is much more stringent than that required for generic small-molecule products, and as such, the terms biosimilar and generic should not be used interchangeably [30]. Pharmacokinetic equivalence is necessary but not sufficient to demonstrate biosimilarity, since certain molecular differences, albeit minimal, can modify affinity for the target ligand without altering the PK profile [11]. Regulatory authorities draw a clear distinction between the documentation and approval process required for the registration of biosimilars and the path taken for assessment of manufacturing changes (comparability). Importantly, the totality of evidence, including structural, functional, immunogenic, PK, PD, and clinical similarities, is central in the appraisal of proposed biosimilars. Indeed, the FDA embraced this concept and has provided guidance on considering the totality of evidence and details the unique approach to both structural and functional evaluation in the assessment of biosimilarity [11]. The first biosimilar to be approved under the FDA 351(k) pathway was Zarxio™ (a recombinant granulocyte colony-stimulating factor; Sandoz Inc., Princeton, NJ, USA) [31], and more recently, the first biosimilar monoclonal antibody was approved by the FDA (Inflectra™, a biosimilar version of infliximab; Celltrion Inc., Incheon, Republic of Korea) [32]. Multiple proposed biosimilars are under review by the FDA, with the expectation that submissions and approvals will significantly increase in the coming years.
The role of regulatory standards: non-comparable biotherapeutic products are not biosimilars
In some countries, biologics that claim biosimilarity are available to the public, but they have not undergone the degree of extensive and rigorous scientific and clinical evaluations such as those stipulated by the FDA [11], EMA [10], and WHO [23]. Consequently, these products, which may not have been analyzed directly against a licensed reference product, with possible unintentional structural or chemical changes, are known as “non-comparable biotherapeutic products” (also known as “intended copies” or “biomimics”) and should not be regarded as biosimilars [24].
The clinical profile of non-comparable biotherapeutic products is unclear, with little data available on their efficacy and safety. The potential for clinically relevant differences in formulation and dosage is also unclear, with the potential for compromised patient care (Table 1). Since these products are not considered biosimilars, the terms non-comparable biotherapeutic product and biosimilar must not be used interchangeably, as outlined in the International Federation of Pharmaceutical Manufacturers and Associations (IFPMA) policy statement on non-comparable biotherapeutic products [22].
Comparability and biosimilarity: defining features and practical distinctions
Fundamental defining features underpin concepts of comparability and biosimilarity. A comparability assessment provides sufficient evidence to assure that the efficacy and safety profiles of the post-change product are within pre-change ranges. This can be assessed based on extensive clinical and manufacturing history, supported by analytical methods and controls used throughout the development and post-approval history of the product. Using a risk-based approach, the need for supportive pre-clinical or clinical data is determined on a case-by-case basis.
This is in contrast to the development of a biosimilar, which is based on reverse engineering, extensive rounds of process development, and analytical characterization to produce a product that is highly similar to the reference product, all conducted with limited information on the originator’s manufacturing processes. Consequently, this process may involve using a new cell line, newly developed cell culture conditions, purification process, and, in some instances, more contemporary formulation to that used for the originator. As such, the biosimilar manufacturer must have a detailed knowledge of the product quality and stability characteristics of the reference product and the proposed biosimilar in the evaluation of the potential impact on the biological function, structural integrity, stability, efficacy, safety, and immunogenicity.
Owing to the proprietary knowledge of the manufacturing process of the originator, which is not publicly revealed, the development of a proposed biosimilar involves reverse engineering through the implementation of current manufacturing technologies and best practices in the production of the biosimilar candidate. In the development of a biosimilar, a thorough understanding of the originator product (including critical quality attributes and mechanism of action) must be in place in order to develop a manufacturing process for the proposed biosimilar, utilizing state-of-the-art analytical methods (Table 2).
Conclusions
While there are common regulatory and scientific aspects, a clear understanding of the distinctions between comparability and biosimilarity is integral to the development of biologics. Comparability refers to the regulatory process followed to evaluate any potential differences arising as a result of planned changes made over time to the manufacturing methods of a biologic from the same manufacturer, demonstrating no adverse impact on safety and efficacy of the product. Comparability differs from biosimilarity assessments, which involve the careful and extensive demonstration of similar product quality, safety, and efficacy to the reference product as developed by a different manufacturer according to the totality of evidence generated from the combination of detailed characterization studies and supportive clinical trial data.
The higher level of evidence (i.e., totality of evidence) required to establish biosimilarity during regulatory review compared with that typically needed to show comparability reflects the recognition by regulators of the importance of the depth of the proprietary knowledge of the manufacturer of the reference product and their capability to manage changes in their manufacturing process. In the absence of such proprietary knowledge of manufacturing processes for biosimilar developers, and given technical and scientific advancement of biotechnology manufacturing over the past 25 years, the FDA, EMA, and WHO have successfully applied the foundational comparability concepts into biosimilarity guidance. These guidance documents provide a robust and scientifically sound overarching framework for the development, regulatory review, and approval of biosimilars.
References
Morrow T, Felcone LH (2004) Defining the difference: what makes biologics unique. Biotechnol Healthc 1:24–29
Kuhlmann M, Covic A (2006) The protein science of biosimilars. Nephrol Dial Transplant 21(Suppl 5):v4–8. doi:10.1093/ndt/gfl474
US Food and Drug Admiistration, Troy DE (2013) Drug Price Competition and Patent Term Restoration Act of 1984 (Hatch-Waxman Amendments). US Department of Heralth & Human Services. http://www.fda.gov/newsevents/testimony/ucm115033.htm. Accessed 5 July 2016
US Food and Drug Administration (2011) Submission of summary bioequivalence data for ANDAs. U.S. Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research (CDER). http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM134846.pdf. Accessed 5 July 2016
Morais JA, Lobato Mdo R (2010) The new European Medicines Agency guideline on the investigation of bioequivalence. Basic Clin Pharmacol Toxicol 106:221–225. doi:10.1111/j.1742-7843.2009.00518.x
Meyer MC (2001) United States Food and Drug Administration requirements for approval of generic drug products. J Clin Psychiatry 62(Suppl 5):4–9, discussion 23-24
Mellstedt H, Niederwieser D, Ludwig H (2008) The challenge of biosimilars. Ann Oncol 19:411–419. doi:10.1093/annonc/mdm345
Zelenetz AD, Ahmed I, Braud EL, Cross JD, Davenport-Ennis N, Dickinson BD, Goldberg SE, Gottlieb S, Johnson PE, Lyman GH, Markus R, Matulonis UA, Reinke D, Li EC, DeMartino J, Larsen JK, Hoffman JM (2011) NCCN biosimilars white paper: regulatory, scientific, and patient safety perspectives. J Natl Compr Canc Netw 9(Suppl 4):S1–22
Walsh G (2010) Biopharmaceutical benchmarks 2010. Nat Biotechnol 28:917–924. doi:10.1038/nbt0910-917
Committee for Medicinal Products for Human Use (CHMP) (2014) Guideline on similar biological medicinal products containing biotechnology-derived proteins as active substance: non-clinical and clinical issues. European Medicines Agency. http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2015/01/WC500180219.pdf. Accessed 5 July 2016
US Food and Drug Administration (2015) Scientific considerations in demonstrating bosimilarity to a reference product. Department of Health and Human Services, Center for Drug Evaluation and Research (CDER), Center for Biologics Evaluation and Research (CBER). http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM291128.pdf. Accessed 5 July 2016
Garces S, Antunes M, Benito-Garcia E, da Silva JC, Aarden L, Demengeot J (2014) A preliminary algorithm introducing immunogenicity assessment in the management of patients with RA receiving tumour necrosis factor inhibitor therapies. Ann Rheum Dis 73:1138–1143. doi:10.1136/annrheumdis-2013-203296
Declerck PJ (2013) Biosimilar monoclonal antibodies: a science-based regulatory challenge. Expert Opin Biol Ther 13:153–156. doi:10.1517/14712598.2012.758710
Dorner T, Strand V, Castaneda-Hernandez G, Ferraccioli G, Isaacs JD, Kvien TK, Martin-Mola E, Mittendorf T, Smolen JS, Burmester GR (2013) The role of biosimilars in the treatment of rheumatic diseases. Ann Rheum Dis 72:322–328. doi:10.1136/annrheumdis-2012-202715
Graumann K, Premstaller A (2006) Manufacturing of recombinant therapeutic proteins in microbial systems. Biotechnol J 1:164–186. doi:10.1002/biot.200500051
Berger M, Kaup M, Blanchard V (2012) Protein glycosylation and its impact on biotechnology. Adv Biochem Eng Biotechnol 127:165–185. doi:10.1007/10_2011_101
Sarpatwari A, Avorn J, Kesselheim AS (2015) Progress and hurdles for follow-on biologics. N Engl J Med 372:2380–2382. doi:10.1056/NEJMp1504672
Nowicki M (2007) Basic facts about biosimilars. Kidney Blood Press Res 30:267–272. doi:10.1159/000105133
Lee JF, Litten JB, Grampp G (2012) Comparability and biosimilarity: considerations for the healthcare provider. Curr Med Res Opin 28:1053–1058. doi:10.1185/03007995.2012.686902
Ramanan S, Grampp G (2014) Drift, evolution, and divergence in biologics and biosimilars manufacturing. BioDrugs 28:363–372. doi:10.1007/s40259-014-0088-z
Kay J, Smolen JS (2013) Biosimilars to treat inflammatory arthritis: the challenge of proving identity. Ann Rheum Dis 72:1589–1593. doi:10.1136/annrheumdis-2012-203198
International Federation of Pharmaceutical Manufacturers & Associations (IFPMA) (2014) Policy statement. Non-comparable biotherapeutic products. IFPMA. http://www.ifpma.org/wp-content/uploads/2016/02/Non-comparable_Biotherapeutic_Products__English__02.pdf. Accessed 5 July 2016
World Health Organization (2010) Guidelines on evaluation of similar biotherapeutic products (SBPs). World Health Organization. http://www.who.int/biologicals/areas/biological_therapeutics/BIOTHERAPEUTICS_FOR_WEB_22APRIL2010.pdf. Accessed 5 July 2016
International Conference on Harmonisation (ICH), ICH Expert Working Group (2009) ICH harmonised tripartite gudieline: pharmaceutical development Q8 (R2): current Step 4 version. International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use. http://www.ich.org/fileadmin/Public_Web_Site/ICH_Products/Guidelines/Quality/Q8_R1/Step4/Q8_R2_Guideline.pdf. Accessed 5 July 2016
International Conference on Harmonisation (ICH), ICH Expert Working Group (2004) ICH harmonised tripartite guideline: comparability of biotechnological/biological products subject to changes in their manufacturing process. Q5E. International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use. http://www.ich.org/fileadmin/Public_Web_Site/ICH_Products/Guidelines/Quality/Q5E/Step4/Q5E_Guideline.pdf. Accessed 5 July 2016
Declerck P, Farouk-Rezk M, Rudd PM (2015) Biosimilarity versus manufacturing change: two distinct concepts. Pharm Res. doi:10.1007/s11095-015-1790-3
US Food and Drug Adminstration, Yao L (2008) Meeting of the Endocrinologic and Metabolic Drugs Advisory Committee (EMDAC) to evaluate myozyme (alglucosidase alfa) for the treatment of late onset Pompe disease. Clinical background materials. US Food and Drug Administrtion, Center for Drug Evaluation and Research (CDER). http://www.fda.gov/ohrms/dockets/ac/08/briefing/2008-4389b1-01-FDA.pdf. Accessed 5 July 2016
McCamish M, Woollett G (2011) Worldwide experience with biosimilar development. MAbs 3:209–217
Committee for Medicinal Products for Human Use (CHMP) (2016) European public assessment reports: biosimilars. European Medicines Agency. http://www.ema.europa.eu/ema/index.jsp?curl=pages%2Fmedicines%2Flanding%2Fepar_search.jsp&mid=WC0b01ac058001d125&searchTab=searchByAuthType&alreadyLoaded=true&isNewQuery=true&status=Authorised&status=Withdrawn&status=Suspended&status=Refused&keyword=Enter+keywords&searchType=name&taxonomyPath=&treeNumber=&searchGenericType=biosimilars&genericsKeywordSearch=Submit. Accessed 5 July 2016
de Mora F (2015) Biosimilar: what it is not. Br J Clin Pharmacol 80:949–956. doi:10.1111/bcp.12656
Colwell J (2015) FDA approves first biosimilar, Zarxio. Cancer Discov 5:460. doi:10.1158/2159-8290.CD-ND2015-002
US Food and Drug Admiistration (2016) FDA approves Inflectra, a biosimilar to Remicade [news release]. US Department of Health & Human Services. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm494227.htm. Accessed 5 July 2016
Martinusen DJ, Lo C, Marin JG, Tsao NW, Leung M (2014) Potential impact of subsequent entry biologics in nephrology practice in Canada. Can J Kidney Health Dis 1:32. doi:10.1186/s40697-014-0032-7
Castañeda-Hernández G, González-Ramírez R, Kay J, Scheinberg MA (2015) Biosimilars in rheumatology: what the clinician should know. RMD Open 1:e000010
Beck A (2011) Biosimilar, biobetter and next generation therapeutic antibodies. MAbs 3:107–110
Weise M, Bielsky MC, De Smet K, Ehmann F, Ekman N, Giezen TJ, Gravanis I, Heim HK, Heinonen E, Ho K, Moreau A, Narayanan G, Kruse NA, Reichmann G, Thorpe R, van Aerts L, Vleminckx C, Wadhwa M, Schneider CK (2012) Biosimilars: what clinicians should know. Blood 120:5111–5117. doi:10.1182/blood-2012-04-425744
Declerck PJ, Farouk-Rezk M, Rudd PM (2016) Biosimilarity versus manufacturing change: two distinct concepts. Pharm Res 33:261–268. doi:10.1007/s11095-015-1790-3
Acknowledgments
Medical writing support was provided by Neel Misra, MSc, CMPP, of Engage Scientific Solutions and was funded by Pfizer. The authors would like to thank Chee-Keng Ng of Pfizer for his contributions to the manuscript. The authors also wish to thank Shivanthy Arnold, Beverly Ingram, and Judith Macdonald, all of Pfizer, for their contributions to the regulatory sections of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Authors had control of all primary data. Valderilio Azevedo has received unrestricted grants or served on speakers bureaus for AbbVie, Bristol-Myers Squibb, Janssen, Novartis, Pfizer, Roche, Celltrion, UCB, and AstraZeneca. João Eurico Fonseca has received unrestricted research grants or served on speakers bureaus for AbbVie, Amgen, Bristol-Myers Squibb, Janssen, Merck Sharp & Dohme, Novartis, Novo Nordisk, Pfizer, Roche, Servier, and UCB. Tatsuya Atsumi has accepted honoraria for educational meetings from Mitsubishi Tanabe Pharma, Chugai Pharmaceutical Co., Astellas Pharma Inc., Takeda Pharmaceutical Co., Pfizer Inc., AbbVie Inc., and Eisai and has received a research grant from Astellas Pharma Inc., Takeda Pharmaceutical Co., Mitsubishi Tanabe Pharma Corporation, Chugai Pharmaceutical Co., Daiichi-Sankyo, Otsuka Pharmaceutical, and Pfizer Inc. Brian Hassett, Javier Coindreau, Ira Jacobs, Ehab Mahgoub, Julie O’Brien, Ena Singh, Steven Vicik, and Brian Fitzpatrick are full-time employees of Pfizer.
Funding
This report is supported by Pfizer Inc.
Rights and permissions
About this article
Cite this article
Azevedo, V., Hassett, B., Fonseca, J.E. et al. Differentiating biosimilarity and comparability in biotherapeutics. Clin Rheumatol 35, 2877–2886 (2016). https://doi.org/10.1007/s10067-016-3427-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-016-3427-2