Abstract
Biological medicines (biologics) are produced in living cells and purified in complex, multi-step processes. Compared with chemically synthesized small-molecule drugs, biologics are more sensitive to changes in manufacturing conditions. Process and product consistency should be founded on rigorous design and control of manufacturing processes, but consistency is ultimately ensured through robust quality systems. Even a minor change in any component of a quality system could lead to product drift, evolution, and divergence, which may impact the quality, safety, efficacy, and/or interchangeability of biologics. Unintended or unexplained deviations in manufacturing processes can lead to excursions in product attributes (i.e., drift). Well-managed quality systems can help detect and mitigate drift. Occasionally, quality attributes could shift outside of established acceptable ranges as the result of a known manufacturing change (defined here as evolution). Such changes should be studied extensively for effects on product safety and efficacy. With the advent of biosimilars, similar biologics will be produced by multiple manufacturers with different quality systems. Different patterns of product drift and evolution could contribute, over time, to clinically meaningful differences among biologics, including among originator products across regions and among originator products and biosimilar products, a process defined here as divergence. Manufacturers and policymakers can minimize the potential impact of divergence by establishing robust pharmacovigilance systems; requiring distinguishable names for all biologics, including both originator products and biosimilars; adhering to high standards for designations of interchangeability; and ensuring that patient medical records accurately reflect the specific biologic dispensed, especially if the biologic could be sourced from multiple manufacturers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Compared with small-molecule drugs, biological drugs are extremely sensitive to changes in the manufacturing process. |
Changes in biological product parameters can result from unknown deviations in the manufacturing process (drift) and known changes in the manufacturing process (evolution). Though some variability is normal, any changes must be rigorously investigated and controlled through robust quality systems. |
Biosimilars introduce new challenges because two products that were initially deemed biosimilar or interchangeable could each undergo unique patterns of drift and evolution, ultimately resulting in two products that are no longer biosimilar (divergence). |
Pharmacovigilance systems, distinguishable product names, robust standards of interchangeability, and procedures for pharmacist–physician communication in the event of substitution can reduce patient risk. |
1 Introduction
Biological medicines (biologics) are made from living organisms [1], and manufacturing of recombinant biologics involves cell line development, cell culture, harvest, purification, formulation, filling, finishing, and packaging. Additionally, biologics are relatively heterogeneous compared with small-molecule or chemical drugs and contain a complex mixture of molecular entities including the components of the active ingredient, their structural variants, and impurities [2]. In contrast, small-molecule drugs are synthesized via a series of well-defined chemical reactions and have well-defined structures and compositions [2]. As biologics are complex molecules manufactured by living cells, these medicines are highly sensitive to changes in the manufacturing process [2]. Thus, quality control measures that suffice for traditional small-molecule drugs and generics do not suffice for biologics.
For many chemically synthesized small-molecule drugs, a few simple chemical tests for identity, purity, and potency may suffice to confirm quality [3, 4]. Such tests can be standardized and shared in the form of public pharmacopeia (e.g., the US Pharmacopeia [USP]) to ensure the consistency of medicines from multiple manufacturers. However, biologics generally require panels of sophisticated and proprietary tests that collectively provide a profile of the approved product’s measurable quality attributes [5, 6].
Extensive characterization data are used to establish proven acceptable ranges (PARs) for quality attributes (Fig. 1) [7]. Quality attributes and their associated specifications can be either quantitative (e.g., high-performance liquid chromatography [HPLC] purity) or qualitative (e.g., gel analysis, color). Quantitative analytical techniques and specification criteria are preferred since data from historical batches can be compared and analyzed statistically to assign PARs. Because quality attributes are measured in a variety of units and scales, we introduce a normalization convention to help visualize control of the multiple attributes (Fig. 1). However, numerous quality attributes cannot be practically and consistently measured using existing analytical technologies. For example, trace amounts of product variants can be difficult to detect and quantify because of their low concentration, and the precise three-dimensional structures of molecules cannot be determined for a mixture of proteins in solution. The control of quality attributes is accomplished via specifications (typically set to ensure the identity, purity, potency, and quality of the product) and PARs for attributes that are not routinely measured with each batch. Thus, testing of biologics is not amenable to the same sort of standardization that is used for testing of small-molecule drugs. Health care providers should understand that quality control for biologics is a dynamic, interactive, and iterative process, which involves quality systems that are internal to each manufacturer and oversight of the product and the manufacturing process by regulatory authorities.
a Quality attributes before and after normalization. Several quality attributes are shown in their native measured units and subsequently converted to normalized units for ease of visualization. b Normalized quality attributes and acceptable ranges for these attributes. General classes of attributes include general properties (e.g., protein concentration, osmolality, pH, appearance, color, and clarity); primary structure (e.g., molecular mass, peptide map under reducing and non-reducing conditions, identity, and extinction coefficient); higher order structure (e.g., spectral measurements by near-ultraviolet circular dichroism, differential scanning calorimetry, and fourier transform infrared spectroscopy); product-related substances (e.g., charged variants and glycan map); impurities (e.g., host cell proteins and DNA and leached chromatography ligand); particles and aggregates; functional attributes (e.g., antibody-dependent cell-mediated toxicity, complement-dependent toxicity, and potency); and stability (e.g., select quality attributes measured over time under normal and stressed conditions). incl. including, LL lower limit, PAR proven acceptable range, UL upper limit range
Many factors can contribute to changes in product quality attributes. Unknown, unintended, or unexplained deviations in process parameters (i.e., drift) [8] and/or known or intended changes in process parameters (i.e., evolution) can result in product quality attributes outside of the historical PAR. However, these changes are unlikely to impact the safety or efficacy of any given biologic.
Drift and evolution may present greater challenges when assessing biosimilars. A biosimilar is any biological product that is highly similar to a reference product, notwithstanding minor differences in clinically inactive components and for which there are no clinically meaningful differences between the biosimilar product and the reference product in terms of the safety, purity, and potency [9]. Biosimilars are considered interchangeable if they can be expected to produce the same clinical result as the reference product in any given patient and, if the product is to be administered more than once, no additional risks are introduced by alternating or switching among products [10]. Two products that were initially deemed biosimilar or interchangeable could each undergo unique patterns of drift and evolution, ultimately resulting in two products that are no longer biosimilar. This process is defined here as divergence. Divergence has important implications for the way in which regulators and health care providers handle safety surveillance, product naming, interchangeability, and medical records. This review summarizes the nature and causes of product drift, evolution, and divergence and the implications of such changes for policy and medical practice.
2 Quality Systems
The US Food and Drug Administration (FDA) and the International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use (ICH) have issued technical regulatory requirements for quality systems [11, 12]. The manufacturer is responsible for establishing a robust quality system to ensure strict control over the manufacturing process and product quality attributes. Recommended elements of quality systems are as follows:
-
Quality system oversight of overall compliance with current good manufacturing practice (cGMP) and internal requirements; includes management responsibilities to provide appropriate resources and ensure proper documentation for changes in manufacturing processes, batch releases, etc.
-
Materials system oversight of control of raw materials needed to manufacture the drug substance and the drug product (glass vials, syringes, etc.).
-
Facilities and equipment system oversight of facility design and controls during routine manufacturing to ensure proper flow of personnel, product, and materials, including waste.
-
Production system oversight of procedures and controls for the manufacture of the drug substance and drug product and process validation.
-
Laboratory control system oversight of quality assurance assays, analytical methods validation, and stability programs.
-
Packaging and labeling system oversight of procedures and controls ensuring that the label aligns with clinical data for the product and that the packaging is clear and legible with no confusion.
All manufacturers, including manufacturers of originator biologics and biosimilars, must have robust quality systems. However, quality systems vary among manufacturers. For example, some manufacturers implement quality systems with minimally required process controls and quality assurance under cGMPs, while others design quality systems that are responsive to information from outside of traditional quality assurance practices. These can include findings from management review of production data, risk management programs, pharmacovigilance signal detection, and information shared by regulators and industry peers.
3 Normal Variability
All manufacturing processes have inherent variability. Given that biologics are sensitive to changes in the manufacturing process, the relationships between the inputs (e.g., raw materials, pressure, and temperature) and outputs (product quality attributes) are studied during development so that acceptable variation (i.e., normal variability [7]) can be established. Subsequently, during routine manufacturing, both the process input parameters and product quality attributes are monitored for adherence within normal variability through control charts. An example of batch-to-batch variability is shown in Fig. 2. As long as variation of quality attributes is within the PARs, physicians can be assured that the variation does not pose a safety or efficacy threat to patients.
Protein concentration in the final product for a monoclonal antibody varied within a normal range relative to the specification limits indicated by the red horizontal lines. The specifications were established on the basis of a combination of data from the historical batches used in clinical studies and structure–function studies relating concentration to the potency of the product. LCL lower control limit, LSL lower specification limit, UCL upper control limit, USL upper specification limit
4 Drift
A recent Product Quality Research Institute (PQRI)–FDA workshop defined process drift as “an unintended, unexplained, or unexpected trend of measured process parameter(s) and/or resulting product attribute(s) away from its intended target value in a time-ordered analysis over the lifetime of a process or product” [13]. Drift can be a systematic trend in one direction or a sudden shift in quality attributes over time (Fig. 3a).
An example of drift is illustrated in Fig. 3b. For the biologic shown, the host cell protein levels (a measure of impurity) were within acceptance limits during conformance batches. However, during subsequent manufacturing, the host cell protein levels slowly started increasing. An investigation showed that the drift was due to interaction between a raw material and process parameters that had not been studied earlier. Following this investigation, controls were tightened for the process parameters, thereby lowering the impurity levels.
5 Product Evolution
Quality attribute(s) can also evolve as a result of deliberate process changes implemented by the manufacturer. Manufacturers have many motivations for considering process changes (e.g., to meet regulator requests and requirements, to implement state-of-the-art technology, to scale up to meet increased demand, or to improve efficiency). Manufacturers also seek to improve the quality, convenience, and functionality of their drug products to meet patient requirements, which may mean improving product purity or developing new formulations, presentations, or devices.
5.1 Management of Product and Process Changes by Manufacturers
Both the FDA and the European Medicines Agency (EMA) have well-established mechanisms to manage post-licensure manufacturing changes [14–16]. Prior to implementing any change, a manufacturer must assess the risk that the change will impact product quality. This assessment is carried out by the internal quality system (i.e., change management) group. The nature of the risk assessment and subsequent characterization/categorization of risk differs among manufacturers. As the risk of impacting quality, safety, and efficacy increases, more data are required to evaluate the impact on product quality.
In general, the preference of manufacturers is to implement changes without shifts in product attributes, and manufacturers are mostly successful in doing so. Many changes are minor and incremental, isolated to a single process step that can be directly evaluated for evidence of any shift in performance. A change in a filter supplier’s manufacturing location with all else remaining identical (filter material, manufacturing process, specifications, etc.) could be deemed a minor change by some manufacturers. In these cases, the manufacturer simply implements the change and notifies the regulators after implementation during the routine annual notification cycle. If a change could potentially impact product quality attribute(s) (e.g., installation of a new like-for-like stainless steel tank), the risk is assessed, and if the lack of impact can be readily demonstrated, the agency is notified, and should the regulator have no objections, the change is then implemented.
More comprehensive changes, such as a change in a key processing step, scale-up of the manufacturing process, or transfer of the entire process to a new manufacturing site, are generally considered to have a higher risk to product quality. Such changes require evaluation of the comparability of the pre-change and post-change products, and the comparability data must be reviewed and approved by a regulatory agency prior to implementation [17]. An experienced organization can generally execute such changes while maintaining product quality within historical trends, such that the analytical comparability exercise is merely confirmatory.
Occasionally, manufacturers implement changes with a high risk of impacting quality, safety, or efficacy, such as a change in a product formulation and/or a change in the production cell line. Shifts in quality attributes might be expected with these changes, whether or not they can be detected analytically. Regulatory agencies may, therefore, require a more comprehensive comparability evaluation. Such an evaluation would include additional analyses of product structure and function beyond routine lot-release tests and may also require non-clinical studies and even clinical studies to confirm lack of impact to safety and efficacy [18]. If a shift in one or a few product quality attributes is anticipated (i.e., product evolution), these shifts are extensively studied, both individually and collectively, for their impact on product safety and/or efficacy [18]. As with the facility site change or scale-up changes, these higher-risk changes require approval from the regulators prior to implementing the changes [18].
Minor incremental changes often do not result in any change in quality attributes. As illustrated in Fig. 4a, b, all of the post-change attributes fall within the previously established ranges. However, although the intention of the manufacturer is to improve the product quality or the process without having an adverse impact on safety and efficacy, manufacturing changes always have the potential to introduce change in one or more quality attribute(s) (Fig. 4c). The manufacturer must then prove to the regulators that the change in the quality attribute(s) has not had an effect on safety and efficacy [18]. Clinical bridging studies, coupled with continued safety monitoring, are used to demonstrate that changes in a few quality attributes (while the rest remain within historical controls) have not had an impact on the safety profile or the efficacy of the product [18].
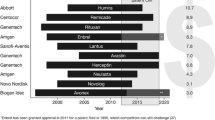
A recent article by Schneider et al. [19] showed a cumulative list of process changes as examples of the high incidence of post-approval changes (e.g., 20 process changes for Enbrel®, 36 for Remicade®, and 18 for Humira®). While the authors cannot comment on the specific process changes listed in the article by Schneider et al., we have conducted a similar analysis for darbepoetin alfa (Aranesp®). Details of changes implemented after marketing authorization can be obtained from the EMA European Public Assessment Reports, and 18 changes to the drug substance, drug product manufacturing process, or final product presentations have been listed for darbepoetin alfa [20]. The majority of these changes were not expected to introduce a shift in quality attributes, but one change implemented in 2008 was associated with a shift in the product isoform distribution (Fig. 5). This shift was also noted in a 2010 publication [21]. This process change was evaluated using clinical bridging studies, and the European Public Assessment Report is available from EMA [22]. This rare event over a 10-year period is an example of the nature and frequency of product evolution. Aside from the one-time shift, variations in the isoform metric for darbepoetin alfa represent normal process variability.
Variation in product attributes of darbepoetin alfa (Aranesp®). The relative quantity of an isoform of darbepoetin alfa is plotted in each lot prior to and after product evolution (left). Using the same counting convention as was used in Schneider et al. [19], 18 darbepoetin alfa variations were approved by the European Medicines Agency in the time period that was examined (right). Only one change was associated with a measurable shift in quality attributes (star). LSL lower specification limit
6 Product Divergence
The preceding sections describe how unplanned deviations in a manufacturing process can contribute to product drift and planned changes can contribute to product evolution, resulting in changes of quality attributes for a given biologic. When robust quality systems and regulatory oversight are in place, a drift that is corrected or evolution should have no adverse impact on the safety and efficacy of the product.
But two biological products that are highly similar to each other at one point in time (i.e., at the time of approval) might not remain similar over time, especially if the products are produced by two different manufacturers. Uncorrected drift by one of the manufacturers and/or evolution of one or both products could result in a cumulative loss of similarity, a process known as product divergence (Fig. 6). Divergence can occur between multiple originator products, an originator and a biosimilar, and ostensibly between multiple biosimilar products, though biosimilars are not expected to be evaluated for similarity to other biosimilars. Divergence should not lead to a change in the safety or efficacy of either product as a stand-alone biologic but could potentially result in clinically meaningful differences between the two products (e.g., potency, safety, or immunogenicity profile). For example:
-
Divergence in potency could result in a difference in optimal dosing for a particular patient. Although both approved products are still effective, switching between the two could cause a disruption in dosing.
-
Divergence in immunogenicity could occur, such that one product is less immunogenic or better tolerated than the other for a given patient, and that patient’s care might be impacted by a switch to the more immunogenic product.
It should be noted that the equivalence window (Fig. 6) is the range of quality attributes established during biosimilar licensure on the basis of a limited number of originator lots. However, PARs are often derived from a larger data set. The ranges for PARs and the equivalence window are derived independently by different manufacturers and will likely vary among manufacturers.
6.1 Examples of Divergence
Divergence is not just a hypothetical phenomenon. In some cases, divergence has even occurred for biologics licensed from an originator company to a partner, where the partner assumes independent regulatory and manufacturing responsibility. Examples include cetuximab and epoetin alfa. Cetuximab is manufactured by separate entities for the US and European markets. Recently, a new indication was approved in Europe on the basis of clinical data from the European-sourced product [23]. The FDA approved the label indication for the US product, while stating that the two products no longer retain equivalent pharmacokinetics [24, 25].
Epoetin alfa is manufactured by separate entities for the US, Japanese, and European markets. The European epoetin alfa underwent formulation and presentation changes in the 1990s, and these changes were associated with safety issues, which resulted in removal of the subcutaneous route of administration from the approved label in Europe [26, 27]. This route of administration was subsequently restored after the sponsor addressed the manufacturing issue. Meanwhile, the corresponding US product did not implement the formulation change and retained the original route of administration on its label.
As these examples show, product quality attributes can diverge as a result of post-marketing manufacturing changes. If such divergence can occur for biologics transferred between licensing partners, where the partners retain some right of reference to the originator’s development data, divergence can certainly occur and is arguably more likely with completely independent entities that have no right of reference to proprietary information collected during development.
7 Impacts of Product Drift, Evolution, and Divergence on Patients and Physicians
The quality systems that govern the detection and management of drift and evolution differ between manufacturers. Currently, there is no mechanism for either regulators or manufacturers to align process changes, quality systems, or life-cycle management systems. Furthermore, regulators are not permitted to share or disclose data received from one manufacturer with another, and manufacturers could be accused of anti-competitive behavior if they shared manufacturing data. Thus, there is no internal or cross-organizational regulatory mechanism to detect and evaluate the impact of divergence. This is not to suggest that new constraints on manufacturing should be imposed by regulators—product drift and evolution are inevitable in biologics manufacturing and, in many cases, process changes represent necessary or desirable improvements that should be encouraged. Rather, policies should take into account the possibility of divergence for multisource biologics.
7.1 Need for Robust Pharmacovigilance Systems
Pharmacovigilance is the system by which drug-related adverse events are tracked over time for marketed products [28]. Ongoing pharmacovigilance is especially important for biologics because of their susceptibility to changes in the manufacturing process and the possibility that drift, evolution, or divergence may have adverse consequences for patients. Therefore, product-specific pharmacovigilance is critical when multiple manufacturers begin supplying related biologics [29].
The FDA stated the following concerning the US biosimilars program:
The FDA process for biosimilars must include product specific safety monitoring. History suggests that pharmaceutical companies will make manufacturing-related changes to biologics periodically throughout their lifecycles, and even small changes could affect safety or efficacy. Tracking adverse events associated with the use of reference and biosimilar products will be difficult if the specific product or manufacturer cannot be readily identified, and appropriate strategies must be developed to ensure the implementation of robust, modern pharmacovigilance programs for biologics [30].
A robust, product-specific pharmacovigilance system for biologics may require special policy measures such as mandatory use of distinguishable names for prescribing. A variety of options exist to ensure that unique product identifiers are captured in medical records, as have been reviewed elsewhere [31]. Policy makers are evaluating the relative merits of requiring prescribing by brand or trade name versus requiring distinguishable non-proprietary names for related biologics.
Furthermore, in a situation where a pharmacist could dispense a different biologic than the one prescribed (i.e., when substitution is permitted), information about the medication actually dispensed should be readily available to the prescriber and reflected in the patient record. To ensure that the prescriber is informed, interoperable electronic health records or a requirement for an after-the-fact communication from the pharmacist to the prescriber may be needed. To address these policy concerns, Europe has taken steps to require product-specific prescribing and record-keeping measures for biologics with the 2010 Pharmacovigilance Directive [32]. In the US, the FDA and individual states are currently considering appropriate policies to help ensure traceability of adverse events [30, 33].
Manufacturers also bear the responsibility to support robust pharmacovigilance for biologics. If a manufacturing problem is causing adverse events, the manufacturer needs to know about it. Pharmacovigilance systems should not merely track the types and severities of adverse events for the purpose of detecting new class-based risks, but should also be statistically robust enough to detect the frequencies of adverse events and to register any increases that occur over time. An accountable manufacturer will couple the pharmacovigilance program to the manufacturing quality system, such that changes in the safety profile of a given product can be quickly detected and investigated.
7.2 Robust Interchangeability Standards
In the US today, only the FDA has the authority to determine on a scientific basis if a biosimilar should be deemed interchangeable with an innovator biologic [34]. The FDA defines an interchangeable biologic as one that “is biosimilar to the reference product, can be expected to produce the same clinical result as the reference product in any given patient, and for a product administered more than once, the safety and reduced efficacy risks of alternating or switching are not greater than with repeated use of the reference product without alternating or switching” [10]. If a product is deemed interchangeable, the product may be substituted by a pharmacist without the intervention of the prescribing physician; however, the authority of a pharmacist to substitute is determined by the state [35].
While approval standards for interchangeability are robust, no regulatory mechanisms are currently in place to ensure continued interchangeability in the event of product drift or product evolution. Thus, products that were interchangeable at the time of approval might continue to be considered interchangeable by regulators even though the quality attributes of the originator and biosimilar products have diverged. Policymakers will need to consider whether there are circumstances where such divergence might impact the interchangeability status of the products and whether mechanisms to prevent or mitigate divergence should be developed. Current sponsor-specific quality systems may not be sufficient to control divergence, as quality systems will likely vary among different manufacturers (see Sect. 2).
7.3 Differences Between Manufacturing Process Changes and Biosimilars
The fundamental difference between manufacturing changes and developing a biosimilar resides in the point of reference for each product. When a manufacturer makes specific changes to its own process, all other aspects of the manufacturing process remain constant. Thus, the impact of a particular change and any product evolution can be readily evaluated [18]. In biosimilar development, almost every aspect of the manufacturing process may have changed, and the only point of reference is the reference drug product. As biological manufacturers do not have access to the originator manufacturing process as a point of reference, comparing the biosimilar product to the reference product is necessarily more complex [18, 30].
Some have argued that interchangeable biologics should be exempt from special pharmacovigilance and questions about long-term interchangeability [36]. A case is made that such policy measures are not required following same-manufacturer process changes, even though the pre-change and post-change products may be concurrently distributed for some period of time and are, therefore, “interchanged” [36]. However, major process changes are rare and episodic and are characterized by a one-time transition from the pre-change to the post-change product. Such time-bound transitions are thus amenable to risk management programs designed to detect changes in the risk-benefit profile of a given product. In contrast, divergence in the risk-benefit profiles between two products may not be readily apparent to either sponsor because competing sponsors do not typically share their manufacturing changes or safety monitoring data. Therefore, it may be appropriate for regulatory authorities to adopt different policy measures in these different situations.
7.4 What a Prescriber Needs to Know
For the reasons described here, prescribers of biologics should be aware of the need for enhanced traceability of these products in patient health records. Because of the high approval standards for biologics and biosimilars in the USA and other well-regulated markets [30, 37], there is a relatively low probability that an issue will be associated with any given manufacturing change or with any given product. Post-approval, regulators and manufacturers can manage residual risks as long as safety data are traceable to the correct manufacturer. In this context, prescribers do not need to be aware of specific manufacturing changes, but they can ensure the best care for their patients and also support public health systems by using distinguishable, product-specific names in patient health records and by being alert to unexpected adverse events. Finally, while interchangeable biologics may be substituted by a pharmacist without the intervention of the prescriber, the prescriber should have timely access to the medication dispensing records. Implementation of electronic health records and evolving state pharmacy practice acts can facilitate such access.
8 Conclusion
Biologics consist of a complex mixture of molecular entities that are characterized by a set of quality attributes. Variability in the quality attributes of biologics is normal, and patients and physicians can be confident in the safety of the product when variability falls within established PARs. Regulatory authorities also examine product variability and assess the potential impact of variability on patients. Regulatory approval is given in light of manufacturer disclosures regarding process variability and because the risk to patients is perceived to be extremely low. Biosimilar manufacturers may use completely different production processes than the manufacturer of the originator biologic and must, therefore, demonstrate to the regulatory authorities that “there are no clinically meaningful differences between the biological product and the reference product in terms of the safety, purity, and potency” [34].
While there may be “no clinically meaningful differences” at the time of approval, uncontrolled deviations in quality attributes or processes (drift) and major manufacturing changes that result in known and measured changes in quality attributes (evolution) may result in divergence of quality attributes between an originator product and a biosimilar. Such divergence may also affect biosimilars that are deemed interchangeable, since quality systems differ between manufacturers and there are no mechanisms in place to ensure continued interchangeability. To prevent risks to patients as a result of divergence, it is essential to establish pharmacovigilance systems, distinguishable product names, robust standards of interchangeability, and procedures for physician and patient notification in the event of substitution of interchangeable biologics.
References
US Food and Drug Administration. What is a biological product? http://www.fda.gov/AboutFDA/Transparency/Basics/ucm194516.htm. Accessed 20 Sept 2013.
Genazzani AA, Biggio G, Caputi AP, Del Tacca M, Drago F, Fantozzi R, Canonico PL. Biosimilar drugs: concerns and opportunities. BioDrugs. 2007;21(6):351–6.
Wiggins JM, Skutnik J, Shimek-Cox J, Schwarzwalder N. The ideal pharmacopeia: a model for the future. Pharm Technol. 2008;32(11):122–5.
Crommelin DJ, Storm G, Verrijk R, de Leede L, Jiskoot W, Hennink WE. Shifting paradigms: biopharmaceuticals versus low molecular weight drugs. Int J Pharm. 2003;266(1–2):3–16.
Chirino AJ, Mire-Sluis A. Characterizing biological products and assessing comparability following manufacturing changes. Nat Biotechnol. 2004;22(11):1383–91. doi:10.1038/nbt1030.
Berkowitz SA, Engen JR, Mazzeo JR, Jones GB. Analytical tools for characterizing biopharmaceuticals and the implications for biosimilars. Nat Rev Drug Discov. 2012;11(7):527–40. doi:10.1038/nrd3746.
Glodek M, Liebowitz S, McCarthy R, McNally G, Oksanen C, Schultz T, Sundararajan M, Vorkapich R, Vukovinsky K, Watts C, Millili G. Process robustness—a PQRI white paper. Pharm Eng. 2006;26(6):1–11.
European Medicines Agency. Concept paper on the revision of the guideline on similar biological medicinal products containing biotechnology-derived proteins as active substance: quality issues. 2011. http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2011/02/WC500102285.pdf. Accessed 20 Sept 2013.
The Patient Protection and Affordable Care Act. 2010. http://www.gpo.gov/fdsys/pkg/BILLS-111hr3590enr/pdf/BILLS-111hr3590enr.pdf. Accessed 27 Jan 2014.
Sherman RE. Biosimilar biological products. Biosimilar guidance webinar. 2012. http://www.fda.gov/downloads/drugs/developmentapprovalprocess/howdrugsaredevelopedandapproved/approvalapplications/therapeuticbiologicapplications/biosimilars/ucm292463.pdf. Accessed 20 Sept 2013.
US Department of Health and Human Services. Guidance for industry quality systems approach to pharmaceutical CGMP regulations. 2006. http://www.fda.gov/downloads/Drugs/.../Guidances/UCM070337.pdf. Accessed 20 Sept 2013.
International Conference on Harmonization of Technical Requirements for Registration of Pharmaceuticals for Human Use. Pharmaceutical quality system: Q10. ICH harmonized tripartite guideline. 2008. http://www.ich.org/fileadmin/Public_Web_Site/ICH_Products/Guidelines/Quality/Q10/Step4/Q10_Guideline.pdf. Accessed 20 Sept 2013.
Szymczak MM, Friedman RL, Uppoor R, Yacobi A. Detection, measurement, and control in pharma manufacturing. Pharm Technol. 2011;70–76.
US Food and Drug Administration. Guidance for industry: changes to an approved application for specified biotechnology and specified synthetic biological products. 1997. http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/ucm124805.pdf. Accessed 20 Sept 2013.
US Food and Drug Administration. Guidance for industry: comparability protocols—chemistry, manufacturing, and controls information. 2003. http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/ucm070545.pdf. Accessed 20 Sept 2013.
European Medicines Agency. Comparability of biotechnological/biological products subject to changes in their manufacturing process. http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2009/09/WC500002805.pdf. Accessed 22 Oct 2013.
Fundamentals of US regulatory affairs, seventh edition. Regulatory Affairs Professionals Society. Maryland: Rockville; 2011.
Lee JF, Litten JB, Grampp G. Comparability and biosimilarity: considerations for the healthcare provider. Curr Med Res Opin. 2012;28(6):1053–8. doi:10.1185/03007995.2012.686902.
Schneider CK. Biosimilars in rheumatology: the wind of change. Ann Rheum Dis. 2013;72(3):315–8. doi:10.1136/annrheumdis-2012-202941.
European Medicines Agency. Aranesp: changes made after 1 September 2003. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Procedural_steps_taken_and_scientific_information_after_authorisation/human/000332/WC500026145.pdf. Accessed 20 Sept 2013.
Schiestl M, Stangler T, Torella C, Cepeljnik T, Toll H, Grau R. Acceptable changes in quality attributes of glycosylated biopharmaceuticals. Nat Biotechnol. 2011;29(4):310–2. doi:10.1038/nbt.1839.
European Medicines Agency. Aranesp: darbepoetin alfa. http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/medicines/000332/human_med_000651.jsp&murl=menus/medicines/. Accessed 22 Oct 2013.
European Medicines Agency. Summary of opinion (post authorization): Erbitux. 2011. http://www.ema.europa.eu/docs/en_GB/document_library/Summary_of_opinion/human/000558/WC500117820.pdf. Accessed 20 Sept 2013.
Erbitux US prescribers information, Updated 2011. http://www.accessdata.fda.gov/drugsatfda_docs/label/2011/125084s153lbl.pdf. Accessed 16 Sept 2013.
Cohen MH, Chen H, Shord S, Fuchs C, He K, Zhao H, Sickafuse S, Keegan P, Pazdur R. Approval summary: cetuximab in combination with cisplatin or carboplatin and 5-fluorouracil for the first-line treatment of patients with recurrent locoregional or metastatic squamous cell head and neck cancer. Oncologist. 2013;18(4):460–6. doi:10.1634/theoncologist.2012-0458.
Casadevall N, Nataf J, Viron B, Kolta A, Kiladjian JJ, Martin-Dupont P, Michaud P, Papo T, Ugo V, Teyssandier I, Varet B, Mayeux P. Pure red-cell aplasia and antierythropoietin antibodies in patients treated with recombinant erythropoietin. N Engl J Med. 2002;346(7):469–75. doi:10.1056/NEJMoa011931.
Locatelli F, Del Vecchio L, Pozzoni P. Pure red-cell aplasia “epidemic”—mystery completely revealed? Perit Dial Int. 2007;27(Suppl 2):S303–7.
US Food and Drug Administration. Guidance for industry: good pharmacovigilance practices and pharmacoepidemiologic assessment. 2005. http://www.fda.gov/downloads/regulatoryinformation/guidances/ucm126834.pdf. Accessed 20 Sept 2013.
Wieser C, Rosenkranz AR. Pure red cell aplasia after treatment of renal anaemia with epoetin theta. Clin Kidney J. 2013;6:539–42.
Kozlowski S, Woodcock J, Midthun K, Sherman RB. Developing the nation’s biosimilars program. N Engl J Med. 2011;365(5):385–8. doi:10.1056/NEJMp1107285.
Casadevall N, Edwards IR, Felix T, Graze PR, Litten JB, Strober BE, Warnock DG. Pharmacovigilance and biosimilars: considerations, needs and challenges. Expert Opin Biol Ther. 2013;13(7):1039–47. doi:10.1517/14712598.2013.783560.
Directive 2010/84/EU of the European Parliament and of the Council of 15 December 2010 amending, as regards pharmacovigilance, directive 2001/83/EC on the Community code relating to medicinal products for human use. Off J Eur Union. 2010;348:74–99.
US Food and Drug Administration. Guidance for industry: scientific considerations in demonstrating biosimilarity to a reference product. http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM291128.pdf. Accessed 22 Oct 2013.
Biologics Price Competition and Innovation Act of 2009; 2010.
Abood RR. Pharmacy practice and the law. 7th ed. Burlington, MA. 2012.
McCamish M, Woollett G. The state of the art in the development of biosimilars. Clin Pharmacol Ther. 2012;91(3):405–17. doi:10.1038/clpt.2011.343.
Weise M, Bielsky MC, De Smet K, Ehmann F, Ekman N, Giezen TJ, Gravanis I, Heim HK, Heinonen E, Ho K, Moreau A, Narayanan G, Kruse NA, Reichmann G, Thorpe R, van Aerts L, Vleminckx C, Wadhwa M, Schneider CK. Biosimilars: what clinicians should know. Blood. 2012;120(26):5111–7. doi:10.1182/blood-2012-04-425744.
Acknowledgments
This study was funded by Amgen Inc. Kerri Hebard-Massey and Micah Robinson (Amgen Inc.) provided medical writing support. Sundar Ramanan and Gustavo Grampp are employees of and stockholders in Amgen Inc.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ramanan, S., Grampp, G. Drift, Evolution, and Divergence in Biologics and Biosimilars Manufacturing. BioDrugs 28, 363–372 (2014). https://doi.org/10.1007/s40259-014-0088-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40259-014-0088-z