Abstract
Epidemiological studies suggest a strong contribution of genetic factors in the pathogenesis of systemic lupus erythematosus (SLE). In the last decades, many risk loci have been identified in several genetic association studies following both candidate gene and genome-wide approaches. The present work was conducted by GAPAID (Genes And Proteins for AutoImmunity Diagnostics) consortium with a dual aim: to replicate the association of several previously reported SLE susceptibility loci in an independent European sample and to explore their relation with some disease subphenotypes. A total of 48 single nucleotide polymorphisms (SNP) from 40 associated loci were typed in a cohort of 208 SLE patients and 152 controls from Rheumatology Units of the University Hospital of Pisa (Italy) and University of Pécs Medical Center (Hungary). Regression analyses were performed to detect disease susceptibility loci and to identify genes affecting specific disease manifestations (renal, neurological, or skin involvement; arthritis; secondary Sjögren syndrome; and secondary antiphospholipid syndrome). Association of previously described risk alleles from HLA locus has been replicated, while IRF5, BLK, ITGAM, and IRF8 loci have been found to be consistent with previous published results. In addition, two new subphenotype-specific associations have been detected: SNP rs5754217 (UBE2L3) with skin involvement and rs3093030 (ICAM1-ICAM4-ICAM5) with hematological disorders. Overall, results from GAPAID project are consistent with previously established associations for HLA, IRF5, BLK, ITGAM, and IRF8 SLE susceptibility loci and report for the first time two subphenotype-specific associations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Systemic lupus erythematosus (SLE) is a complex autoimmune disease affecting multiple organs, characterized by a wide spectrum of clinical manifestations and laboratory findings. Multiple lines of evidence support a strong genetic contribution to the development of the disease, and it is well accepted that SLE occurs in genetically predisposed individuals exposed to certain environmental stimuli. Evidence of familial clustering was the first indication of a genetic susceptibility to SLE. On the basis of twin studies, SLE heritability (that is the relative contribution of genetic variation to the liability of developing the disease) has been estimated to be about 66 % based on the higher monozygotic twins concordance rates (24–56 %) compared to dizygotic twins (2–5 %) [1]. Familial aggregation for SLE, measured by the sibling recurrent risk ratio, varies from 8 to 29 depending upon the disease prevalence in the population used as reference [2].
Several linkage studies and genome-wide association studies have highlighted the impact of genetic polymorphisms on the risk of developing the disease [3–9]. The strong contribution of HLA region is widely known; the risk conferred by DRB1*1501 (HLA-DR2) and DRB1*0301 (HLA-DR3) genes is confirmed in many European populations. Outside the MHC region, IRF5 (interferon regulatory factor 5) is one of the most strongly and consistently SLE-associated loci; STAT4 (signal transducer and activator of transcription 4) has been found to associate with SLE in multiple studies in European or Asian populations [10, 11].
Only a few studies have addressed the influence of disease-predisposing genes on SLE severity and outcome. Fc Rs I, II, and III have been consistently associated with both susceptibility and severity of SLE. In the case of FcgammaRIIa and Fc gammaRIIIa, the low affinity allele is predisposing not only to SLE but also to lupus nephritis [12, 13], while homozygosity for the valine allele of Fc gammaRIIIa is a risk factor for the progression of renal involvement to end-stage renal disease [14]. On the whole, only limited information is available on the association of risk genes for SLE with specific disease phenotypes.
The GAPAID (Genes And Proteins for AutoImmunity Diagnostics) consortium was created within the European Union’s Seventh Framework Programme for Research and Technological Development (FP7), with the aim of developing a novel diagnostic/prognostic platform for patients affected by SLE, based on a genetic array, a serological protein array, and a software combining the clinical data with the genetic and serological information. In this context, the present study describes the genetic study performed on susceptibility to SLE, where 48 single nucleotide polymorphisms (SNP) from 40 different loci have been tested for SLE susceptibility and their association with disease subphenotypes.
Materials and methods
Ethic statement
This study was approved by the Ethics Committee of the University Hospital of Pisa (reference number: 45066/2012) and the Hungarian Scientific and Research Ethics Board (reference number: 24973-1/2012 EKU). The procedures followed were in accordance with the Helsinki Declaration of 1975. All the patients gave written informed consent.
SLE case-control population
A cohort of 208 SLE patients (cases) and 152 healthy blood donors (controls) was recruited between August 2012 and October 2013 from two centers, the Clinical Immunology Unit, Department of Clinical and Experimental Medicine of the University of Pisa (Italy) and the Department of Rheumatology and Immunology of the University of Pécs (Hungary) (Table 1). All SLE patients fulfilled the American College of Rheumatology (ACR) classification [15]. Gender and age data from all individuals were collected, as well as several clinical data retrospectively evaluated from SLE patients such as the age of patients at the onset of the disease, organ involvement, and secondary antiphospholipid syndrome (APS) (Table 1). The occurrence of arthritis (erosive or not) in clinical history was scored. Renal involvement was diagnosed on the basis of proteinuria, hematuria, and/or creatinine increase and/or hypertension and was in most cases (more than 80 % pts) confirmed by kidney biopsy. Hematological involvement was diagnosed in the presence of thrombocytopenia and/or hemolytic anemia and/or leucopenia. Neurological involvement was diagnosed in the presence of neuropsychiatric manifestations such as seizures, psychoses, cerebrovascular disease, and myelopathy. Skin involvement included generalized or malar rash, discoid lesions, and cutaneous vasculitis.
SNP selection and genotyping process
A total of 48 SNPs from 42 loci previously associated with SLE, in European ancestry populations, have been included in GAPAID project (Table 2). Genetic markers were principally selected from candidate gene, genome wide and replication association studies published at the time of the project. Some of the previously reported subphenotype-specific associations regarding those clinical features evaluated in the present study were also considered. The final list included several well known susceptibility loci such as 1q25.1, PTPN22, TNFSF4, STAT4, PXK, BANK1, HLA, TNFAIP3, IRF5, BLK, IRF8, or ITGAM, along with some less studied or controversial ones (e.g., IL10, LY9, IL21, LYN, TRAF6, ICAM region).
DNA from the buffy coat of all collected samples was purified by NucleoSpin 96 Blood Core Kit Macherey-Nagel). DNA quantity (ng/ul) and quality (260/280 and 260/230 absorbances) were checked with Qubit fluorometer and NanoDrop 8000 Spectrophotometer, respectively, before the genotyping process. Genotyping of selected SNP was performed by BioMark™ HD System (Fluidigm), based on the 5’ exonuclease activity of the polymerase. For each array, 2 negative controls and 46 unknown samples were included. Fluidigm SNP Genotyping Analysis Software v.3 was used for allele assignation.
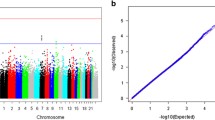
Before statistical analyses, three quality criteria were checked with PLINK v.2.050 software [34]: SNP call rate (min. 95 %), sample call rate (min. 95 %), and conformity of genotype proportions to Hardy-Weinberg equilibrium (HWE) in the overall population.
Statistical analyses
Regression analyses were performed with the abovementioned software with the aim of detecting SLE susceptibility loci (case-control analysis) or specific polymorphisms for any of the measured subphenotypes (case-case analyses). All analyses were carried out under additive, dominant, and recessive genetic models. As differences in age and gender distribution between analyzed populations could limit the results of the study, both factors were included as covariates in all regression analyses. In the same manner, the origin of individuals was also considered as covariate in order to control the possible effect of genetic ancestry in the study. Finally, the results from the case-case analyses for renal, central nervous system (CNS), and skin involvement and presence of arthritis or secondary APS were also adjusted for the age of patients at the onset of the disease. The genetic model with the best P value has been chosen in each case. Corrections for multiple testing implemented in PLINK v.2.050 software have been performed and significant associations were considered when adjusted P values < 0.05.
Results
After the genotyping process, SNPs rs396991 (FCGR3A), rs231775 (CTLA4), rs11568821 (PDCD1), rs6568431 (PRMD1/ATG5), and rs4963128 (PHRF1) were removed for subsequent statistical analyses due to their low call rate (<95 %). The same threshold was applied to remove 9 individuals (5 cases and 4 controls). In addition, SNP rs2187668 (HLA-DQA1) did not fit HWE in the overall population (P value < 0.001). Thus, a total of 42 SNPs and 351 individuals (203 cases and 148 controls) were included in the final case-control and case-case analyses.
Results from the regression analysis focused on the identification of SLE susceptibility loci (case-control analysis) are shown in Table 3. Two SNPs located in the HLA region (rs3131379 and rs1270942) appear significantly associated with the disease (adjusted P value < 0.05). Five additional SNPs in IRF5 (rs729302 and rs2070197), BLK (rs2736340), IRF8 (rs4843869), and ITGAM (rs1143679) loci show also a trend to be related with SLE susceptibility (nominal P value < 0.05).
Two significant subphenotype-specific associations (adjusted P value < 0.05) have been found between SNP rs5754217 (UBE2L3) and skin involvement, and SNP rs3093030 (ICAM1-ICAM4-ICAM5) and hematological manifestations (Table 4). Other 32 suggestive associations have also been observed among all the analyzed clinical features (nominal P value < 0.05).
Discussion
SLE is an autoimmune disease affecting predominantly women characterized by a loss of tolerance to self-antigens, inflammation, and dysregulated immune responses leading to multi-organ damage [35]. Epidemiological studies suggest a strong contribution of genetic factors in the pathogenesis of the disease; many SLE risk loci have been identified in several genome-wide association studies (GWASs) and other association studies in the last decades [36]. In the present study, the strongest association has been detected for HLA region, concordantly with previous GWASs [4, 9]. Encoding more than 200 genes and subdivided into class I, II, and III regions, HLA complex was the first SLE susceptibility locus identified [37]. The two SNPs significantly associated with SLE in this study, rs3131379 and rs1270942, are located in MSH5 and CFB immune genes, respectively, in the class III HLA region. The first one, previously reported as an SLE-associated gene in UK families and also in a study on SLE patients with African American background [38, 39], has recently also been related with cutaneous SLE in European populations [40].
The results found for IRF5, BLK, IRF8, and ITGAM could be also highlighted. Although the association level between these loci and SLE susceptibility does not reach the statistical significance in the present study, probably due to a limited sample size, all of them are well-known SLE susceptibility genes. The three SNPs from IRF5 analyzed here (rs729302, rs2070197, and rs10954213) represent three haplotype blocks with an already described independent effect on SLE risk [41]. Regarding the related IRF8, Cunninghame Graham et al. [19] identified for the first time this gene associated with the disease in a European population, which was later robustly established with the independent effect of the three SNPs analyzed in the present study [8]. There are several studies reporting also the implication of BLK locus in SLE susceptibility, which encodes a tyrosine protein kinase involved in the proliferation, differentiation, and tolerance of B cells. The T allele from SNP rs2736340 has been associated with a major risk of the disease, as detected in the present study [42, 43]. Finally, the non-synonymous variant from ITGAM associated in the present study (rs1143679, R77H) has been proposed as one of the causal variants in this locus affecting the numerous ligand binding activities of ITGAM in monocytes, neutrophils, and dendritic cells and impairing C3-mediated phagocytosis [44, 45].
The analysis of SLE subphenotypes performed in the present study reveals two major findings. The association between UBE2L3 gene and skin involvement is the strongest one. UBE2L3, encoding a ubiquitin conjugating enzyme, was suggested to be a SLE susceptibility locus for European populations by Harley et al. [4] and later confirmed in a large-scale replication study [7]. Both studies showed positive results for the intronic SNP rs5754217 which has been included in a SLE risk haplotype leading to a higher UBE2L3 mRNA expression [46]. Furthermore, T allele of rs5754217 has been associated with the presence of several autoantibodies in African-American and European SLE patients [47, 48], but this is the first study reporting its implication in organ involvement during the disease; this T allele appears to be associated with a higher risk of skin manifestations. The second novel association in the present study is that reported between ICAM1-ICAM4-ICAM5 and hematological disorders. The ICAM locus, encoding intercellular adhesion molecule proteins that are expressed in vascular endothelium, macrophages, lymphocytes, red blood cells, and brain, confers susceptibility to SLE in multiple ancestry populations [31], but no association with disease subphenotypes has been so far reported.
Other several suggestive associations have been observed in this study near to the statistical significance. XKR6 gene, encoding a transmembrane protein of the Kell blood group of antigens and related only to SLE nephritis up to now [28], appears to be linked with CNS involvement. On the contrary, the implication of IL21 with hematological disorders has already been described in Europeans [20]. Other subphenotype-specific tendencies observed here match also previously reported results. Furthermore, the present paper is the first one suggesting some of these associations in European SLE patients, such as the relation between IKZF1 and IRF5 loci and lupus nephritis, IRF8 and hematological disorders, or NCF2 locus and arthritis, all of them already described in Chinese populations [49–52]. However, these new suggestive subphenotype-specific associations with moderate significance values should be taken with caution and replicated in independent populations.
Overall, and despite the possibility of some study design limitations, results from the present study are consistent with previously established associations for the SLE susceptibility loci HLA, IRF5, BLK, ITGAM, and IRF8. The analysis of disease subphenotypes shows new specific associations such as those between UBE2L3 and skin involvement, and ICAM1-ICAM4-ICAM5 and hematological manifestations, in addition to other several suggestive associations which need to be replicated in an independent and larger populations.
References
Deapen D, Escalante A, Weinrib L, Horwitz D, Bachman B, Roy-Burman P, Walker A, Mack TM (1992) A revised estimate of twin concordance in SLE. Arthritis Rheum 35:311–8
Alarcón-Segovia D, Alarcón-Riquelme ME, Cardiel MH, Caeiro F, Massardo L, Villa AR, Pons-Estel BA, Grupo Latinoamericano de Estudio del Lupus Eritematoso (GLADEL) (2005) Familial aggregation of systemic lupus erythematosus, rheumatoid arthritis, and other autoimmune diseases in 1,177 lupus patients from the GLADEL cohort. Arthritis Rheum 52:1138–47
Graham RR, Cotsapas C, Davies L et al (2008) Genetic variants near TNFAIP3 on 6q23 are associated with systemic lupus erythematosus (SLE). Nat Genet 40:1059–61
Harley JB, Alarcón-Riquelme ME, Criswell LA et al (2008) Genome-wide association scan in women with systemic lupus erythematosus identifies susceptibility variants in ITGAM, PXK, KIAA1542 and other loci. Nat Genet 40:204–10
Hom G, Graham RR, Modrek B et al (2008) Association of systemic lupus erythematosus with C8orf13-BLK and ITGAM-ITGAX. N Engl J Med 358:900–9
Kozyrev SV, Abelson AK, Wojcik J et al (2008) Functional variants in the B-cell gene BANK1 are associated with systemic lupus erythematosus. Nat Genet 40:211–6
Gateva V, Sandling JK, Hom G et al (2009) A large-scale replication study identifies TNIP1, PRDM1, JAZF1, UHRF1BP1 and IL10 as risk loci for systemic lupus erythematosus. Nat Genet 41:1228–33
Lessard CJ, Adrianto I, Ice JA et al (2012) Identification of IRF8, TMEM39A, and IKZF3-ZPBP2 as susceptibility loci for systemic lupus erythematosus in a large-scale multiracial replication study. Am J Hum Genet 90:648–60
Armstrong DL, Zidovetzki R, Alarcón-Riquelme ME et al (2014) GWAS identifies novel SLE susceptibility genes and explains the association of the HLA region. Genes Immun 15:347–54
Sestak AL, Fürnrohr BG, Harley JB, Merrill JT, Namjou B (2011) The genetics of systemic lupus erythematosus and implications for targeted therapy. Ann Rheum Dis 70(Suppl 1):i37–43
Deng Y, Tsao BP (2010) Genetic susceptibility to systemic lupus erythematosus in the genomic era. Nat Rev Rheumatol 6:683–92
Karassa FB, Trikalinos TA, Ioannidis JP, FcgammaRIIa-SLE Meta-Analysis Investigators (2002) Role of the Fcgamma receptor IIa polymorphism in susceptibility to systemic lupus erythematosus and lupus nephritis: a meta-analysis. Arthritis Rheum 46:1563–71
Karassa FB, Trikalinos TA, Ioannidis JP, FcgammaRIIa-SLE Meta-Analysis Investigators (2003) The Fc gamma RIIIA-F158 allele is a risk factor for the development of lupus nephritis: a meta-analysis. Kidney Int 63:1475–82
Ramos PS, Brown EE, Kimberly RP, Langefeld CD (2010) Genetic factors predisposing to systemic lupus erythematosus and lupus nephritis. Semin Nephrol 30:164–76
Tan EM, Cohen AS, Fries JF, Masi AT, McShane DJ, Rothfield NF, Schaller JG, Talal N, Winchester RJ (1982) The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 25:1271–7
Willcocks LC, Carr EJ, Niederer HA et al (2010) A defunctioning polymorphism in FCGR2B is associated with protection against malaria but susceptibility to systemic lupus erythematosus. Proc Natl Acad Sci U S A 107:7881–5
Jönsen A, Gunnarsson I, Gullstrand B, Svenungsson E, Bengtsson AA, Nived O, Lundberg IE, Truedsson L, Sturfelt G (2007) Association between SLE nephritis and polymorphic variants of the CRP and FcgammaRIIIa genes. Rheumatology (Oxford) 46:1417–21
Cunninghame-Graham DS, Vyse TJ, Fortin PR et al (2008) Association of LY9 in UK and Canadian SLE families. Genes Immun 9:93–102
Cunninghame Graham DS, Morris DL, Bhangale TR, Criswell LA, Syvänen AC, Rönnblom L, Behrens TW, Graham RR, Vyse TJ (2011) Association of NCF2, IKZF1, IRF8, IFIH1, and TYK2 with systemic lupus erythematosus. PLoS Genet 7, e1002341
Sanchez E, Nadig A, Richardson BC et al (2011) Phenotypic associations of genetic susceptibility loci in systemic lupus erythematosus. Ann Rheum Dis 70:1752–7
Ulker M, Yazisiz V, Sallakci N, Avci AB, Sanlioglu S, Yegin O, Terzioglu E (2009) CTLA-4 gene polymorphism of exon 1(+49 A/G) in Turkish systemic lupus erythematosus patients. Int J Immunogenet 36:245–50
Koldobskaya Y, Ko K, Kumar AA et al (2012) Gene-expression-guided selection of candidate loci and molecular phenotype analyses enhance genetic discovery in systemic lupus erythematosus. Clin Dev Immunol 2012:682018
Prokunina L, Castillejo-López C, Oberg F et al (2002) A regulatory polymorphism in PDCD1 is associated with susceptibility to systemic lupus erythematosus in humans. Nat Genet 32:666–9
Taylor KE, Remmers EF, Lee AT et al (2008) Specificity of the STAT4 genetic association for severe disease manifestations of systemic lupus erythematosus. PLoS Genet 4, e1000084
Sawalha AH, Webb R, Han S et al (2008) Common variants within MECP2 confer risk of systemic lupus erythematosus. PLoS ONE 3, e1727
Musone SL, Taylor KE, Lu TT et al (2008) Multiple polymorphisms in the TNFAIP3 region are independently associated with systemic lupus erythematosus. Nat Genet 40(9):1062–4
Järvinen TM, Hellquist A, Koskenmies S et al (2010) Tyrosine kinase 2 and interferon regulatory factor 5 polymorphisms are associated with discoid and subacute cutaneous lupus erythematosus. Exp Dermatol 19:123–31
Alonso-Perez E, Suarez-Gestal M, Calaza M et al (2012) Further evidence of subphenotype association with systemic lupus erythematosus susceptibility loci: a European cases only study. PLoS ONE 7, e45356
Xu K, Peng H, Zhou M, Wang W, Li R, Zhu KK, Zhang M, Wen PF, Pan HF, Ye DQ (2013) Association study of TRAF1/C5 polymorphism (rs10818488) with susceptibility to rheumatoid arthritis and systemic lupus erythematosus: a meta-analysis. Gene 517:46–54
Sandling JK, Garnier S, Sigurdsson S et al (2011) A candidate gene study of the type I interferon pathway implicates IKBKE and IL8 as risk loci for SLE. Eur J Hum Genet 19(4):479–84
Kim K, Brown EE, Choi CB et al (2012) Variation in the ICAM1-ICAM4-ICAM5 locus is associated with systemic lupus erythematosus susceptibility in multiple ancestries. Ann Rheum Dis 71:1809–14
Sawalha AH, Kaufman KM, Kelly JA et al (2008) Genetic association of interleukin-21 polymorphisms with systemic lupus erythematosus. Ann Rheum Dis 67:458–61
Kaufman KM, Zhao J, Kelly JA et al (2013) Fine mapping of Xq28: both MECP2 and IRAK1 contribute to risk for systemic lupus erythematosus in multiple ancestral groups. Ann Rheum Dis 72:437–44
Purcell S, Neale B, Todd-Brown K et al (2007) PLINK: a tool set for whole-genome association and population-based linkage analyses. Am J Hum Genet 81:559–575
Chung SA, Taylor KE, Graham RR et al (2011) Differential genetic associations for systemic lupus erythematosus based on anti-dsDNA autoantibody production. PLoS Genet 7, e1001323
Rullo OJ, Tsao BP (2013) Recent insights into the genetic basis of systemic lupus erythematosus. Ann Rheum Dis 72(Suppl 2):56–61
Goldberg MA, Arnett FC, Bias WB, Shulman LE (1976) Histocompatibility antigens in systemic lupus erythematosus. Arthritis Rheum 19:129–132
Fernando MM, Freudenberg J, Lee A et al (2012) Transancestral mapping of the MHC region in systemic lupus erythematosus identifies new independent and interacting loci at MSH5, HLA-DPB1 and HLA-G. Ann Rheum Dis 71:777–784
Sanchez E, Comeau ME, Freedman BI et al (2011) Identification of novel genetic susceptibility loci in African American lupus patients in a candidate gene association study. Arthritis Rheum 63:3493–3501
Kunz M, König IR, Schillert A et al (2015) Genome-wide association study identifies new susceptibility loci for cutaneous lupus erythematosus. Exp Dermatol 24(7):510–5
Graham RR, Kyogoku C, Sigurdsson S et al (2007) Three functional variants of IFN regulatory factor 5 (IRF5) define risk and protective haplotypes for human lupus. Proc Natl Acad Sci U S A 104:6758–63
Järvinen TM, Hellquist A, Zucchelli M, Koskenmies S, Panelius J, Hasan T, Julkunen H, D’Amato M, Kere J (2012) Replication of GWAS-identified systemic lupus erythematosus susceptibility genes affirms B-cell receptor pathway signalling and strengthens the role of IRF5 in disease susceptibility in a Northern European population. Rheumatology (Oxford) 51:87–92
Delgado-Vega AM, Dozmorov MG, Quirós MB et al (2012) Fine mapping and conditional analysis identify a new mutation in the autoimmunity susceptibility gene BLK that leads to reduced half-life of the BLK protein. Ann Rheum Dis 71:1219–26
Nath SK, Han S, Kim-Howard X et al (2008) A nonsynonymous functional variant in integrin-alpha(M) (encoded by ITGAM) is associated with systemic lupus erythematosus. Nat Genet 40:152–4
Kim-Howard X, Maiti AK, Anaya JM et al (2010) ITGAM coding variant (rs1143679) influences the risk of renal disease, discoid rash and immunological manifestations in patients with systemic lupus erythematosus with European ancestry. Ann Rheum Dis 69:1329–32
Wang S, Adrianto I, Wiley GB et al (2012) A functional haplotype of UBE2L3 confers risk for systemic lupus erythematosus. Genes Immun 13:380–7
Taylor KE, Chung SA, Graham RR et al (2011) Risk alleles for systemic lupus erythematosus in a large case-control collection and associations with clinical subphenotypes. PLoS Genet 7, e1001311
Agik S, Franek BS, Kumar AA, Kumabe M, Utset TO, Mikolaitis RA, Jolly M, Niewold TB (2012) The autoimmune disease risk allele of UBE2L3 in African American patients with systemic lupus erythematosus: a recessive effect upon subphenotypes. J Rheumatol 39:73-8. J Am Soc Nephrol 25:2859-70.
He CF, Liu YS, Cheng YL et al (2010) TNIP1, SLC15A4, ETS1, RasGRP3 and IKZF1 are associated with clinical features of systemic lupus erythematosus in a Chinese Han population. Lupus 19:1181–6
Qin L, Lv J, Zhou X, Hou P, Yang H, Zhang H (2010) Association of IRF5 gene polymorphisms and lupus nephritis in a Chinese population. Nephrology (Carlton) 15:710–3
Li SW, He Y, Zheng ZH, Liu DW, Liu ZS (2014) Single-nucleotide polymorphisms of IRF8 gene are associated with systemic lupus erythematosus in Chinese Han population. Int J Immunogenet 41:112–8
Yu B, Chen Y, Wu Q et al (2011) The association between single-nucleotide polymorphisms of NCF2 and systemic lupus erythematosus in Chinese mainland population. Clin Rheumatol 30:521–7
Acknowledgments
The authors thank for the technical and human support provided by Sequencing and Genotyping Facilities from SGIker of UPV/EHU. This work was supported by the European Union Seventh Framework Programme FP7/2007-2013 (grant agreement n° 314971).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethic statement
This study was approved by the Ethics Committee of the University Hospital of Pisa (reference number: 45066/2012) and the Hungarian Scientific and Research Ethics Board (reference number: 24973-1/2012 EKU). The procedures followed were in accordance with the Helsinki Declaration of 1975. All the patients gave written informed consent.
Disclosures
None.
Rights and permissions
About this article
Cite this article
Ruiz-Larrañaga, O., Migliorini, P., Uribarri, M. et al. Genetic association study of systemic lupus erythematosus and disease subphenotypes in European populations. Clin Rheumatol 35, 1161–1168 (2016). https://doi.org/10.1007/s10067-016-3235-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-016-3235-8