Abstract
Microparticles (MP) are considered a key component in the haemostatic response. Beyond their in vitro procoagulant properties, a number of pieces of evidence points to procoagulant MP as efficient effectors in the haemostatic response and as pathogenic markers of thrombotic disorders and vascular damage. The aim of the present study was to analyze the procoagulant activity of MP and its correlation with clinical manifestations focusing on vascular involvement in patients with Behçet’s disease (BD). We analyzed 55 BD patients in inactive phase of the disease (26 men; mean age, 35 ± 15 years) of which 19 had previously suffered from thrombosis (deep venous thrombosis in 17 and ischemic stroke in 2), and 73 healthy controls matched for age and sex. Procoagulant MP were assessed by a functional assay. BD patients showed higher procoagulant MP values than controls (22.89 ± 15.74 nM versus 14.47 ± 7.34 nM; p < 0.0001). Conversely, we did not find differences in the levels of procoagulant MP according to the gender of patients (22.22 ± 16.23 nM for men versus 21.46 ± 16.47 for women; p = 0.846) or to previous and current treatments. Moreover, the plasmatic concentration of MP does not define any clinical phenotype and it was not related to the time of evolution of the disease. Although inactive BD patients had high values of procoagulant MP, they did not differentiate between BD patients with or without thrombosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the last 2012 revised international consensus conference nomenclature of vasculitides, Behçet’s disease (BD) has been classified as a variable vessel vasculitis involving both venous and arterial vessels [1]. In fact, venous thrombosis in BD is common with a general prevalence ranging from 14 to 39 % [2].
The etiopathogenesis of BD is not fully understood, but there are evidences that genetic and immunological abnormalities play a role in this condition [3, 4]. In fact, the increased risk to develop BD associated to HLA B51/B5 and the perturbations of T cell homeostasis including the promotion of Th17 responses and the suppression of regulatory T cells have been reported recently [5]. On the other hand, activation of the haemostatic system with increase of procoagulant markers of thrombosis and defective fibrinolysis has also been described [6]. Finally, infections as triggering factor may also play a role in the development of the disease in the genetically predisposed patients [7].
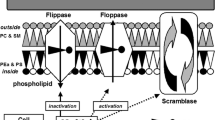
Microparticles (MP) are vesicles with size ranging from 0.1 to 1 μm that are shed from the surface of activated cells such as platelets, endothelial cells, and leukocytes [8]. Recently, it has been postulated that MP have proinflammatory and prothrombotic functions that may affect the course of thrombotic and cardiovascular diseases [9] as well as autoimmune and rheumatic conditions [10]. In fact, increased levels of procoagulant MP have been described in the majority of them and, in the case of systemic lupus erythematosus (SLE) or rheumatoid arthritis, they have been implicated in their pathogenesis [11, 12].
The objective of this study was to analyze the levels of circulating procoagulant MP in a cohort of patients with BD and their relationship with clinical manifestations (mainly to thrombosis), therapy, and time of evolution of the disease.
Patients and methods
Patients
We studied 55 patients with BD (26 men and 29 women). The mean (SD) age at onset of the disease was 27 (12) years (range, 10 to 58). The mean age at diagnosis was 31 (13) years (range, 16 to 62), and the mean age at study inclusion was 35 (15) years (range, 16 to 67). Median follow-up was 36 months (range, 1 to 276).
Patients were recruited in the outpatient clinics of the Department of Autoimmune Diseases, Hospital Clinic, Barcelona, and of the Department of Internal Medicine, Hospital de Bellvitge, l’Hospitalet de Llobregat, Barcelona, two tertiary university hospitals. All patients fulfilled three or more of the International Study Group criteria for the diagnosis of BD [13]. Of note, at the study time, all BD patients were in inactive phase in accordance to Behçet’s Syndrome Activity Score (BSAS) [14]. After informed consent, demographic and clinical data, with particular attention to prior development of thrombosis (arterial or venous), were collected. A total of 19 patients had previously presented episodes of thrombosis (deep venous thrombosis in 17 and ischemic stroke in 2). Thrombotic episodes were assessed by objective methods. Diagnosis of deep venous thrombosis was confirmed by Doppler ultrasonographic scans or by venography. Cerebrovascular ischemic episodes were confirmed by computed tomography scanning or by magnetic resonance imaging techniques. Some of patients of the present series have been included in previous studies [6, 15, 16]. The main cumulative clinical characteristics and previous and current treatments of these patients are described in Table 1.
A sex- and age-matched control group of 73 volunteer healthy subjects (35 men and 38 women; mean age, 34 (14) years, without previous history of thrombotic events, was also recruited.
Blood collection and plasma preparation
Venous blood samples were drawn from a clean antecubital venopuncture without venocclusion in the morning with the patient sitting and resting. Samples for coagulation and fibrinolysis studies were obtained in tubes containing 3.8 % trisodium citrate (1:9, v:v) (Becton Dickinson, Rutherford, NJ, USA), and platelet-free plasma was immediately obtained by double centrifugation: first at 2000g for 10 min at 22 °C and then at 5000g for 10 min at 4 °C. Plasma was aliquoted, snap frozen in a mixture of dry ice:ethanol (1:2, v:v), and stored.
Measurement of procoagulant microparticles
Procoagulant MP were assessed by a functional assay in which MP were captured through annexin V, and then, thrombin was formed by the addition of activated factor X, activated factor V, and prothrombin (ZYMUPHEN MP-Activity, Hyphen BioMed, Neuville, France). Procoagulant MP are expressed as nM phosphatidylserine equivalent.
Statistical analysis
Results are shown as mean ± standard deviation (SD). Comparisons were performed by χ 2 test or analysis of variance (ANOVA). Data were analyzed with the Statistical Package for Social Sciences (SPSS) version 20.0.
Results
Plasmatic levels of procoagulant MP were increased in patients with BD compared to healthy controls (22.89 ± 15.74 nM versus 14.47 ± 7.34 nM; p < 0.0001). There were no differences in the levels of procoagulant MP according to the gender of patients (22.22 ± 16.23 nM for men versus 21.46 ± 16.47 for women; p = 0.846). Notably, we did not find differences according to the clinical manifestations of BD patients, including those patients with and without venous or arterial thrombosis (Table 2). In patients with posterior uveitis and central nervous system involvement, the level of MP was lower than those without this type of severe involvement but without statistical significance (for posterior uveitis, 15.64 ± 11.69 nM versus 24.58 ± 17.29 nM; p = 0.058, and for central nervous system involvement, 13.09 ± 11.39 nM versus 22.88 ± 16.47 nM; p = 0.098).
We also investigated the possible role of treatment in the level of procoagulant MP. Neither previous nor current treatments at the moment of the study were related with differences in the level of MP (Table 2). These results were similar when we analyzed each immunosuppressive treatment separately (data not shown).
Given the data that BD disease activity diminishes with the time evolution [17], we investigated the relationship between the time of evolution of the disease and the mean concentration of MP. We divided the whole series into two groups according to the time from the onset of disease to the time of study: those patients with less than 5 years of evolution and those with more than 5 years of evolution. The level of procoagulant MP was similar between the two groups (20.63 ± 17.00 nM versus 25.64 ± 13.19 nM; p = 0.277). Furthermore, the percentages of patients who received the combination of prednisone and/or immunosuppressive treatment during the evolution or at the moment of the study were similar between the two groups.
Discussion
In the present study, we have confirmed that patients with inactive BD have increased levels of circulating MP. This increase is not related to the gender of patients or to previous or current treatments. Moreover, the levels of procoagulant MP do not define any clinical phenotype and are not related to the time of evolution of the disease.
Circulating levels of MP may reflect the balance between cell stimulation, proliferation, and death. There are some conditions associated with increased levels of MP, mainly thromboembolic and cardiovascular diseases [18]. In fact, some authors have proposed the MP levels as a predictive factor for recurrence thrombosis [19]. Malignancies; normal pregnancy; obesity; hematologic disorders such as aplastic anemia or hemophilia; infectious diseases such as sepsis, malaria, hepatitis C infection, and kidney and liver transplantation; and other conditions such as Alzheimer’s disease, acute respiratory distress syndrome, and schizophrenia are some of the physiological states or diseases in those MP that have been reported to be elevated [9].
In the field of autoimmune diseases, increased levels of circulating MP have been described in patients with SLE [20], Sjögren’s syndrome and rheumatoid arthritis [21], antiphospholipid syndrome [22], systemic sclerosis [23], inflammatory myopathies [24], and vasculitis [25, 26]. Pisetsky et al. [27] have recently reviewed the different functions of circulating MP in these conditions, including modulation of inflammation, endothelial cell activation, and immune complex formation.
In BD, only one previous study has evaluated the level of MP [28]. These authors found significantly increased levels of CD62P+ platelet MP in active and inactive male and female BD patients compared with healthy controls. In addition, percentages of CD62P+ MP were lower in the >50-year age group of BD patients suggesting that activity of the disease is decreasing with age. One limitation of this study is that the authors did not consider the effect of prednisone and immunosuppressive treatment on the levels of circulating MP. In our study, MP were also increased in inactive BD patients compared with healthy controls. However, we did not find differences according to the time evolution of the disease. Regarding the role of current or previous treatment in the level of circulating MP, the small number of patients included in this study made it impossible to draw definitive conclusions considering prednisone, any immunosuppressant, or each one of them separately. Notably, MP in BD patients have not been related with any clinical manifestation, including thrombotic history.
In previous studies, our group has demonstrated increased levels of markers of endothelial damage, such as von Willebrand factor and thrombomodulin, in inactive BD patients [6] and an increased thrombin generation in BD patients with a history of thrombosis [29]. These data, together with those of the present study, may suggest the existence of persistent endothelial dysfunction and an inflammatory process in BD patients, even when they are inactive, and that they may be present for very long time regardless of the immunosuppressive therapy. The prothrombotic nature of circulating MP may also explain the development of thrombotic complications during the course of BD.
The most prominent shortcomings of the present study are its sample size and the fact that there was no control data of BD patients in active phase of the disease. The role of circulating MP as biomarker of activity of BD and their role in the pathogenesis of BD or if they are only an epiphenomenon related to endothelial dysfunction are fields that need to be clarified in the near future.
References
Jennette JC, Falk RJ, Bacon PA et al (2013) 2012 Revised International Chapel Hill consensus conference nomenclature of vasculitides. Arthritis Rheum 65:1–11
Calamia KT, Schirmer M, Melikoglu M (2011) Major vessel involvement in Behçet’s disease: an update. Curr Opin Rheumatol 23:24–31
Hatemi G, Seyahi E, Fresko I, Hamuryudan V (2013) Behçet’s syndrome: a critical digest of the 2012–2013 literature. Clin Exp Rheumatol 31(3 Suppl 77):S108–S117
Pineton de Chambrun M, Wechsler B, Geri G, Cacoub P, Saadoun D (2012) New insights into the pathogenesis of Behçet’s disease. Autoimmun Rev 11:687–698
Na S, Park M, Park S, Lee E (2013) Up-regulation of Th17 and related cytokines in Behçet’s disease corresponding to disease activity. Clin Exp Rheumatol 31(3 Suppl 77):S32–S40
Espinosa G, Font J, Tassies D et al (2002) Vascular involvement in Behcet’s disease: relation with thrombophilic factors, coagulation activation, and thrombomodulin. Am J Med 112:37–43
Mendoza-Pinto C, García-Carrasco M, Jiménez-Hernández M et al (2010) Etiopathogenesis of Behçet’s disease. Autoimmun Rev 9:241–245
Reitsma PH, Versteeg HH, Middeldorp S (2012) Mechanistic view of risk factors for venous thromboembolism. Arterioscler Thromb Vasc Biol 32:563–568
Barteneva NS, Fasler-Kan E, Bernimoulin M et al (2013) Circulating microparticles: square the circle. BMC Cell Biol 14:23
Beyer C, Pisetsky DS (2010) The role of microparticles in the pathogenesis of rheumatic diseases. Nat Rev Rheumatol 6:21–29
Biro E, Nieuwland R, Tak PP et al (2007) Activated complement components and complement activator molecules on the surface of cell-derived microparticles in patients with rheumatoid arthritis and healthy individuals. Ann Rheum Dis 66:1085–1092
Ullal AJ, Reich CF 3rd, Clowse M et al (2011) Microparticles as antigenic targets of antibodies to DNA and nucleosomes in systemic lupus erythematosus. J Autoimmun 36:173–180
(1990) International Study Group for Behcet’s disease. Criteria for diagnosis of Behcet’s disease. Lancet 335:1078–1080
Forbess C, Swearingen C, Yazici Y (2008) Behcet’s Syndrome Activity Score (BSAS): a new disease activity assessment tool, composed of patient-derived measures only, is strongly correlated with the Behcet’s Disease Current Activity Form (BDCAF). Arthritis Rheum 58(S9):S54
Muñoz-Saa I, Cambra A, Pallares L et al (2006) Allelic diversity and affinity variants of MICA are imbalanced in Spanish patients with Behçet’s disease. Scand J Immunol 64:77–82
Espinosa G, Arostegui JI, Plaza S, Rius J, Cervera R, Yague J, Font J (2005) Behçet’s disease and hereditary periodic fever syndromes. Casual association or causal relationship? Clin Exp Rheumatol 23(4 Suppl 38):S64–S66
Saadoun D, Wechsler B, Desseaux K, Le Thi Huong D, Amoura Z, Resche-Rigon M, Cacoub P (2010) Mortality in Behcet’s disease. Arthritis Rheum 62:2806–2812
Enjeti AK, Lincz LF, Seldon M (2008) Microparticles in health and disease. Semin Thromb Hemost 34:683–691
Rectenwald JE, Myers DD Jr, Hawley AE et al (2005) d-dimer, P-selectin, and microparticles: novel markers to predict deep venous thrombosis. a pilot study. Thromb Haemost 94:1312–1317
Parker B, Al-Husain A, Pemberton P et al (2014) Suppression of inflammation reduces endothelial microparticles in active systemic lupus erythematosus. Ann Rheum Dis 73:1144–1150
Sellam J, Proulle V, Jungel A et al (2009) Increased levels of circulating microparticles in primary Sjogren’s syndrome, systemic lupus erythematosus and rheumatoid arthritis and relation with disease activity. Arthritis Res Ther 11:R156
Vikerfors A, Mobarrez F, Bremme K et al (2012) Studies of microparticles in patients with the antiphospholipid syndrome (APS). Lupus 21:802–805
Iversen LV, Ostergaard O, Ullman S et al (2013) Circulating microparticles and plasma levels of soluble E- and P-selectins in patients with systemic sclerosis. Scand J Rheumatol 42:473–482
Baka Z, Senolt L, Vencovsky J, Mann H, Simon PS, Buzás E, Nagy G (2010) Increased serum concentrations of immune cell derived microparticles in polymyositis/dermatomyositis. Immunol Lett 128:124–130
Erdbruegger U, Grossheim M, Hertel B et al (2008) Diagnostic role of endothelial microparticles in vasculitis. Rheumatology 47:1820–1825
Yahata T, Suzuki C, Yoshioka A, Hamaoka A, Ikeda K (2014) Platelet activation dynamics evaluated using platelet-derived microparticles in Kawasaki disease. Circ J 78:188–193
Pisetsky DS, Ullal AJ, Gauley J, Ning TC (2012) Microparticles as mediators and biomarkers of rheumatic disease. Rheumatology 51:1737–1746
Macey M, Hagi-Pavli E, Stewart J, Wallace GR, Stanford M, Shirlaw P, Fortune F (2011) Age, gender and disease-related platelet and neutrophil activation ex vivo in whole blood samples from patients with Behçet’s disease. Rheumatology 50:1849–1859
Mejia JC, Espinosa G, Tassies D, Reverter JC, Cervera R (2014) Endogenous thrombin potential in Behçet’s disease: relationship with thrombosis and anticoagulant therapy. Clin Exp Rheumatol 32(4 Suppl 84):S33–S39
Disclosure
None
Author information
Authors and Affiliations
Corresponding author
Additional information
Juan Carlos Mejía and Thaia Ortiz contributed equally to this work.
Rights and permissions
About this article
Cite this article
Mejía, J.C., Ortiz, T., Tàssies, D. et al. Procoagulant microparticles are increased in patients with Behçet’s disease but do not define a specific subset of clinical manifestations. Clin Rheumatol 35, 695–699 (2016). https://doi.org/10.1007/s10067-015-2903-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-015-2903-4