Abstract
Microparticles (MPs) have been associated with inflammatory and thrombotic disease. High levels of MPs have been identified in patients with systemic lupus erythematosus (SLE) and associated with cardiovascular disease. We analyzed the procoagulant activity of MPs and its correlation with arteriosclerosis and arterial thrombosis in SLE patients. Eighty-seven patients with SLE were included: 22 (25.3%) with associated antiphospholipid syndrome (APS), 32 (36.8%) without antiphospholipid antibodies (aPL) and 33 (37.9%) with aPL but without APS. Subclinical arteriosclerosis, defined as the presence and number of plaques, was evaluated by ultrasonography of carotid arteries. Thrombotic events were confirmed by objective methods. The procoagulant activity of MPs was determined by a functional assay with annexin V. Subclinical arteriosclerosis was found in 19 (21.8%) patients. Thirteen episodes of arterial thrombosis and eight of venous thrombosis were recorded. The procoagulant activity of MPs was greater in patients with arterial thrombosis (17.28 ± 8.29 nM vs 12.96 ± 7.90 nM, p < 0.05). In patients without arterial thrombosis, greater procoagulant activity of MPs was identified in patients with multiple (≥ 2) carotid plaques (17.26 ± 10.63 nM vs 12.78 ± 7.15 nM, p = 0.04). In the multivariate analysis, the procoagulant activity of MPs was independently associated with multiple (≥ 2) carotid plaques and arterial thrombosis [OR = 1.094 (95%CI 1.010–1.185), p = 0.027 and OR = 1.101 (95%CI 1.025–1.182), p = 0.008; respectively]. In conclusion, the procoagulant activity of MPs is associated with arteriosclerosis burden and arterial thrombosis in patients with SLE.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Highlights
-
Systemic lupus erythematosus (SLE) patients have a higher risk of cardiovascular (CV) disease (CVD) compared with the general population, which is not fully explained by traditional CV risk factors.
-
Microparticles (MPs) have been associated with inflammatory and thrombotic disease, so we analyzed the relationship between the procoagulant activity of MPs and CVD in SLE patients.
-
The procoagulant activity of MPs was associated with arteriosclerosis burden and arterial thrombosis in patients with SLE.
-
If the role of MPs as a biomarker of CV risk in SLE patients is confirmed, early arteriosclerosis prophylaxis could be initiated in these patients.
Introduction
Systemic lupus erythematosus (SLE) is the paradigm of the systemic autoimmune diseases. It affects half a million people in Europe and a quarter of a million in the United States [1]. CV involvement is a principal clinical characteristic of SLE. Accelerated subclinical arteriosclerosis occurs in SLE patients [2,3,4], and arteriosclerotic disease follows a pathophysiological continuum whose maximum expression is arterial thrombosis [5]. Carotid ultrasound is the most widely used method for evaluating arteriosclerosis due to its relative low cost and because it is a non-invasive test [4]. This is a validated technique, in which both the carotid intima-media thickness and the presence of carotid plaque measured by ultrasound are considered surrogate markers for arteriosclerosis and are capable of predicting CV events [6]. Carotid ultrasound has been previously used to assess subclinical arteriosclerosis in SLE [2, 3, 7]. In recent years, the concept of arteriosclerotic burden has become very important, since it seems to better predict CV risk than the mere presence of plaque [8] and it has been linked to target organ damage [6, 9]. The concept of arteriosclerotic burden could represent an intermediate point in the aforementioned arteriosclerotic continuum, from the mere presence of single plaque to arterial thrombosis. In this sense, SLE patients also have a higher risk of acute CVD compared with the general population. Coronary artery disease, stroke and peripheral arterial disease are leading causes of death in SLE patients, especially in advanced stages [4, 10]. However, in these patients, CVD is not fully explained by traditional CV risk factors [4, 11], genetic markers [7, 12, 13], or disease-related factors such as the disease duration, treatments received and the chronic inflammatory substrate [14, 15].
Arteriosclerosis is now considered the result of an interaction between different factors, such as traditional CV risk factors, immune-mediated mechanisms, and inflammatory triggers [16]. Likewise, the role of inflammation in thrombosis is very important and terms such as immunothrombosis or thromboinflammation are used to designate this interaction [17].
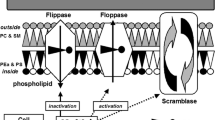
In this scenario of inflammation and vascular damage, the role of circulating MPs has been investigated [18,19,20,21,22]. MPs are small cell membrane vesicles measuring < 1 micron released from cells upon cellular activation and contain proteins and lipids on their surface membrane and nucleic acids inside from the cells which they originated [18]. It has been suggested that MPs represent the link between inflammation, autoimmunity and thrombosis [19, 20]. MPs are involved as modulators in several pathophysiological mechanisms such as endothelial damage [21], chronic inflammation and thrombosis [22]. They participate in the different steps of arteriosclerosis [23], and have also been associated with arterial thrombosis [24]. This evidence has led to MPs being proposed as CV risk biomarkers and even as possible therapeutic targets [22, 23, 25, 26]. Independently of their cellular origin, most MPs have functional procoagulant activity mainly related to the surface expression of phosphatidylserine and/or tissue factor [21, 22, 24,25,26,27]. In SLE patients, an increase in MPs related to increased thrombin generation [28] and endothelial disfunction [29] has been reported in some studies [30,31,32,33] although not in others [31, 33].
Therefore, the aim of the present study was to analyze the procoagulant activity of MPs and its correlation with arteriosclerosis and arterial thrombosis in patients with SLE.
Patients and methods
Patients
Patients with SLE were selected at the outpatient clinic of the Department of Autoimmune Diseases of a tertiary hospital (Hospital Clinic of Barcelona) and consecutively enrolled. All patients fulfilled the 2019 European League Against Rheumatism/American College of Rheumatology (EULAR/ACR) classification criteria for SLE [34]. With the intention of covering the entire spectrum of SLE and avoid confounding factors, three profiles of SLE patients were included: Group 1 (SLE–APS) consisted of patients with SLE who were also diagnosed with antiphospholipid syndrome (APS) according to the Sidney classification criteria [35], including patients with thrombotic and obstetric symptoms. Group 2 (SLE non-aPL) was made up of patients with SLE and persistently negative antiphospholipid antibodies (aPL). Thrombotic events were detected in this group, but in the absence of aPL, they did not meet the APS classification criteria. Group 3 (SLE–aPL) included patients with SLE, and persistently positive aPL who did not experience thrombotic events and therefore could not be classified as APS.
The study was approved by the Clinical Research Ethics Committee of the Hospital Clinic de Barcelona (linked to the University of Barcelona), it was performed according to the principles of the Declaration of Helsinki and informed consent was obtained from all participants.
Variables
Demographic data at SLE diagnosis and study inclusion were collected from the medical record. CV risk factors, considered as previously defined [2], were recorded. Disease duration was defined as the time (in months) from the diagnosis of SLE to study inclusion. Immunosuppressive agents, immunomodulatory therapy, antiplatelet and anticoagulant treatment were recorded. In SLE patients, the activity and chronicity indices were evaluated using the Systemic Lupus Erythematosus Disease Activity Index 2000 (SLEDAI-2K) [36] and the Systemic Lupus International Collaborating Clinics/American College of Rheumatology (SLICC/ACR) Damage Index [37], respectively.
Arteriosclerosis assessment by carotid ultrasound
The study of arteriosclerosis was performed using a carotid ultrasound. The presence of atheroma plaques in this vascular territory was assessed. Carotid ultrasound was performed, according to the protocol of the Hospital Clinic of Barcelona, with a Siemens scanner (Antares model) using a multifrequency duplex Doppler transductor of 7.5–10 MHz for the real time imaging and 3.75 MHz for the Doppler study. All scans were performed by the same sonographer, who had extensive experience with carotid ultrasound. The scanning was performed at right and left carotid territories. Three predetermined segments of the arteries from both sides were examined: the common carotid artery (1 cm proximal to the carotid bulb), the bulb (1–2 cm), and the origin of the internal carotid artery (1 cm distal to the bifurcation). For each location, the sonographer imaged the vessel in longitudinal and transverse planes, with 45° of neck rotation to the contralateral side. The presence and number of plaques were evaluated in each study. Intima-media thickness (IMT) was defined as the distance between the carotid light-intima interface and the media-adventitia interface. Carotid plaque was considered as IMT focal or diffuse thickening with a height ≥ 1.2 mm.
Subclinical arteriosclerosis
Subclinical arteriosclerosis was defined by the presence of one or more plaques at any of the carotid territories explored in the absence of clinical manifestations of arteriosclerotic disease (i.e. cerebrovascular ischemic episodes or myocardial infarctions).
Multiple carotid plaques
To evaluate the arteriosclerosis burden, the number of plaques was taken into account. The existence of ≥ 2 carotid plaques at any of the carotid territories explored was defined as multiple carotid plaques. Multiple carotid plaques as the indicator of arteriosclerosis burden was analyzed only in the group of patients with subclinical arteriosclerosis.
Thrombosis diagnosis
Thrombotic events (cerebrovascular ischemic episodes, myocardial infarctions, deep venous thrombosis and pulmonary embolism) were recorded. The clinical diagnosis was confirmed by objective methods (computed tomography scanning, magnetic resonance imaging, electrocardiographic studies and elevated levels of cardiac enzymes, Doppler ultrasonographic scan, ventilation-perfusion scanning and pulmonary angiography).
Laboratory methods
Blood sampling
Venous blood samples were drawn by clean antecubital venous puncture without venocclusion, in the morning, with the patient sitting and resting. Samples for coagulation and fibrinolysis studies were obtained in tubes containing 3.8% trisodium citrate (1:9, vol:vol) (Becton Dickinson, Rutherford, NJ, USA) and platelet-free plasma was immediately obtained by double centrifugation: first at 2000 g for 10 min at 22 °C, and then at 5000 g for 10 min at 4 °C. Plasma was aliquoted, snap frozen in a mixture of dry ice:ethanol (1:2, vol:vol) and stored at −80 °C.
General hemostasis studies
Prothrombin and activated partial thromboplastin time were determined in an automated analyzer (Siemens, Marburg, Germany) using standard reagents (Siemens) and were expressed as ratios (patient time/control time). Fibrinogen was measured by the Clauss technique.
Antiphospholipid antibodies
Lupus anticoagulant (LAC) was detected according to the Subcommittee on Lupus Anticoagulant/Phospholipid-dependent Antibodies of the International Society on Thrombosis and Haemostasis guidelines [38]. Anticardiolipin (aCL) and anti-ß2 glycoprotein I antibodies were measured using standardized ELISAs (Aesku, Wendelsheim, Germany) and the results were expressed in GPL and MPL units. Titers > 40 GPL or MPL were considered positive for aCL and higher than the 99th percentile of the reference range for anti-ß2 glycoprotein I antibodies, respectively.
Microparticles
The total procoagulant activity of MPs was tested in plasma using a commercial functional assay (Hyphen BioMed, Neuville, France) based on the property of annexin-V, immobilized onto plastic wells, to bind phosphatidylserine (PS) expressed in MPs, as described previously [39]. In brief, plasma samples were placed onto plate microwells coated with streptavidin and biotinylated annexin V. After incubation and washing, bovine factor Xa–Va and human prothrombin were added. After further incubation, the thrombin-specific chromogenic substrate was added. The reaction was stopped with 2% citric acid after 10 min, and absorbance was measured at 405 nm. The results of duplicates were expressed as nanomolar PS equivalent (nM PS eq) by reference to a standard curve. The detection limit of the assay was 0.05 nM, the intra-assay coefficient of variation was 5% and the interassay coefficient of variation was 8%.
Statistical analysis
Data were stored on SPSS (SPSS version 20 for MS Windows statistical package, Chicago, IL, USA) with a unique record per patient. The Student´s t-test or the analysis of variance (ANOVA) test with Bonferroni’s correction were used to compare quantitative variables. The Chi-square test or Fisher's exact test were used to compare qualitative variables. Logistic multivariate regression analyses were carried out using subclinical arteriosclerosis (presence of one or more plaque in the absence of clinical manifestations of arteriosclerotic disease), multiple (≥ 2) carotid plaques and arterial thrombosis as the dependent variables. Variables significantly associated in the multivariate analysis together with other potentially relevant variables were included in the analysis as independent variables. All statistical tests were two-tailed and a value of p < 0.05 was considered statistically significant.
Results
General characteristics
The main characteristics according to the SLE profiles are shown in Table 1. Eighty-seven SLE patients were included: Twenty-two (25.3%) patients were classified as SLE–APS, 32 (36.8%) as SLE non-aPL, and 33 (37.9%) as SLE–aPL patients. Most patients (93.1%) were female and their mean age was 41.1 ± 11.2 years. There was no difference in the prevalence of vascular risk factors (family history of CVD, smoking, obesity, arterial hypertension, diabetes mellitus, hypercholesterolemia, and hypertriglyceridemia) among the three groups.
Subclinical arteriosclerosis was found in 19 (21.8%) patients. Thirteen episodes of arterial thrombosis were recorded: 8 in patients with SLE–APS and 5 in patients with SLE non-aPL. Only one episode of thrombotic microangiopathy was observed (in a SLE–APS patient). Eight episodes of venous thrombosis were detected, all in patients with SLE–APS.
MPs in the whole series
The mean procoagulant activity of MPs in all 87 patients was 13.65 ± 8.08 nM and there was no difference among SLE–APS (15.24 ± 9.07 nM), SLE non-aPL (12.46 ± 5.94 nM), and SLE–aPL (13.76 ± 9.16 nM); p = 0.466. No significant differences were seen in procoagulant MPs according to age, vascular risk factors or aPL positivity.
MPs and subclinical arteriosclerosis
After excluding patients with arterial thrombosis, the procoagulant activity of MPs was analyzed based on the presence or absence of subclinical arteriosclerosis. The main characteristics of these 2 groups of patients are reflected in Table 2. Patients with subclinical arteriosclerosis were older, had a longer time of evolution of the disease, more chronic damage assessed by the SLICC scale and had predominance of some aPL (LAC and IgG aCL).
The procoagulant activity of MPs was 15.35 ± 9.26 nM in SLE patients with subclinical arteriosclerosis and 12.85 ± 7.40 nM in patients without subclinical arteriosclerosis (p = NS) (Fig. 1). The multivariate analysis included demographic characteristics, CV risk factors, clinical manifestations, activity and damage scales (SLEDAI and SLICC), laboratory features, and treatment received. Only age [OR = 1.100 (95%CI 1.040–1.164); p = 0.001] and SLICC [OR = 1.528 (95%CI 1.073–2.178); p = 0.019] were independently associated with subclinical arteriosclerosis.
Procoagulant activity of MPs in SLE patients with subclinical arteriosclerosis, multiple carotid plaques without arterial thrombosis, or arterial thrombosis. Procoagulant activity of MPs (mean ± standard deviation) obtained for the different study subgroups was the following: subclinical arteriosclerosis, presence 15.35 ± 9.26 nM vs absence 12.85 ± 7.40 nM, p = NS; multiple carotid plaques, presence 17.26 ± 10.63 nM vs absence 12.78 ± 7.15 nM, p = 0.04; and arterial thrombosis, presence 17.28 ± 8.29 nM vs absence 12.96 ± 7.90 nM, p < 0.05. The p-value was obtained by Student t-test. The results shown are unadjusted for covariables. Subclinical arteriosclerosis was defined by the presence of one or more plaques at any of the carotid territories explored in the absence of clinical manifestations of arteriosclerotic disease. Multiple carotid plaques was defined by the existence of ≥ 2 plaques at any of the carotid territories explored. The analysis was performed in patients without arterial thrombosis.
MPs and multiple carotid plaques
Subsequently, the association of arteriosclerosis burden with the procoagulant activity of MPs was analyzed, comparing patients with multiple (two or more) carotide plaques versus those with less than two (one or none) carotid plaques. To analyze the relationship of MPs with the arteriosclerosis burden, patients with arterial thrombosis were excluded. The main characteristics of the patients without arterial thrombosis based on the absence or presence of multiple carotid plaques are shown in Table 2. Patients with multiple carotid plaques (and therefore, with a greater arteriosclerosis burden), were older, with a longer evolution time of the disease and had more chronic damage. However, there were no differences in the presence of aPL in both groups.
In SLE patients with multiple carotid plaques, the procoagulant activity of MPs was significantly higher (17.26 ± 10.63 nM vs 12.78 ± 7.15 nM; p = 0.04) (Fig. 1). In the multivariate analysis (performed with the variables described in the previous section), age [OR = 1.121 (95%CI 1.044–1.205); p = 0.002], SLICC [OR = 1.658 (95%CI 1.124–2.445); p = 0.011] and the procoagulant activity of MPs [OR = 1.094 (95%CI 1.010–1.185); p = 0.027] were independently associated with multiple carotid plaques.
MPs and arterial thrombosis
The main characteristics of the patients based on the absence or presence of arterial thrombosis are reflected in Table 3. The patients who suffered arterial thrombosis were older and had less joint involvement, took fewer antimalarials and received anticoagulation more frequently. As it could be predictable, a higher prevalence and burden of arteriosclerosis was seen in patients who had suffered arterial thrombosis (Table 3), which corroborates the arteriosclerotic continuum in the patients of the present study.
The procoagulant activity of MPs was higher in SLE patients with arterial thrombosis than in those without arterial thrombosis (17.28 ± 8.29 nM vs 12.96 ± 7.90 nM; p < 0.05) (Fig. 1). Likewise, in the multivariate analysis (including the variables used in previous sections) arterial thrombosis was independently associated with age [OR = 1.080 (95%CI 1.016–1.148); p = 0.014] and the procoagulant activity of MPs [OR = 1.101 (95%CI 1.025–1.182); p = 0.008].
MPs and other thrombosis
No relationship was found between increased procoagulant activity of MPs and venous thrombosis (17.78 ± 9.75 nM vs 13.24 ± 7.84 nM; p = NS). Since thrombotic microangiopathy was detected in only one patient, we decided not to include it in the analysis.
Discussion
MPs have been associated with endothelial dysfunction [29] and CVD [33] in SLE patients but, to our knowledge, this is the first study to analyze the specific relationship between the procoagulant activity of MPs and the arteriosclerotic disease continuum, from subclinical arteriosclerosis to arterial thrombosis, highlighting the importance of the arteriosclerosis burden. We found that the procoagulant activity of MPs was not statistically different among patients with or without subclinical arteriosclerosis (presence/absence of plaque). However, with the increase in arteriosclerotic burden (patients with multiple carotid plaques and patients with arterial thrombosis) an association with procoagulant activity of MPs was found.
The importance of the arteriosclerosis burden in CV risk assessment has been highlighted in recent years [6, 8, 9, 40] stating that compared to the mere presence of plaque, the measurement of arteriosclerosis burden better assess the CV risk [8]. In line with our results, in a recent study analyzing obesity (another CV risk factor), an association between adiposity and carotid plaque burden, but not with the presence/absence of plaque, has been found. The authors suggested that perhaps adiposity contributes more to development than to the onset of plaque [40]. Other authors have demonstrated in type 1 [6] and type 2 [9] diabetes patients an association between the arteriosclerosis burden and the existence of diabetic retinopathy, a target organ injury associated with an increased risk of developing CVD [6, 9].
Our findings support an association between MPs and arteriosclerosis burden in SLE patients. These results are in line with those obtained in patients without autoimmune diseases. Chironi et al. [41] analyzed subclinical arteriosclerosis by ultrasound of the carotid arteria, abdominal aorta and femoral arteries in 216 asymptomatic subjects included in a CV prevention program and found that leukocyte-derived MPs levels were significantly associated with a higher arteriosclerotic burden, defined by plaque in 2 or 3 sites compared with a single site or no site. Suades et al. [42] analyzed MPs levels in 37 high CV risk-familial hypercholesterolemia patients and compared them with 37 patients with secondary hypercholesterolemia. Levels of procoagulant tissue factor-bearing MPs were higher in high CV risk patients and, among them, MPs levels correlated with the lipid-rich arteriosclerotic plaque burden at the carotid and aortic levels. The fact that MPs were associated with arteriosclerosis burden rather than the mere presence or absence of plaque is intriguing. In our study, presence/absence of plaque was related only with age and chronic damage associated with SLE. Consequently, and in accordance with that suggested by Imahori et al. [40], we can hypothesise that MPs contribute to the process of arteriosclerosis progression more than the process of plaque initiation.
We found an association between the procoagulant activity of MPs and arterial thrombosis in patients with SLE. Only two studies have analyzed the relationship between arterial thrombosis and MPs in patients with SLE, with differing results [31, 33]. López et al. [33] found a significantly higher amount of total MPs in SLE patients with CVD. In contrast, Nielsen et al. [31] reported lower levels of MPs in 70 patients with SLE compared with controls, with a relative increase in annexin V-nonbinding MPs in SLE patients with a history of arterial thrombosis.
The role of MPs in non-autoimmune diseases has been assessed in arterial thrombosis. In 2018, a meta-analysis of 13 studies including 988 patients with ischemic stroke and 985 controls found an association between MPs levels and ischemic stroke, except for lymphocyte-derived MPs where no relationship was found [43]. In another review, an association between endothelial and platelet-derived MPs and stroke was postulated [44]. Additionally, in a meta-analysis of 11 studies, a relationship was found between myocardial infarction and annexin V-positive, endothelial and platelet MPs, but not with leukocyte MPs [45]. This evidence seems to show a clear relationship between MPs and arterial thrombosis [31, 33, 43,44,45], although studies assessing subtypes of MPs related to CVD are not always concordant [43, 45]. This may be explained, in part, by methodological issues. Flow cytometry is the method most frequently used to determine MPs and allows the quantification and determination of their cellular source. Although flow cytometry is considered the gold standard, it has some technical limitations, such as the lack of standardization and concerns about the detection limit for small size MPs that makes its use outside of research laboratories difficult. Functional assays, such as that used in the present study, assess the biological activities (procoagulant in the present assay) independently of their cellular source or size. Functional assays are reproducible and automatable and thus procoagulant MPs may be postulated as a biomarker of atherothrombotic risk [46].
Lastly, the possible value of MPs as a biological therapeutic target for arterial thrombosis or subclinical arteriosclerosis progression in SLE remains to be assessed. A therapeutic regime including drugs such as statins, aspirin or aggressive immunosuppressive therapy, which is known to diminish MPs levels [47,48,49], may be a useful approach in the future.
Strengths and limitations
A strength of the study is that it is the first specific analysis of the relationship between MPs and arteriosclerosis burden in patients with SLE. However, some limitations should be noted. Firstly, the retrospective nature of the study. Secondly, the small number of patients, inherent to the low prevalence of the disease. Thirdly, the use of carotid ultrasound to assess the arteriosclerosis burden. Although it is a validated test, there are subjective aspects in its interpretation, linked to the experience of the sonographer. Finally, the risk of type I error (that is, the existence of "casual" false positives, just by analyzing multiple subgroups) is another limitation that is implicit in a work of this nature where the analysis of different subgroups was essential to eliminate confounding factors.
Future directions
If prospective studies with more patients confirm that the procoagulant activity of MPs could identify SLE patients at greater atherothrombotic risk, their use as a biomarker would enable patients to benefit from early arteriosclerosis prophylaxis.
Conclusions
In conclusion, our results show the procoagulant activity of MPs was associated with the burden of arteriosclerosis and with arterial thrombosis in patients with SLE and, therefore, is related to the CV risk of these patients.
Abbreviations
- MPs:
-
Microparticles
- NS:
-
No significant
- nM PS eq:
-
Nanomolar phosphatidylserine equivalent
References
Bertsias G, Ioannidis JPA, Boletis J et al (2008) EULAR recommendations for the management of systemic lupus erythematosus. Report of a Task Force of the EULAR Standing Committee for International Clinical Studies Including Therapeutics. Ann Rheum Dis 67:195–205. https://doi.org/10.1136/ard.2007.070367
Jiménez S, García-Criado M, Tàssies D et al (2005) Preclinical vascular disease in systemic lupus erythematosus and primary antiphospholipid syndrome. Rheumatology(Oxford) 44:756–761. https://doi.org/10.1093/rheumatology/keh581
Thompson T, Sutton-Tyrrell K, Wildman RP et al (2008) Progression of carotid intima-media thickness and plaque in women with systemic lupus erythematosus. Arthritis Rheum 58:835–842. https://doi.org/10.1002/art.23196
Teixeira V, Tam L-S (2018) Novel insights in systemic lupus erythematosus and atherosclerosis. Front Med 4:262. https://doi.org/10.3389/fmed.2017.00262
Shah PK, Lecis D (2019) Inflammation in atherosclerotic cardiovascular disease. F1000Res. https://doi.org/10.12688/f1000research.18901.1
Carbonell M, Castelblanco E, Valldeperas X et al (2018) Diabetic retinopathy is associated with the presence and burden of subclinical carotid atherosclerosis in type 1 diabetes. Cardiovasc Diabetol 17:66. https://doi.org/10.1186/s12933-018-0706-z
Jiménez S, Tàssies D, Espinosa G et al (2008) Double heterozygosity polymorphisms for platelet glycoproteins Ia/IIa and IIb/IIIa increases arterial thrombosis and arteriosclerosis in patients with the antiphospholipid syndrome or with systemic lupus erythematosus. Ann Rheum Dis 67:835–840. https://doi.org/10.1136/ard.2007.077321
Naqvi TZ, Lee M-S (2014) Carotid intima-media thickness and plaque in cardiovascular risk assessment. JACC Cardiovasc Imaging 7:1025–1038. https://doi.org/10.1016/j.jcmg.2013.11.014
Alonso N, Traveset A, Rubinat E et al (2015) Type 2 diabetes-associated carotid plaque burden is increased in patients with retinopathy compared to those without retinopathy. Cardiovasc Diabetol 14:33. https://doi.org/10.1186/s12933-015-0196-1
Urowitz MB, Bookman AAM, Koehler BE et al (1976) The bimodal mortality pattern of systemic lupus erythematosus. Am J Med 60:221–225. https://doi.org/10.1016/0002-9343(76)90427-7
Esdaile JM, Abrahamowicz M, Grodzicky T et al (2001) Traditional Framingham risk factors fail to fully account for accelerated atherosclerosis in systemic lupus erythematosus. Arthritis Rheum 44:2331–2337. https://doi.org/10.1002/1529-0131(200110)44:10<2331:AID-ART395>3.0.CO;2-I
Tàssies D, Espinosa G, Muñoz-Rodríguez FJ et al (2000) The 4G/5G polymorphism of the type 1 plasminogen activator inhibitor gene and thrombosis in patients with antiphospholipid syndrome. Arthritis Rheum 43:2349–2358. https://doi.org/10.1002/1529-0131(200010)43:10<2349:AID-ANR24>3.0.CO;2-J
Plasín-Rodríguez MA, Rodríguez-Pintó I, Patricio P et al (2018) The H1 haplotype of the endothelial protein C receptor protects against arterial thrombosis in patients with antiphospholipid syndrome. Thromb Res 169:128–134. https://doi.org/10.1016/j.thromres.2018.07.006
Narshi CB, Giles IP, Rahman A (2011) The endothelium: an interface between autoimmunity and atherosclerosis in systemic lupus erythematosus? Lupus 20:5–13. https://doi.org/10.1177/0961203310382429
Schoenfeld SR, Kasturi S, Costenbader KH (2013) The epidemiology of atherosclerotic cardiovascular disease among patients with SLE: a systematic review. Semin Arthritis Rheum 43:77–95. https://doi.org/10.1016/j.semarthrit.2012.12.002
Moriya J (2019) Critical roles of inflammation in atherosclerosis. J Cardiol 73:22–27. https://doi.org/10.1016/j.jjcc.2018.05.010
Jackson SP, Darbousset R, Schoenwaelder SM (2019) Thromboinflammation: challenges of therapeutically targeting coagulation and other host defense mechanisms. Blood 133:906–918. https://doi.org/10.1182/blood-2018-11-882993
Beyer C, Pisetsky DS (2010) The role of microparticles in the pathogenesis of rheumatic diseases. Nat Rev Rheumatol 6:21–29. https://doi.org/10.1038/nrrheum.2009.229
Niccolai E, Emmi G, Squatrito D et al (2015) Microparticles: bridging the gap between autoimmunity and thrombosis. Semin Thromb Hemost 41:413–422. https://doi.org/10.1055/s-0035-1549850
Cunningham M, Marks N, Barnado A et al (2014) Are microparticles the missing link between thrombosis and autoimmune diseases? involvement in selected rheumatologic diseases. Semin Thromb Hemost 40:675–681
Tushuizen ME, Diamant M, Sturk A, Nieuwland R (2011) Cell-derived microparticles in the pathogenesis of cardiovascular disease: friend or foe? Arterioscler Thromb Vasc Biol 31:4–9. https://doi.org/10.1161/ATVBAHA.109.200998
Voukalis C, Shantsila E, Lip GYH (2019) Microparticles and cardiovascular diseases. Ann Med 51:193–223. https://doi.org/10.1080/07853890.2019.1609076
Rautou PE, Vion AC, Amabile N et al (2011) Microparticles, vascular function, and atherothrombosis. Circ Res 109:593–606. https://doi.org/10.1161/CIRCRESAHA.110.233163
Świtońska M, Słomka A, Sinkiewicz W, Zekanowska E (2015) Tissue-factor-bearing microparticles (MPs-TF) in patients with acute ischaemic stroke: The influence of stroke treatment on MPs-TF generation. Eur J Neurol 22:395–401. https://doi.org/10.1111/ene.12591
Thulin Å, Christersson C, Alfredsson J, Siegbahn A (2016) Circulating cell-derived microparticles as biomarkers in cardiovascular disease. Biomark Med 10:1009–1022. https://doi.org/10.2217/bmm-2016-0035
Montoro-García S, Orenes-Piñero E, Marín F et al (2012) Pharmacological modulation of microparticle release: new strategies for the management of atherothrombotic vascular disorders. Curr Pharm Des 18:840–849. https://doi.org/10.2174/138161212799277789
Versteeg HH, Heemskerk JWM, Levi M, Reitsma PH (2013) New fundamentals in hemostasis. Physiol Rev 93:327–358. https://doi.org/10.1152/physrev.00016.2011
Pereira J, Alfaro G, Goycoolea M et al (2006) Circulating platelet-derived microparticles in systemic lupus erythematosus. Thromb Haemost 95:94–99
McCarthy EM, Wilkinson FL, Parker B, Alexander MY (2016) Endothelial microparticles: pathogenic or passive players in endothelial dysfunction in autoimmune rheumatic diseases? Vascul Pharmacol 86:71–76. https://doi.org/10.1016/j.vph.2016.05.016
Sellam J, Proulle V, Jüngel A et al (2009) Increased levels of circulating microparticles in primary Sjögren’s syndrome, systemic lupus erythematosus and rheumatoid arthritis and relation with disease activity. Arthritis Res Ther 11:R156. https://doi.org/10.1186/ar2833
Nielsen CT, Østergaard O, Johnsen C et al (2011) Distinct features of circulating microparticles and their relationship to clinical manifestations in systemic lupus erythematosus. Arthritis Rheum 63:3067–3077. https://doi.org/10.1002/art.30499
Nielsen CT, Østergaard O, Rekvig OP et al (2015) Galectin-3 binding protein links circulating microparticles with electron dense glomerular deposits in lupus nephritis. Lupus 24:1150–1160. https://doi.org/10.1177/0961203315580146
López P, Rodríguez-Carrio J, Martínez-Zapico A et al (2017) Circulating microparticle subpopulations in systemic lupus erythematosus are affected by disease activity. Int J Cardiol 236:138–144. https://doi.org/10.1016/j.ijcard.2017.02.107
Aringer M, Costenbader K, Daikh D et al (2019) 2019 European League Against Rheumatism/American College of Rheumatology classification criteria for systemic lupus erythematosus. Ann Rheum Dis. https://doi.org/10.1136/annrheumdis-2018-214819
Miyakis S, Lockshin MD, Atsumi T et al (2006) International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). J Thromb Haemost 4:295–306. https://doi.org/10.1111/j.1538-7836.2006.01753.x
Gladman DD, Ibañez D, Urowitz MB (2002) Systemic lupus erythematosus disease activity index 2000. J Rheumatol 29:288–291
Gladman D, Ginzler E, Goldsmith C et al (1996) The development and initial validation of the Systemic Lupus International Collaborating Clinics/American College of Rheumatology damage index for systemic lupus erythematosus. Arthritis Rheum 39:363–369. https://doi.org/10.1002/art.1780390303
Pengo V, Tripodi A, Reber G et al (2009) Update of the guidelines for lupus anticoagulant detection. J Thromb Haemost 7:1737–1740. https://doi.org/10.1111/j.1538-7836.2009.03555.x
Martínez-Zamora MA, Tàssies D, Creus M et al (2016) Higher levels of procoagulant microparticles in women with recurrent miscarriage are not associated with antiphospholipid antibodies. Hum Reprod 31:46–52. https://doi.org/10.1093/humrep/dev278
Imahori Y, Mathiesen EB, Leon DA et al (2018) The contribution of obesity to carotid atherosclerotic plaque burden in a general population sample in Norway: the Tromsø Study. Atherosclerosis 273:15–20. https://doi.org/10.1016/j.atherosclerosis.2018.04.014
Chironi G, Simon A, Hugel B et al (2006) Circulating leukocyte-derived microparticles predict subclinical atherosclerosis burden in asymptomatic subjects. Arterioscler Thromb Vasc Biol 26:2775–2780. https://doi.org/10.1161/01.ATV.0000249639.36915.04
Suades R, Padró T, Alonso R et al (2015) High levels of TSP1+/CD142+ platelet-derived microparticles characterise young patients with high cardiovascular risk and subclinical atherosclerosis. Thromb Haemost 114:1310–1321. https://doi.org/10.1160/TH15-04-0325
Wang B, Cai W, Zhang Z et al (2018) Circulating microparticles in patients after ischemic stroke: a systematic review and meta-analysis. Rev Neurosci. https://doi.org/10.1515/revneuro-2017-0105
El-Gamal H, Parray AS, Mir FA et al (2019) Circulating microparticles as biomarkers of stroke: a focus on the value of endothelial- and platelet-derived microparticles. J Cell Physiol 234:16739–16754. https://doi.org/10.1002/jcp.28499
Wang Z, Cai W, Hu S et al (2017) A meta-analysis of circulating microvesicles in patients with myocardial infarction. Arq Bras Cardiol 109:156–164. https://doi.org/10.5935/abc.20170102
Campello E, Spiezia L, Radu CM et al (2014) Evaluation of a procoagulant phospholipid functional assay as a routine test for measuring circulating microparticle activity. Blood Coagul Fibrinolysis 25:534–537. https://doi.org/10.1097/MBC.0000000000000068
Suades R, Padró T, Alonso R et al (2013) Lipid-lowering therapy with statins reduces microparticle shedding from endothelium, platelets and inflammatory cells. Thromb Haemost 110:366–377. https://doi.org/10.1160/TH13-03-0238
Bulut D, Becker V, Mügge A (2011) Acetylsalicylate reduces endothelial and platelet-derived microparticles in patients with coronary artery disease. Can J Physiol Pharmacol 89:239–244. https://doi.org/10.1139/y11-013
Parker B, Al-Husain A, Pemberton P et al (2014) Suppression of inflammation reduces endothelial microparticles in active systemic lupus erythematosus. Ann Rheum Dis 73:1144–1150. https://doi.org/10.1136/annrheumdis-2012-203028
Funding
This study was supported in part by Grant Nos. FIS 11/00977 and 05/0204 from the “Instituto de Salud Carlos III (ISCIII)”.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no competing interests.
Ethics approval
The study was approved by the Clinical Research Ethics Committee of the Hospital Clinic de Barcelona (linked to the University of Barcelona), it was performed according to the principles of the Declaration of Helsinki.
Informed consent
Informed consent was obtained from all participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Plasín-Rodríguez, M.A., Patricio, P., Monteagudo, J. et al. Procoagulant microparticles are associated with arterial disease in patients with systemic lupus erythematosus. J Thromb Thrombolysis 52, 30–41 (2021). https://doi.org/10.1007/s11239-020-02295-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-020-02295-1